Which component of blood is primarily responsible for transporting oxygen?
Plasma
White blood cells
Red blood cells
Platelets


Blood, the life-sustaining fluid coursing through our veins, serves as the body’s primary transport system. It delivers essential nutrients and oxygen to cells, while removing waste products and carbon dioxide. This vital fluid also plays a crucial role in immune defense, clotting, and maintaining homeostasis. In this article, we will explore the composition, functions, and importance of blood, shedding light on its integral role in maintaining human health and vitality.
Blood is a specialized bodily fluid that performs essential functions to sustain life. It circulates through the body’s cardiovascular system, delivering vital substances and removing waste products. Here are the primary components and functions of blood
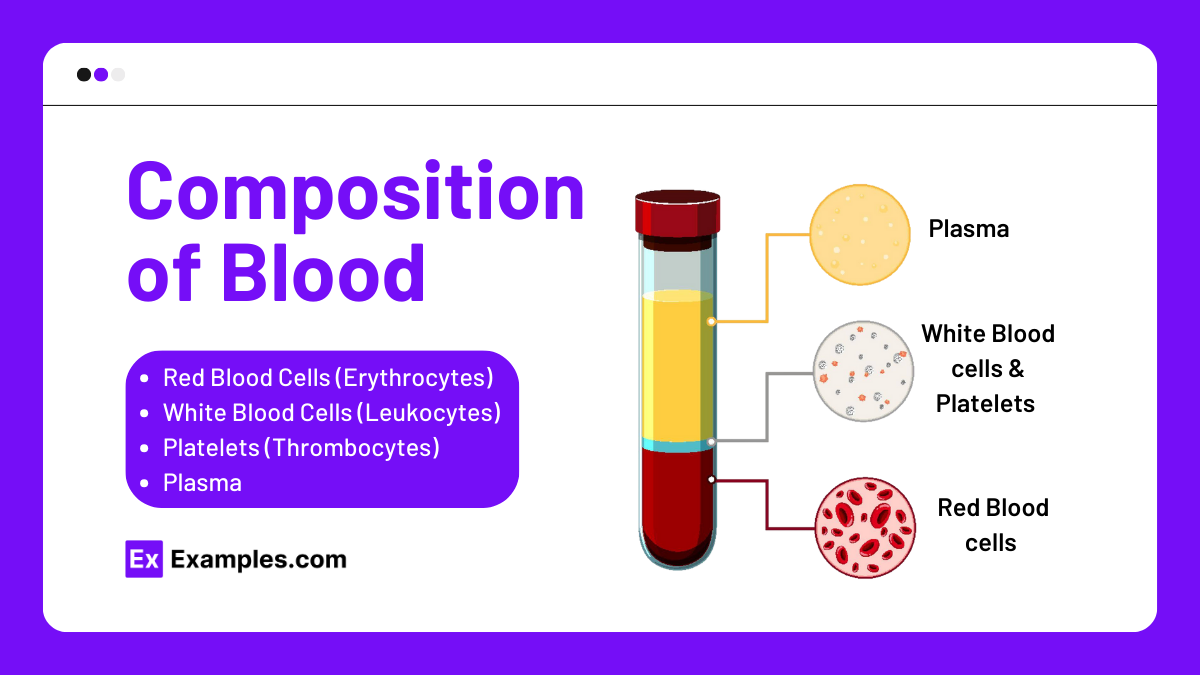
Blood is composed of four main components: red blood cells, white blood cells, platelets, and plasma. Each component plays a unique and essential role in maintaining the body’s health and functionality.
Structure and Function: Red blood cells are biconcave, disc-shaped cells that lack a nucleus. Their primary function is to transport oxygen from the lungs to the body’s tissues and return carbon dioxide from the tissues to the lungs. Hemoglobin, a protein within red blood cells, binds to oxygen and facilitates this transportation.
Production: Red blood cells are produced in the bone marrow through a process called erythropoiesis. This process is regulated by erythropoietin, a hormone produced by the kidneys in response to low oxygen levels.
Lifespan: The average lifespan of a red blood cell is about 120 days. Old or damaged red blood cells are removed from circulation by the spleen and liver.
Types and Functions: White blood cells are crucial for the immune system. They protect the body against infections and foreign invaders. There are several types of white blood cells, each with specific functions:
Lifespan: The lifespan of white blood cells varies greatly depending on the type. Some may live for a few hours to a few days, while others, like memory T cells, can live for years.
Structure and Function: Platelets are small, disc-shaped cell fragments without a nucleus. Their primary function is to prevent bleeding by forming blood clots. When a blood vessel is injured, platelets adhere to the site, aggregate, and work with clotting factors to form a stable clot that seals the wound.
Production: Platelets are produced in the bone marrow from large cells called megakaryocytes. Each megakaryocyte can release thousands of platelets into the bloodstream.
Lifespan: Platelets have a relatively short lifespan of about 7-10 days. They are continuously replenished by the bone marrow.
Composition and Function: Plasma is the liquid component of blood, making up about 55% of its total volume. It is primarily composed of water (about 90%) but also contains proteins, electrolytes, hormones, nutrients, and waste products.
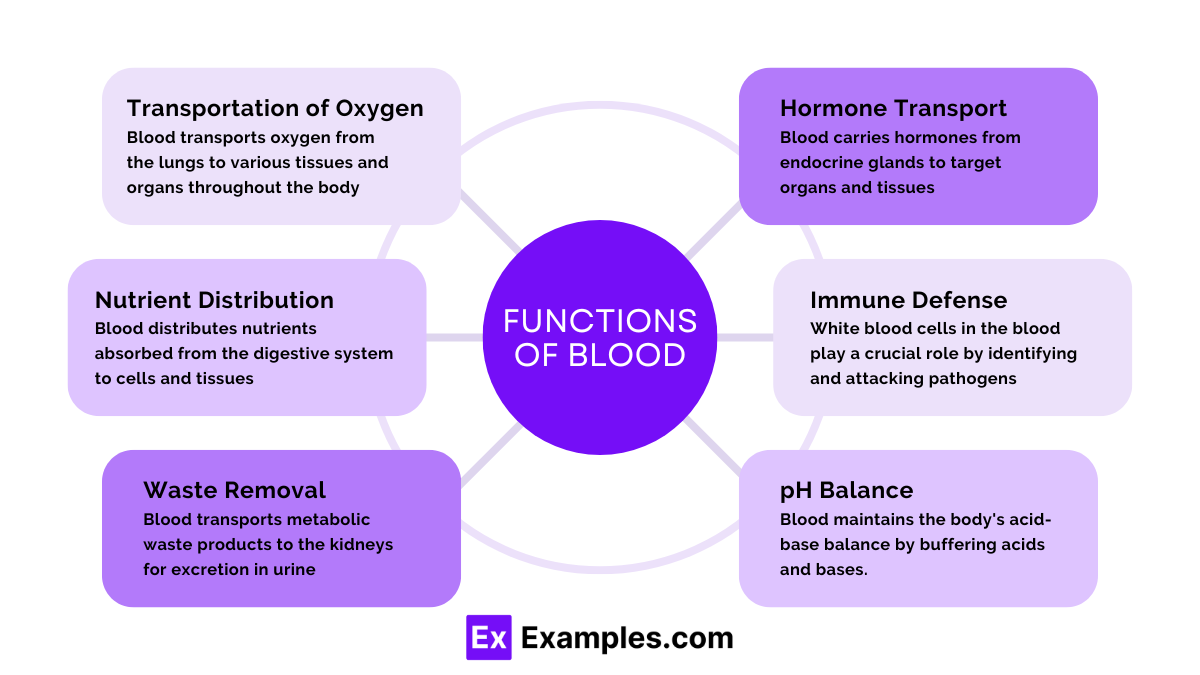
Blood transports oxygen from the lungs to various tissues and organs throughout the body. Hemoglobin in red blood cells binds to oxygen molecules and releases them where needed.
Blood carries carbon dioxide, a waste product of metabolism, from the tissues to the lungs for exhalation. This helps maintain the body’s pH balance.
Blood distributes nutrients absorbed from the digestive system to cells and tissues. These nutrients include glucose, amino acids, fatty acids, and vitamins.
Blood transports metabolic waste products, such as urea and creatinine, to the kidneys for excretion in urine, thus preventing toxic accumulation.
Blood helps regulate body temperature by distributing heat generated by metabolic processes throughout the body and to the skin for dissipation.
Blood carries hormones from endocrine glands to target organs and tissues, facilitating communication and regulation of various bodily functions.
White blood cells in the blood play a crucial role in the immune response by identifying and attacking pathogens, such as bacteria and viruses, and producing antibodies.
Blood contains platelets and clotting factors that initiate the clotting process, preventing excessive blood loss from injuries and promoting wound healing.
Blood maintains the body’s acid-base balance by buffering acids and bases. This is crucial for normal cellular function and enzyme activity.
Blood helps regulate the body’s fluid balance by absorbing and distributing water, ensuring that cells and tissues remain hydrated.
In addition to oxygen and carbon dioxide, blood transports other gases like nitric oxide, which plays a role in vascular dilation and blood pressure regulation.
Blood serves as a reservoir for nutrients such as glucose and lipids, which can be mobilized during periods of fasting or increased demand.
Blood maintains the balance of electrolytes such as sodium, potassium, and calcium, which are essential for nerve function, muscle contraction, and cellular activities.
Blood detoxifies harmful substances by transporting them to the liver for detoxification and subsequent excretion.
Blood provides the necessary substrates for cellular metabolism and removes the byproducts of metabolic processes, ensuring efficient energy production and use.
Blood formation, or hematopoiesis, is a complex process by which blood cells are produced in the body. This essential biological process occurs primarily in the bone marrow, but it also involves the liver and spleen, particularly during fetal development. The following sections explain the stages and mechanisms involved in the formation of blood.
| Blood Cell Type | Progenitor Cells | Mature Cells |
|---|---|---|
| Erythrocytes | Proerythroblast | Erythrocyte (Red Blood Cell) |
| Platelets | Megakaryoblast | Thrombocyte (Platelet) |
| Neutrophils | Myeloblast | Neutrophil |
| Eosinophils | Myeloblast | Eosinophil |
| Basophils | Myeloblast | Basophil |
| Monocytes | Monoblast | Monocyte |
| Lymphocytes | Lymphoblast | B-Cell, T-Cell, NK Cell |
Blood types are classifications of blood based on the presence or absence of specific antigens on the surface of red blood cells. These antigens can trigger an immune response if they are foreign to the body. Understanding blood types is crucial for safe blood transfusions, organ transplants, and understanding certain medical conditions.
The ABO blood group system is the most important blood type system in human blood transfusion. It is determined by the presence or absence of two antigens, A and B, on the surface of red blood cells.
The Rh blood group system is the second most significant blood type classification. It is based on the presence or absence of the Rh antigen (also known as the D antigen).
Combining the ABO and Rh systems, we get the following blood types: A+, A-, B+, B-, AB+, AB-, O+, and O-.
Blood Transfusions
Organ Transplants
Blood type compatibility is also crucial in organ transplants. An incompatible blood type can lead to organ rejection.
Blood type distribution varies among different populations and ethnic groups. Here is a general distribution of blood types in the United States:
| Blood Type | Percentage (%) |
|---|---|
| O+ | 37.4 |
| O- | 6.6 |
| A+ | 26.3 |
| A- | 5.7 |
| B+ | 8.5 |
| B- | 1.5 |
| AB+ | 3.4 |
| AB- | 0.6 |
Red Coloration
Human blood is red, but the shade can vary:
The red color of blood is due to the presence of hemoglobin, a protein in red blood cells. Hemoglobin contains iron, which binds to oxygen. The iron-oxygen complex absorbs and reflects light in a way that gives blood its red color.
Hemoglobin is composed of four subunits, each containing an iron atom embedded in a heme group. When oxygen binds to the iron in hemoglobin, it causes a change in the shape of the hemoglobin molecule, which alters its light absorption properties. This change in light absorption is what causes oxygenated hemoglobin to appear bright red.
The color of blood varies across the animal kingdom due to differences in the respiratory pigments used to transport oxygen.
Certain medical conditions can cause changes in blood color:
Temperature regulation is a crucial physiological process that helps maintain the body’s core temperature within a narrow, optimal range, typically around 37°C (98.6°F). Blood plays a vital role in this thermoregulation through several mechanisms.
| Disorder | Affected Blood Component | Symptoms | Causes |
|---|---|---|---|
| Iron-Deficiency Anemia | Red Blood Cells | Fatigue, weakness, pale skin | Lack of iron |
| Sickle Cell Disease | Red Blood Cells | Pain, potential organ damage | Genetic mutation |
| Acute Lymphocytic Leukemia | White Blood Cells | Fever, fatigue, frequent infections | Unknown, genetic factors |
| Hodgkin Lymphoma | White Blood Cells | Swollen lymph nodes, night sweats | Genetic mutations, Epstein-Barr virus |
| Immune Thrombocytopenia | Platelets | Easy bruising, excessive bleeding | Autoimmune response |
| Hemophilia A | Platelets (clotting factor) | Excessive bleeding, joint pain | Genetic mutation (factor VIII deficiency) |
| Von Willebrand Disease | Platelets (clotting factor) | Prolonged bleeding, nosebleeds | Genetic mutation |
Blood is a vital fluid that circulates through the body, delivering oxygen and nutrients to cells and removing waste products.
Blood consists of red blood cells, white blood cells, platelets, and plasma.
Red blood cells transport oxygen from the lungs to the rest of the body and carry carbon dioxide back to the lungs for exhalation.
White blood cells are crucial for the immune system, protecting the body against infections and foreign invaders.
Platelets help with blood clotting, preventing excessive bleeding when injuries occur.
Plasma is the liquid component of blood, containing water, salts, enzymes, antibodies, and other proteins.
Blood cells are produced in the bone marrow, a spongy tissue inside bones.
Anemia is a condition where there is a deficiency of red blood cells or hemoglobin, leading to fatigue and weakness.
High blood pressure can be caused by genetics, poor diet, lack of exercise, and stress.
Maintain healthy blood by eating a balanced diet, staying hydrated, exercising regularly, and avoiding smoking.
Text prompt
Add Tone
10 Examples of Public speaking
20 Examples of Gas lighting
Which component of blood is primarily responsible for transporting oxygen?
Plasma
White blood cells
Red blood cells
Platelets
What is the main function of white blood cells?
Transporting nutrients
Fighting infections
Clotting blood
Carrying carbon dioxide
Which part of the blood helps in clotting?
Plasma
Red blood cells
White blood cells
Platelets
Plasma, the liquid component of blood, is primarily made up of:
Proteins
Water
Glucose
Red blood cells
Which protein in red blood cells binds to oxygen?
Fibrinogen
Albumin
Hemoglobin
Globulin
What is the average lifespan of a red blood cell?
10 days
30 days
60 days
120 days
Which of the following blood types is known as the universal donor?
A+
B-
AB+
O-
Which of the following is not a function of blood?
Transporting oxygen
Regulating body temperature
Producing hormones
Removing waste products
Which condition is characterized by a deficiency of red blood cells or hemoglobin?
Leukemia
Hemophilia
Thrombosis
Anemia
What type of blood cells are involved in the immune response?
Red blood cells
Platelets
White blood cells
Erythrocytes
Before you leave, take our quick quiz to enhance your learning!

