What is the primary role of B cells in humoral immunity?
To directly destroy pathogens
To produce antibodies
To present antigens to T cells
To enhance phagocytosis

Humoral immunity represents a critical aspect of the adaptive immune system, primarily mediated by antibodies produced by B cells. This type of immunity is key in defending against pathogens circulating in bodily fluids, such as bacteria and viruses. The term “humoral” refers to the humors, or bodily fluids, and is rooted in classical medicine, which believed that health stemmed from a balance among the body’s fluids.
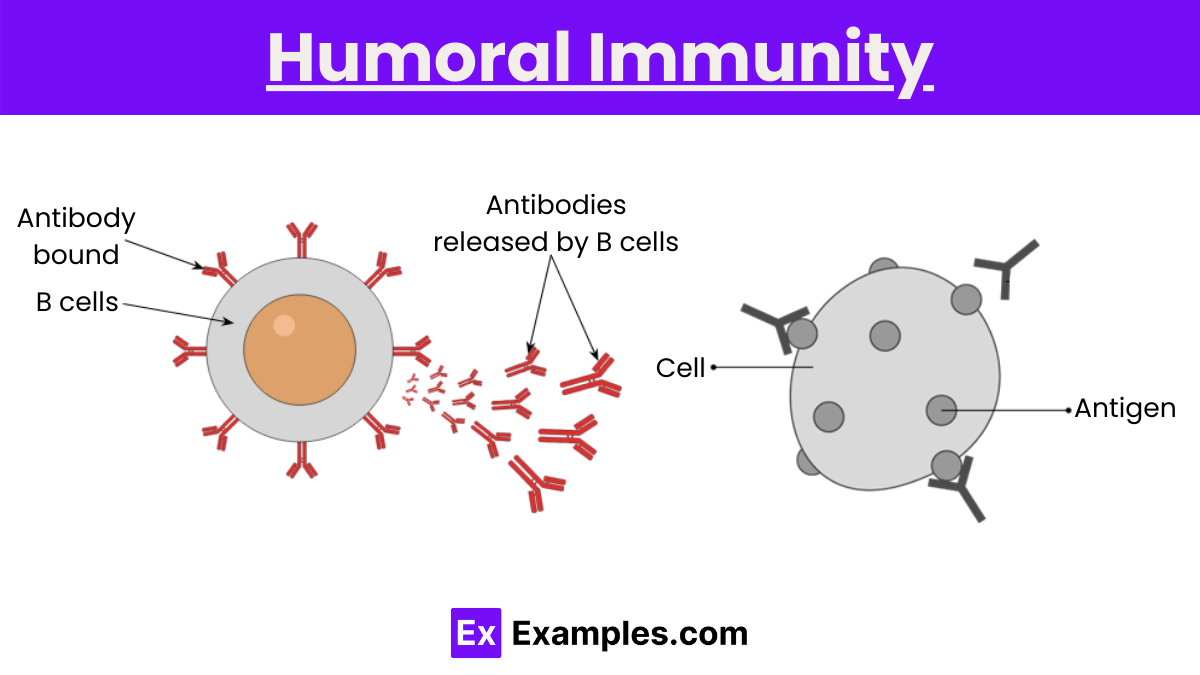
Humoral immunity involves the production of antibodies that fight against pathogens. These antibodies are specific proteins capable of identifying and neutralizing foreign objects like bacteria, viruses, and toxins. The process starts when an invader (antigen) triggers the immune response. B cells, a type of white blood cell, play a pivotal role in this defense mechanism.
The initial step in humoral immunity begins when an antigen, typically a protein or polysaccharide on the surface of a pathogen such as a virus or bacterium, enters the body. These antigens are foreign to the host and trigger the immune response.
Antigens are captured by antigen-presenting cells (APCs), such as dendritic cells or macrophages. These cells process the antigen and then present its fragments on their surface, coupled with major histocompatibility complex (MHC) molecules. This presentation is crucial for the next step—activation of B cells.
B cells, equipped with unique B cell receptors (BCRs), roam through the lymphatic fluid and blood. When a B cell’s receptor specifically binds to an antigen, and receives necessary signals from helper T cells (another type of immune cell), it becomes activated. This dual recognition is essential for ensuring that the immune response is specific and appropriately regulated.
Once activated, B cells begin to proliferate rapidly. This proliferation results in the formation of plasma cells and memory B cells. Plasma cells are short-lived cells that produce high amounts of antibodies specific to the antigen. Memory B cells, on the other hand, persist in the lymphoid tissues for years or even decades, ready to respond more quickly and robustly upon re-exposure to the same antigen.
Plasma cells secrete antibodies into the bloodstream and lymphatic system. These antibodies are Y-shaped proteins specifically designed to bind to the antigen that triggered the immune response. Each antibody has variable regions that allow for the recognition of a unique antigen, ensuring a precise immune response.
Antibodies neutralize pathogens in several ways:
Once the pathogen is neutralized or marked for destruction, the immune system’s cleanup cells, like macrophages, remove the debris from the body. The memory B cells remain vigilant, providing long-term immunity. Upon re-exposure to the same pathogen, these cells can quickly proliferate and produce antibodies, often neutralizing the pathogen before it causes significant harm.
A practical example of humoral immunity is the body’s response to the flu vaccine. When vaccinated, inactivated flu viruses or viral proteins are introduced, acting as antigens that trigger the immune response without causing illness. These antigens are processed by antigen-presenting cells, which display them to B cells. The appropriate B cells, having receptors that specifically recognize these antigens, become activated and differentiate into plasma cells and memory B cells. Plasma cells produce specific antibodies that circulate and bind to the flu virus, preventing infection by neutralizing the virus and marking it for destruction by other immune cells. Meanwhile, memory B cells remain in the body, ready to mount a faster and stronger response if the same virus is encountered again, thereby providing long-lasting immunity.
Active humoral immunity occurs when the immune system is directly exposed to a pathogen or its antigen and responds by producing antibodies. This type of immunity can be further subdivided into natural and artificial immunity:
Passive humoral immunity involves the direct transfer of antibodies from one individual to another. This type of immunity provides immediate protection but is temporary because the body does not produce its own antibodies and does not form a memory response. Passive immunity can also be natural or artificial:
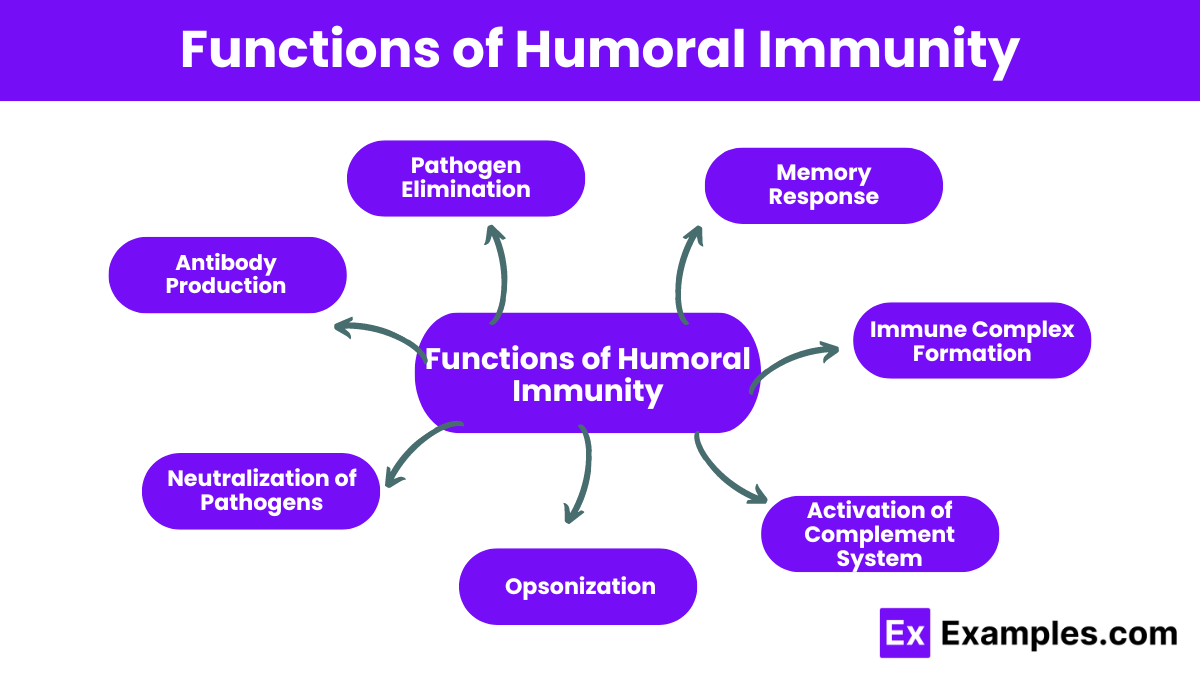
The primary function of humoral immunity is to produce antibodies, which are proteins that specifically recognize antigens (foreign substances such as parts of bacteria, viruses, or other pathogens). B cells are the lymphocytes directly responsible for antibody production. When these B cells encounter an antigen, they transform into plasma cells that secrete large quantities of antibodies.
Antibodies neutralize pathogens by binding to them and blocking their ability to infect host cells. This binding inhibits the biological processes necessary for the pathogen to replicate and spread, effectively stopping the infection in its tracks.
Opsonization is the process by which antibodies coat a pathogen to enhance its recognition by phagocytes (cells that ingest and destroy pathogens). This “tagging” facilitates the more efficient elimination of the pathogen by the immune system.
Antibodies initiate and enhance the complement cascade, a series of protein reactions in blood plasma that aids in pathogen elimination. The complement system can lyse pathogenic cells directly or assist in opsonization and inflammation, thereby bolstering the immune response.
Antibodies bind to antigens to form immune complexes, which are then cleared by other components of the immune system. This process is crucial in preventing the spread of infections and in the neutralization of toxins produced by pathogens.
Humoral immunity is instrumental in developing immunological memory. Memory B cells are produced following an initial exposure to an antigen. These cells persist long-term and enable a quicker and more effective antibody-mediated response upon subsequent exposures to the same antigen. This memory response is the principle behind vaccinations.
The activation of humoral immunity is a complex process involving several steps and components of the immune system. It starts when the body encounters a foreign pathogen, and unfolds as follows:
The process begins when an antigen, typically a protein or polysaccharide on the surface of a pathogen such as a virus or bacterium, enters the body. This antigen is foreign and distinct enough to be recognized by the immune system.
Antigen-presenting cells (APCs), which include dendritic cells and macrophages, capture the antigen. These cells process the antigen by breaking it down into smaller fragments and then display these fragments on their surface using molecules called Major Histocompatibility Complex (MHC) class II. This presentation is critical for the next step, which involves T cells.
Helper T cells (specifically CD4+ T cells) recognize the antigen fragments presented by the APCs through their T cell receptor (TCR). This recognition is aided by the fit between the TCR and the antigen-MHC complex. Once engaged, helper T cells become activated and begin to proliferate and differentiate into various subsets that perform different functions.
B cells, which also roam the bloodstream and lymphatic system, possess specific B cell receptors (BCRs) that can bind to their respective antigens directly. When a B cell’s receptor recognizes and binds to an antigen, and receives additional signals from an activated helper T cell (a process called T cell help), it becomes fully activated. This interaction typically occurs in the lymph nodes or spleen.
Once activated, B cells begin to proliferate and differentiate into plasma cells and memory B cells. Plasma cells are specialized cells that produce large volumes of antibodies specific to the antigen that triggered the response. These antibodies are released into the bloodstream to target and neutralize the pathogen. Memory B cells remain in the lymphatic system, ready to respond more quickly and effectively if the antigen is encountered again in the future.
Plasma cells secrete antibodies into the bloodstream. These antibodies bind specifically to the antigen on the surface of pathogens, marking them for destruction and preventing them from infecting cells. This antibody-mediated response is the hallmark of humoral immunity.
With the help of antibodies, the immune system can neutralize pathogens by blocking their ability to enter cells, clumping them together for easier phagocytosis, or activating the complement system to destroy the pathogen.
Antigens are foreign molecules that elicit an immune response. They are typically proteins or polysaccharides found on the surface of pathogens like bacteria and viruses. Antigens are recognized by antibodies and immune cells, triggering the immune response.
B cells are a type of lymphocyte that play a pivotal role in humoral immunity. They are responsible for producing antibodies. Each B cell has a unique receptor on its surface that binds to a specific antigen. Upon activation, B cells differentiate into plasma cells, which secrete antibodies, and memory B cells, which provide long-term immunity.
Antibodies, also known as immunoglobulins, are Y-shaped proteins that are produced by plasma cells. They specifically bind to antigens to neutralize pathogens and mark them for destruction by other immune cells. Antibodies are crucial for neutralizing viruses and bacteria, preventing them from infecting cells.
Plasma cells are derived from B cells and are the primary producers of antibodies in the immune system. Once a B cell encounters its specific antigen and receives the necessary signals from helper T cells, it can differentiate into a plasma cell.
Helper T cells are another type of lymphocyte that plays a critical role in both cellular and humoral immunity. They aid in B cell activation by providing essential signals that promote B cell proliferation and differentiation.
Antigen-presenting cells, such as dendritic cells and macrophages, are responsible for capturing antigens and presenting them to B cells and T cells. This presentation is crucial for the activation of these lymphocytes and the subsequent adaptive immune response.
The complement system is a series of proteins that work with antibodies to destroy pathogens. Activation of the complement system enhances the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism, promote inflammation, and attack the pathogen’s cell membrane.
Humoral immunity is mediated by antibodies, which are produced by B cells. These antibodies specifically target and neutralize pathogens such as bacteria and viruses, playing a crucial role in the immune defense against extracellular organisms.
In humoral immunity, B cells are the primary cells involved. They recognize antigens, produce and secrete antibodies, and develop into memory B cells for long-lasting immunity. Additionally, helper T cells support B cell functions by enhancing antibody production.
Humoral immunity is a part of the adaptive immune system. Unlike the innate immune system, which provides immediate, non-specific immune responses, the adaptive immune system is characterized by its ability to specifically recognize and remember distinct pathogens, making its response more effective with each exposure. Humoral immunity primarily involves the production of antibodies by B cells, which specifically target and neutralize foreign antigens, such as those found on bacteria and viruses. This specificity and the capability for memory are hallmarks of adaptive immunity.
Humoral immunity involves antibodies and B cells, while cell-mediated immunity relies on T cells without antibodies.
B cells are central to humoral immunity, producing antibodies to fight extracellular pathogens.
It’s called cell-mediated because it depends on direct actions of cells, particularly T cells, rather than antibodies.
Humoral immunity is the body’s way of fighting infections using antibodies produced by B cells.
Text prompt
Add Tone
10 Examples of Public speaking
20 Examples of Gas lighting
What is the primary role of B cells in humoral immunity?
To directly destroy pathogens
To produce antibodies
To present antigens to T cells
To enhance phagocytosis
What type of immunity is provided by the antibodies produced during humoral immunity?
Passive immunity
Cell-mediated immunity
Active immunity
Natural immunity
Which cells are responsible for producing memory cells in humoral immunity?
T cells
B cells
Macrophages
Dendritic cells
Which immunoglobulin is primarily involved in the initial response to an infection?
IgG
IgM
IgA
IgE
How do antibodies neutralize pathogens?
By increasing inflammation
By promoting cell division
By binding to antigens and blocking their function
By enhancing bacterial growth
What is the role of helper T cells in humoral immunity?
To directly kill infected cells
To stimulate B cells to produce antibodies
To destroy foreign proteins
To secrete antibodies
What is a characteristic feature of the secondary immune response compared to the primary response?
It produces fewer antibod
It is slower than the primary response
It produces antibodies of higher affinity
It does not involve memory cells
Which immunoglobulin is most abundant in the bloodstream and provides the majority of antibody-based immunity?
IgM
IgA
IgG
IgD
How do vaccines relate to humoral immunity?
They directly kill pathogens
They stimulate the production of antibodies
They inhibit T cell function
They prevent all infections
What is the significance of class switching in B cells?
It increases the number of T cells
It changes the type of antibody produced
It enhances memory cell formation
It decreases antibody diversity
Before you leave, take our quick quiz to enhance your learning!

