What is the primary function of mast cells in the immune system?
Produce antibodies
Release histamine and other mediators
Destroy pathogens directly
Provide physical barriers to pathogens

Mast cells are pivotal players in the body’s immune system, acting as sentinels that detect and respond to foreign threats. This complete guide delves into their crucial role in health and disease, offering insightful examples of their function. From their involvement in allergic reactions to their importance in wound healing and defense against pathogens, mast cells are multifaceted warriors in our body’s defense arsenal. Discover their mechanisms, how they contribute to various conditions, and the latest research uncovering their potential in medical science.
Mast cells are a type of white blood cell, part of the body’s immune system, with a key role in both protective responses to foreign threats and in the development of allergic reactions. They are found in tissues throughout the body, particularly in areas that are interfaces with the external environment, such as the skin, lungs, digestive tract, and along blood vessels and nerves.
Mast cells contain granules rich in histamine and heparin, which are released into the surrounding tissue in response to certain triggers. This release can be initiated by a variety of stimuli, including allergens, physical injury, or infection, making mast cells crucial in immediate hypersensitivity reactions and inflammatory processes.
The release of histamine from mast cells leads to many of the symptoms associated with allergic reactions, such as itching, swelling, and redness. In addition to histamine, mast cells produce a wide array of cytokines, chemokines, and growth factors, contributing to their role in inflammation, tissue repair, and even the regulation of blood flow and immune responses to pathogens.
Mast cell activation and degranulation are pivotal processes in the body’s immune response, playing a crucial role in allergic reactions, inflammation, and protection against pathogens. This guide dives deep into the intricacies of these processes, offering a detailed look at how mast cells operate and their impact on health.
Mast cell activation is the process by which mast cells respond to external stimuli, such as allergens, pathogens, or physical injury. Upon activation, these cells undergo a change that prepares them to release stored chemicals in their granules, such as histamine, heparin, and various cytokines and chemokines. This activation can be triggered through different pathways, including the cross-linking of Immunoglobulin E (IgE) receptors on the mast cell surface by antigens, direct injury, or through interactions with complement proteins.
Degranulation is the next step following mast cell activation. It involves the release of the contents of mast cell granules into the surrounding tissue. This release is critical for the immediate hypersensitivity reactions characteristic of allergies and asthma. Histamine, one of the primary chemicals released, causes dilation of blood vessels, increased permeability, leading to symptoms like swelling, redness, and itching. Other mediators released during degranulation play roles in attracting other immune cells to the site, amplifying the immune response.
Several factors can influence the activation and degranulation of mast cells, including genetic predispositions, environmental triggers, and the presence of specific antibodies. Understanding these factors is key to managing conditions associated with mast cell dysfunction, such as mast cell activation syndrome (MCAS), where inappropriate activation of mast cells leads to a range of chronic symptoms.
In allergies, mast cell degranulation is a double-edged sword. While it forms a part of the body’s defense mechanism against harmful substances, it can also result in damaging inflammation and the classic symptoms of allergic reactions. In non-allergic immune responses, mast cell activation helps to protect the body against infections by promoting inflammation and recruiting other immune cells to the site of infection or injury.
Management strategies for disorders involving inappropriate mast cell activation, such as MCAS, involve both medication to stabilize mast cells and strategies to avoid known triggers. Treatments may include antihistamines to block the effects of histamine, mast cell stabilizers to prevent degranulation, and corticosteroids to reduce inflammation.
Mast cell signaling is a critical pathway through which mast cells communicate with the rest of the immune system and participate in the body’s defense mechanisms. This comprehensive guide explores the complexities of mast cell signaling, its implications for health and disease, and the potential for therapeutic interventions.
Mast cell signaling involves various receptors on the surface of mast cells that detect external signals, leading to activation, degranulation, and the release of mediators. The most well-known pathway involves the high-affinity IgE receptor (FcεRI), which plays a pivotal role in allergic reactions. When allergens bind to IgE antibodies that are attached to FcεRI receptors on mast cells, it triggers the cells to release histamine and other inflammatory mediators.
Beyond the IgE-mediated pathway, mast cells express a multitude of other receptors that allow them to respond to a wide range of signals, including toll-like receptors (TLRs) for recognizing pathogen-associated molecular patterns, adenosine receptors, and receptors for cytokines and growth factors. These receptors enable mast cells to respond not just to allergens but also to infections, physical injury, and changes in the surrounding environment.
Mast cell signaling plays a crucial role in initiating and modulating immune responses. Through the release of mediators like histamine, prostaglandins, leukotrienes, and cytokines, mast cells influence the behavior of other immune cells, regulate blood vessel permeability, and contribute to the symptoms of inflammation and allergic reactions. Their ability to respond to a wide range of stimuli makes them key players in both innate and adaptive immunity.
An essential aspect of mast cell signaling is its cross-talk with other cells in the immune system, such as T cells, B cells, and neutrophils. This interaction is crucial for coordinating the body’s response to infection and injury. For example, cytokines released by mast cells can attract and activate other immune cells, amplifying the immune response where needed.
Dysregulation of mast cell signaling can lead to various pathologies, including allergic diseases, asthma, autoimmune disorders, and even some forms of cancer. Understanding the mechanisms of mast cell signaling is therefore vital for developing targeted therapies that can modulate these responses, providing relief for patients with mast cell-related conditions.
Advances in our understanding of mast cell signaling pathways have opened up new avenues for therapeutic intervention. Drugs that target specific receptors or signaling molecules involved in mast cell activation can help manage conditions like allergies and asthma. For example, omalizumab, an anti-IgE antibody, can prevent the activation of mast cells by neutralizing IgE and reducing allergic reactions.
Mast cells, key components of the immune system, are strategically positioned throughout the body to effectively respond to injury, infection, and allergens. This guide delves into the various locations of mast cells within the body, highlighting their significance in both health and disease.
Mast cells are most abundantly found in tissues that are interfaces with the external environment, such as the skin, respiratory system, and digestive tract. Their presence in these locations allows them to serve as frontline defenders against pathogens and allergens. However, mast cells are also located in other areas, including connective tissues, around blood vessels, and in nerves, playing roles in wound healing, inflammation, and neuroimmune interactions.
In the skin, mast cells are critical for initiating inflammatory responses to injury and infection. They contribute to wound healing processes and play a key role in allergic reactions, such as hives and contact dermatitis. The high concentration of mast cells in the skin makes it a common site for allergic responses.
Within the respiratory tract, mast cells are found in the lining of the nose, throat, and lungs. They are crucial in responding to inhaled allergens, contributing to symptoms of asthma and allergic rhinitis (hay fever). By releasing mediators like histamine, they cause bronchoconstriction, mucus production, and inflammation of the airways.
The digestive tract is another primary location for mast cells, where they help regulate gut immunity and barrier function. They play a role in responding to food allergens and pathogens, contributing to gastrointestinal disorders such as inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) when dysregulated.
Mast cells are also found in connective tissues throughout the body, including the joints, where they can influence inflammation and pain in conditions like arthritis. Their role in connective tissues underscores their importance in tissue repair and fibrosis.
The specific locations of mast cells in the body are key to understanding their roles in various diseases. For instance, their abundance in the respiratory and digestive systems explains their significant involvement in asthma and food allergies. Targeting mast cell activity in these locations can be crucial for treating these conditions.
Understanding the specific locations and functions of mast cells offers potential therapeutic targets. For diseases characterized by inappropriate mast cell activation, such as mastocytosis or mast cell activation syndrome (MCAS), treatments that stabilize mast cells or inhibit their release of mediators can significantly improve symptoms.
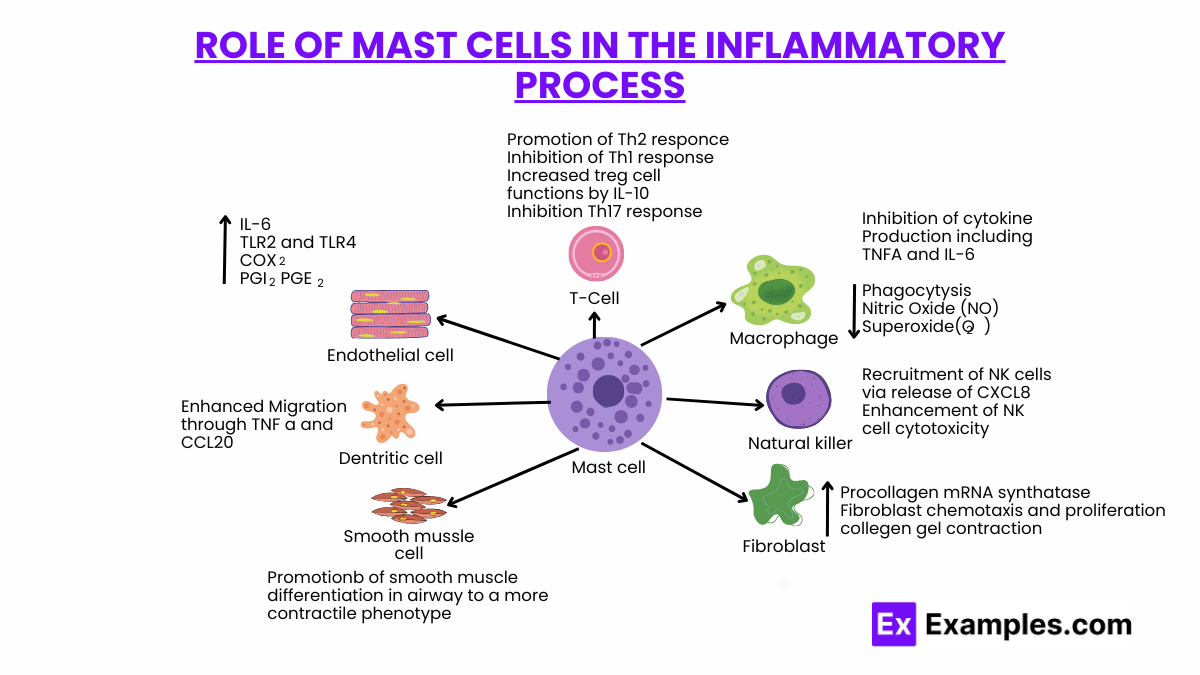
Mast cells play a pivotal role in the body’s inflammatory response, bridging innate and adaptive immunity. This guide explores the complex functions of mast cells in inflammation, elucidating their impact on health and disease.
Mast cells, upon activation, release a plethora of mediators such as histamine, proteases, cytokines, and chemokines. These substances contribute to vasodilation, increased vascular permeability, recruitment of other immune cells, and tissue remodeling. Activation can occur via various stimuli, including allergens, pathogens, physical injury, and immune complexes, highlighting mast cells’ versatile role in detecting and responding to diverse threats.
Histamine, released by mast cells, is synonymous with allergic reactions and plays a critical role in inflammation. It increases blood vessel permeability, allowing immune cells to access the site of injury or infection. Histamine’s effects on smooth muscle contribute to symptoms such as bronchoconstriction in asthma and itching in skin reactions.
Mast cells produce a wide array of cytokines, including TNF-α, IL-1, IL-6, and IL-8, which orchestrate the inflammatory response. TNF-α, for instance, is pivotal in initiating inflammation, promoting endothelial cells to express adhesion molecules that facilitate leukocyte migration. Through cytokine production, mast cells influence the severity and duration of inflammatory responses.
Mast cells interact with various immune cells, such as T cells, B cells, neutrophils, and eosinophils, enhancing the immune response. Their release of chemokines attracts these cells to the site of inflammation, where they perform distinct roles, from pathogen clearance to tissue repair. This cross-talk is essential for a coordinated response to threats.
While beneficial in acute responses, mast cell activation can contribute to chronic inflammation in diseases such as asthma, rheumatoid arthritis, and inflammatory bowel disease. Persistent mast cell activation leads to ongoing tissue damage and remodeling, underlining the need for targeted therapies in conditions driven by excessive inflammation.
Understanding the role of mast cells in inflammation has led to the development of treatments aimed at mitigating their activity. Medications like antihistamines, corticosteroids, and mast cell stabilizers seek to reduce the symptoms of inflammation by inhibiting mast cell degranulation or blocking the action of released mediators.
Mast cells, traditionally recognized for their role in allergic reactions and anaphylaxis, are increasingly acknowledged for their involvement in cardiovascular disease (CVD). These versatile immune cells, found in various tissues throughout the body, including the heart and blood vessels, play complex roles in the development and progression of CVD. This exploration sheds light on the multifaceted contributions of mast cells to cardiovascular health and disease.
Atherosclerosis, the buildup of plaques in the arteries, is a leading cause of heart attacks and strokes. Mast cells contribute to the initiation and progression of atherosclerotic plaques through the release of inflammatory mediators such as cytokines, chemokines, and growth factors. These substances promote the recruitment of other immune cells to the arterial wall, encourage the proliferation of smooth muscle cells, and contribute to the degradation of the extracellular matrix, leading to plaque destabilization. Mast cell-derived mediators can also induce the expression of adhesion molecules on endothelial cells, facilitating the adhesion and transmigration of monocytes and T cells into the intima, further fueling the inflammatory process.
Hypertension, or high blood pressure, is another risk factor for the development of cardiovascular diseases. Mast cells are implicated in the pathophysiology of hypertension through their ability to influence vascular tone and remodeling. The release of vasoactive substances like histamine from mast cells can affect blood vessel constriction and dilation, while cytokines and growth factors released by these cells can promote vascular stiffness by enhancing extracellular matrix production and fibrosis. Furthermore, mast cell-derived renin can directly contribute to blood pressure regulation by activating the renin-angiotensin-aldosterone system, a key regulator of blood pressure and fluid balance.
Following a myocardial infarction (MI), or heart attack, mast cells participate in the inflammatory response that is critical for tissue repair and remodeling. However, excessive or prolonged mast cell activation can contribute to adverse remodeling and the progression to heart failure. Mast cells release mediators that can exacerbate tissue damage, fibrosis, and ventricular dilation. In heart failure, mast cell density in the heart is often increased, and their mediators can further impair cardiac function by promoting inflammation, fibrosis, and angiogenesis.
The involvement of mast cells in cardiovascular diseases offers potential therapeutic targets. Inhibiting mast cell activation or blocking the action of specific mediators released by mast cells could provide novel strategies for the treatment and prevention of CVD. For example, mast cell stabilizers, antihistamines, and inhibitors of cytokine and chemokine receptors are potential therapeutic agents that could mitigate the detrimental effects of mast cells in cardiovascular pathology.
Another name for mast cells is “labrocytes.” This term is less commonly used today, but historically, it has been applied to refer to mast cells due to their granular appearance under the microscope and their role in releasing substances that affect the body’s connective tissue.
Mast cells are immune cells that play a key role in allergic reactions and inflammation, containing granules filled with various mediators, including histamines. Histamines are biochemical compounds released by mast cells upon activation; they cause symptoms like itching, swelling, and redness during allergic responses.
Mast cells originate from hematopoietic stem cells in the bone marrow. They differentiate from precursor cells that circulate in the bloodstream and then migrate into various tissues throughout the body, where they mature and acquire their characteristic functions and mediator content, playing key roles in immunity and inflammation.
Mast cells are crucial components of the immune system, playing multifaceted roles in allergic reactions, pathogen defense, and inflammatory processes. Originating from bone marrow, they mature in various tissues, where they respond to diverse stimuli. Understanding mast cells’ functions and signaling pathways offers potential therapeutic targets for treating allergies, autoimmune diseases, and other inflammatory conditions.
Text prompt
Add Tone
10 Examples of Public speaking
20 Examples of Gas lighting
What is the primary function of mast cells in the immune system?
Produce antibodies
Release histamine and other mediators
Destroy pathogens directly
Provide physical barriers to pathogens
Where are mast cells commonly found in the body?
Bone marrow
Lymph nodes
Connective tissues and mucosal surfaces
Blood plasma
Which of the following substances do mast cells release to initiate inflammation?
Insulin
Serotonin
Histamine
Glucagon
What role do mast cells play in allergic reactions?
They neutralize allergens directly
They trigger the release of histamine and other inflammatory mediators
They provide long-term immunity
They produce antibodies against allergens
Which type of immunity are mast cells most associated with?
Innate immunity
Adaptive immunity
Passive immunity
Cellular immunity
How do mast cells contribute to the defense against parasitic infections?
By producing antibodies specific to parasites
By releasing cytokines that enhance the immune response
By releasing histamine and recruiting eosinophils
By directly attacking parasites
What is the effect of mast cell degranulation?
Release of anti-inflammatory agents
Release of histamine and other pro-inflammatory mediators
Suppression of immune responses
Production of regulatory T cells
In which type of hypersensitivity reaction are mast cells most involved?
Type I hypersensitivity
Type II hypersensitivity
Type III hypersensitivity
Type IV hypersensitivity
What happens to mast cells during an anaphylactic reaction?
They become inactive
They proliferate uncontrollably
They release large amounts of histamine
They destroy themselves
Which of the following treatments can help manage symptoms related to mast cell activation?
Antihistamines
Antibiotics
Antivirals
Antifungals
Before you leave, take our quick quiz to enhance your learning!

