5+ Soap Assessment Examples to Download
Whether you are a student or a healthcare worker, it is always your responsibility to make your notes as clear, concise and neat as possible. Though this may seem more like a challenge to some, this is also a part of a requirement for those who study or work in the medical field. The reason for having to do this is to keep your notes as easy to understand as possible. The same goes when doing an assessment. There may be times when you are doing your best in following the exact steps you took and writing it down in the assessment, that your writing may not be as clear or neat as before. Rather than having to deal with a lot of information of where, what and why, a SOAP assessment is done to help you out. Check out this SOAP assessment below for more information.
5+ Soap Assessment Examples
1. Soap Assessment Template
2. Standard Soap Assessment
3. Clinical Soap Assessment
4. Soap Assessment in PDF
5. Investigation Soap Assessment
6. Soap Assessment Progress Note
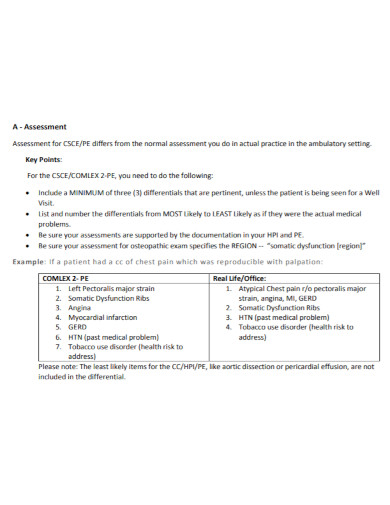
Definition of SOAP
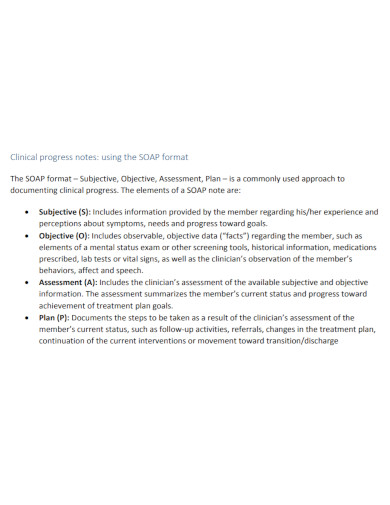
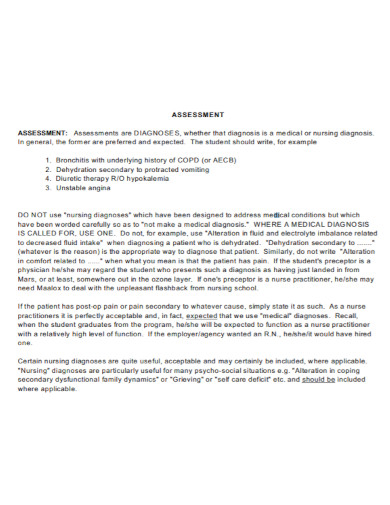
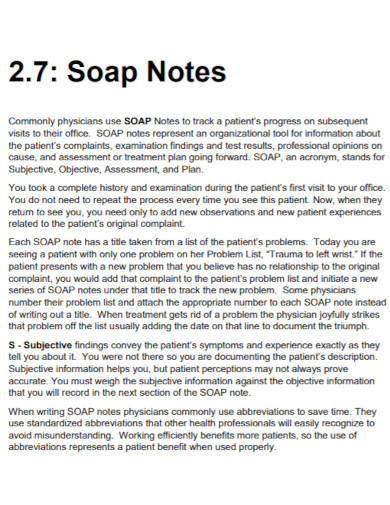
To begin, we must first define the acronym S.O.A.P. or simply called SOAP. The acronym is short for Subjective, Objective, Assessment, Procedure. This is a method that is often used by people in the medical field. These types of notes give healthcare workers and people in the medical field a better understanding of the notes they have. It is also less time consuming to search for the note assessments they may need when catering to patients on a daily basis. All they have to do is to fill out what falls under subjective, objective and procedure as they do their assessment notes.
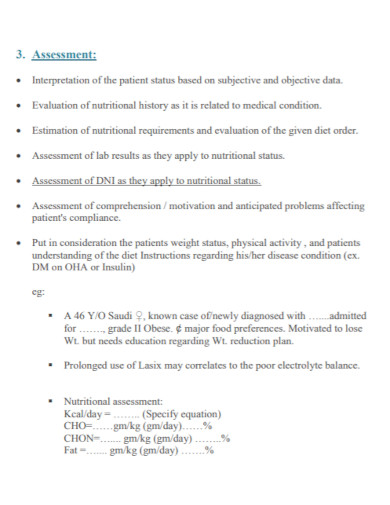
Definition of SOAP Assessment
A SOAP assessment is a method that healthcare workers and anyone in the medical field uses. This is a shorter and more precise version of the longer notes that is not only time consuming but can take a lot of work to fill out. This assessment is used as a way to extract information from the patient’s charts and to use it for their own assessment notes. In addition to that, a SOAP Assessment also hands out the precise information needed provided that these healthcare workers used the format to make it less problematic. These types of notes are quite useful especially when writing a lot can take time and energy out of a person as well as time is gold.
Importance of SOAP Assessment
The importance of having to do a SOAP assessment is these assessment notes are mostly used as a guide. A road map if you want to compare it to the information being added to a patient’s chart. It is also relevant enough for them to be able to record new information about the patient and their progress. The advantage of using the note assessment is that you are more organized. Information is also easy to come by. In addition to that, in case of emergencies, medical experts would no longer need to search for the history of a patient. They can simply take out their notes and take the information they need without wasting time.
Tools Used for SOAP Assessment
Here are some tools. These tools can be used for your SOAP Assessment.
- Narrative Form
- Table Form
- Bullets
- Outline
- Diagram
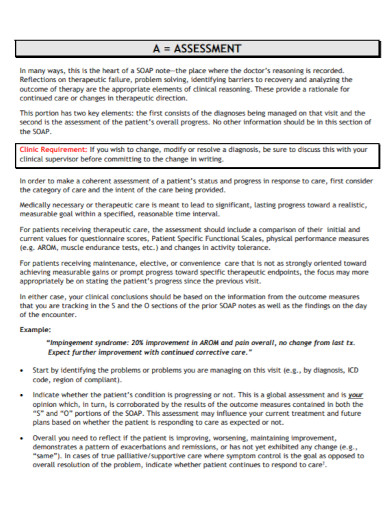
Tips for SOAP Assessment
- Make your assessment notes clear
- Your assessment should follow the format Subjective, Objective, Assessment, Procedure
- Fill out the correct information
- Give an evaluation after the assessment
- Your objectives have to be specific and realistic
FAQs
Why is a SOAP Assessment useful?
For those working in the medical field or healthcare, a SOAP Assessment is an easier way for them to use to assess their patients. It is not only straight to the point, but it is also constructed in an organized way. The assessment and the notes do go hand in hand so it is also useful for them to not have to find out how the results came and what were the steps that they took to get it. All they need to do is to simply check the outlined data.
What to expect when writing a SOAP Assessment?
When writing a SOAP Assessment, expect a neat filled up notes. This is as important as the whole assessment. Your assessment notes are as important to you as they are to the next person using it.
What does a SOAP assessment look like?
Your SOAP assessment notes differ from person to person using it. The common denominator however is the format. It should follow subjective, objective, assessment, procedure.
Should a SOAP assessment be neat?
Yes. As this is needed when you have to understand and know the history of a patient. By doing this, your notes have to be clean and understandable.
SOAP assessment notes are as important as filling them out. Information that should be gathered, collected and assessed are required for the assessment to be complete. But you must also remember that making your notes clear and easy to understand is also another thing to keep. For working in medical fields, there is no such thing as wasting time when emergencies may happen just about anytime and anywhere.