Buying land through real estate is one way of attaining the kind of land you plan to own. When we plan to purchase or rent out a piece of land or simply the entire land, we are often given a piece of document that states the necessary information. This is not to make us feel like we cannot purchase it or rent it, rather it is to expect what is supposed to be in the paper. The information given to us would help us understand and to make us agree to it before any exchange of business can occur. Whether it would be to buy or to rent, we cannot deny that we would still need the exact paperwork and the right amount of knowledge to get this kind of business done. For many of us, to purchase or to rent a piece of land may take a lot of resources and paperwork, but to some who have done this before, it only takes a very important piece of paper to settle the matter. A contract agreement.
[bb_toc content=”][/bb_toc]
4+ Land Contract Agreement Examples
1. Land Contract Agreement Template

2. Land Contract Purchase Agreement Template
3. Standard Land Contract Agreement
4. Draft Land Contract Agreement
5. Land Contract Agreement in PDF
What Is a Land Contract Agreement?
A land contract agreement is a binding piece of paper that real estate agents, companies and even landowners use in order to bind another party who is interested in purchasing land or renting it from a business owner, or a landowner for business use. The contract agreement gives out information about the seller and the buyer, the terms and conditions of the contract, the payment arrangement and of course the signatures that prove that the ownership of the land is changed from one party to the other. As for the purpose of a land contract agreement, it is to give new ownership to the party that bought the land and to give any other legal documents to the new owner. The contract agreement acts as proof that the land that has been purchased has a new owner. The contract agreement is only legally binding if the exact information and signatures are present and can be terminated or void if the signatures and information are missing.
How to Write a Land Contract Agreement?
When dealing with contract agreements, it can sometimes be tricky, and unpredictable. This is why when you write your land contract agreement, you must also be very careful, stick to the facts and be clear and concise as much as possible. Here are some tips on what you should expect in a land contract agreement.
1. Names, Address and Contact Details of the Parties
When you start out with your land contract agreement, you would always have to start with the names of the parties that are going to be selling and purchasing. The complete names, address and contact details of both parties should be written down in the agreement.
2. Terms and Conditions That Apply to the Agreement
Along with the names and contact details of the parties, you would notice terms in bold that would state the terms and conditions. The terms and conditions should be written in order for the party to know the things they need in order to purchase the land from you. In the contract agreement, the terms and conditions are there to make it clear to the purchasers that this would be their roles, duties and responsibilities when they are going to be purchasing the land.
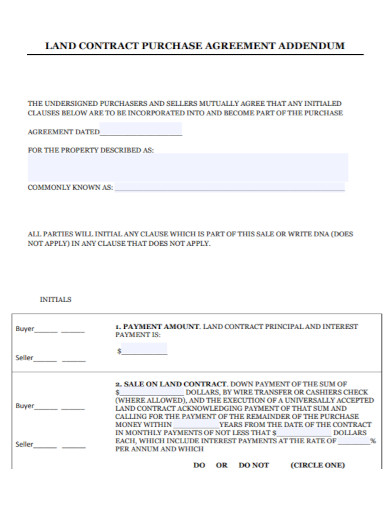
3. Down Payment, Security Deposit, and Final Payment
Apart from the terms and conditions, you must also make sure to add in the contract agreement the down payments, the security deposit which helps the purchasers reserve the land they plan on taking, and of course the final payment. All of which is important for them to check before they are able to get or able to purchase the land from you. However, if there are cases wherein they are not able to give the final payment, you as the owner have the right to withhold the land until they are able to give the final payments. As should be stated in the terms and conditions.
4. Signature and Date of the Agreement
When everything has been settled, the last thing to do is to get the signatures of both the seller and the purchaser and add the date of the agreement. The full purpose of the signatures is to fully bind, complete and seal the contract agreement, signatures of the seller and the purchaser as well as the date of when the signatures have been made.
FAQs
What is a land contract agreement?
A piece of document that binds the purchaser and the seller to the land. The agreement states the terms and conditions, the responsibilities and the necessary details that the seller must comply with in order to purchase the land from the owner or from the real estate agent.
Why are terms and conditions in an agreement so important?
The purpose of the terms and conditions in the agreement is to inform the purchaser of their responsibilities or duties when they will be purchasing the land. For the seller, it is simply to give the title of ownership to a different party when the purchaser has succeeded in buying off the land from the owner.
Why do you need copies for the purchaser?
The purchaser has the right to the exact copy of the contract agreement that both of you have signed. It acts as an important receipt, a proof that they are the new owners of this land.
When you want to buy off some land from real estate or from a private owner, you must always take into consideration the important documents and paperwork that go with it. For real estate or for land owners, the document that they would need is a land contract agreement.