11+ Medical Authorization Form Examples to Download
We have the full autonomy over our bodies and the right to assert such should we find the need to. The health science community, from medical research to clinical practice, upholds and protects individual liberties, including those of the vulnerable population. This sector is composed of people that do not have the legal capacity to provide voluntary and informed consent during emergencies and medical-related situations. The group includes persons with physical and mental impairment, children, and others whose circumstances put them at risk of exploitation. As a protection of the rights of these people, medical authorization letters and forms are required before administering medical interventions.
Medical authorization forms proactively grant authority to health professionals to perform vital procedures to a vulnerable person. From here, vulnerable person refers to the people who cannot give full consent. For minors, their parents or immediate guardian fill in and sign the medical consent forms. This process is required because medical interventions are not generic. Although doctors are intelligent, they do not know at first glance if a medical treatment will have adverse effects on the patient. The patient may die or be irreversibly impaired. This can be a ground for negligence. This will result in court cases and losing the license to practice. The forms are not limited to granting permission to treat a vulnerable person.
The document is also used in other institutions and establishments to obtain or release confidential information. As part of risk evaluation, the employer can request for the employees’ medical details to properly accommodate their health concerns in the workplace. This is to facilitate a safe work environment for the organization and provide a fast medical response when necessary. Meanwhile, health insurance companies require their members to fill in the medical authorization forms. This process allows a company to legally release its member’s personal and medical information to health care providers.
Exercise of Foresight and Prudence
Medical emergencies are unpredictable by nature. The child could be out for a school field trip when his or her allergic reaction to certain food became a full-blown medical emergency. The child cannot consent to procedures to be done on him or her. The parents cannot be contacted on time. It is a life-or-death predicament. This will not happen at every activity or event, but there are chances that a similar scenario might take place. Unless a chaperone is granted a consenting authority, he or she cannot decide for the child. The attending health professionals may be versed in treating medical conditions, but they also need the child’s medical information and the consent of immediate guardians. Aside from permission slips, secure medical authorization forms before an event to prepare for situations like this.
First, Do Not Cross Lines
The process of gaining informed consent before doctors can intervene in a medical situation did not appear out of the blue. We can trace this practice to the institution of medical ethics. The principles were cemented as guidelines to prevent exploitation and abuse of authority. Informed consent aligns with the mandate of health professionals to “First, do no harm.” Consent stems from the right of individuals to exercise autonomy over their bodies. The patients reserve the right to accept or decline interventions. In cases where the patient cannot decide for him or herself, a legal guardian can decide for him or her.
No Place for Guesswork
Therefore, no matter how we picture health professionals—miracle workers or angels—they cannot do anything without permission, the patient’s information, and medical history. This builds a professional relationship between them and patients based on mutual trust and respect. Medical authorization forms maintain this relationship. It proactively grants authority to provide medical intervention and release private information. The confidential information indicated in the form can be the key to saving a person’s life. The information is protected by law. Data misuse and breach of confidentiality are sanctioned appropriately.
11+ Medical Authorization Form Examples
You can download medical authorization forms for your intended use. There are hundreds of printable templates and samples on the Internet. However, you should see to it that you can edit the template or that it can be for general use. If the file you need is not open to customization, you can take inspiration from its structure and create your own. Scroll down for tips on what should be found in your medical authorization forms.
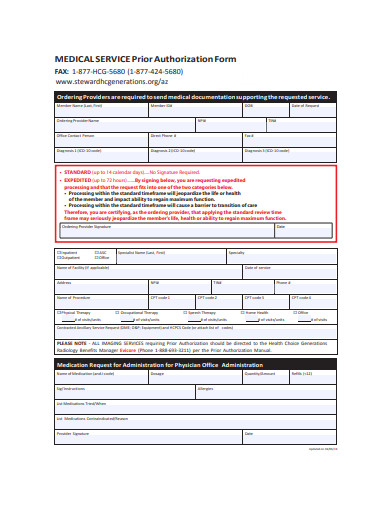
1. Medical Service Prior Authorization Form
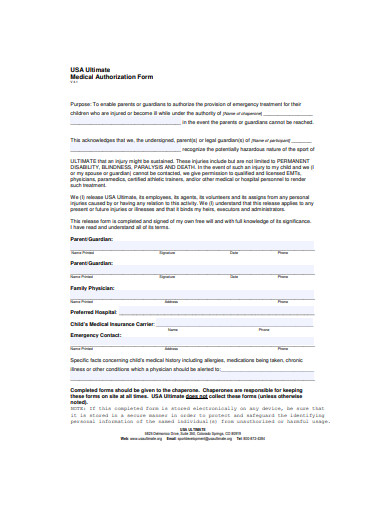
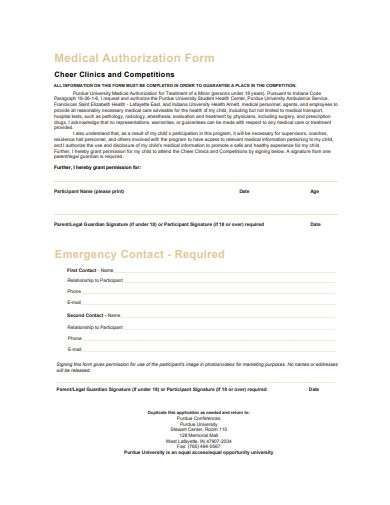
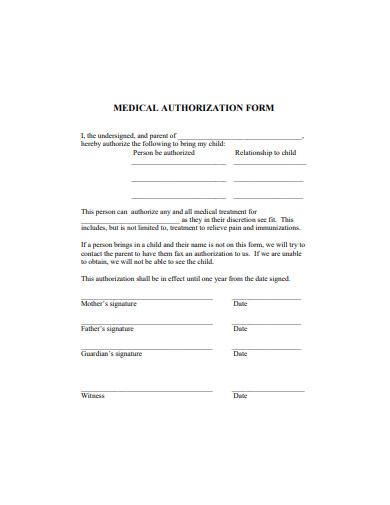
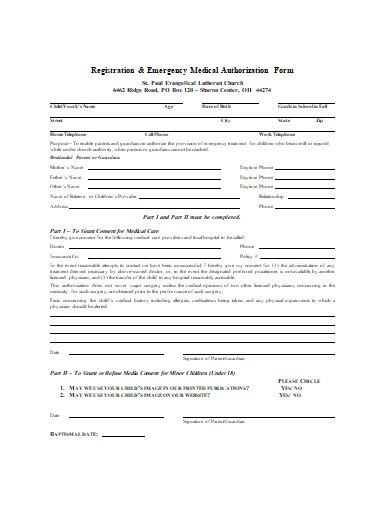
2. Medical Authorization Form
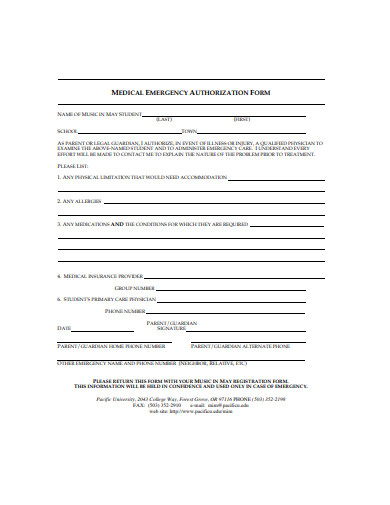
3. Medical Emergency Authorization Form
4. Sample Medical Authorization Form
5. Basic Medical Authorization Form
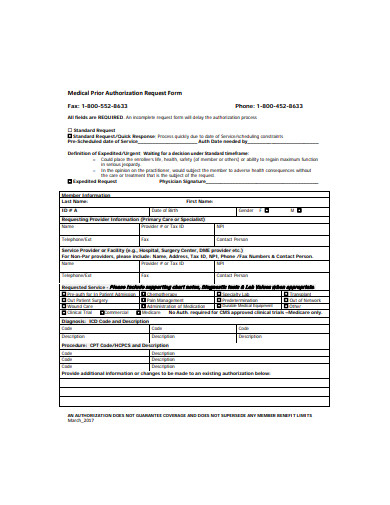
6. Medical Prior Authorization Request Form
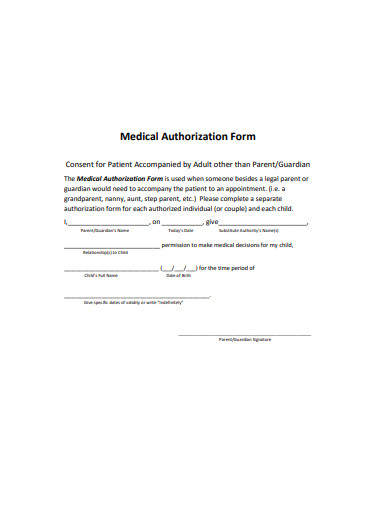
7. Standard Medical Authorization Form
8. Medical Authorization Form Example
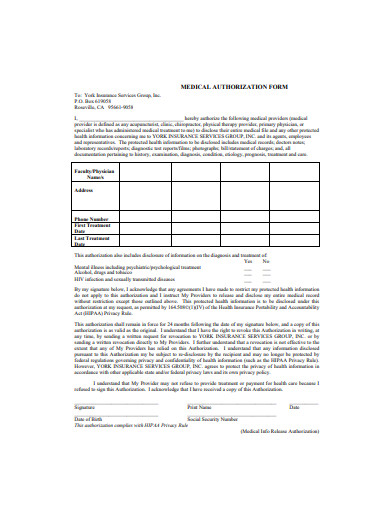
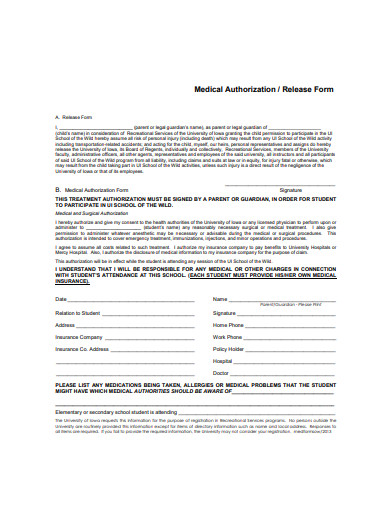
9. Medical Authorization Release Form
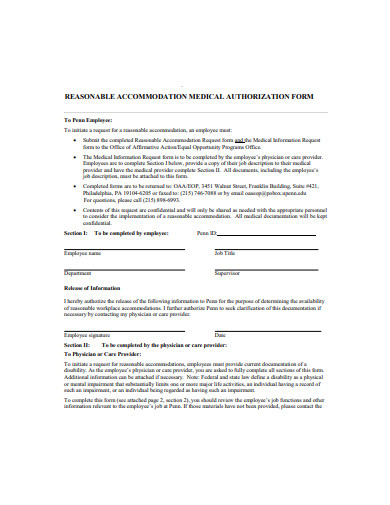
10. Medical Authorization Form Sample
11. Basic Medical Authorization Form Sample
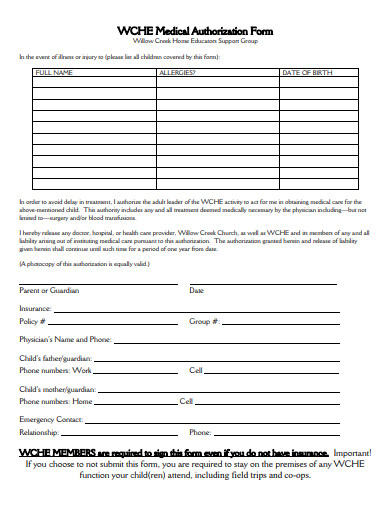
12. Emergency Medical Authorization Form
Elements of an Authorization Form
Standing by the principles of medical ethics, the medical authorization forms share the life-saving backbone. They are similar to the format of authorization letters. The document communicates that the patient or the guardian allows the attending doctors and health professionals to do what they can to save the patient. It also states that an institution can release confidential information to health care providers should that expedite the process of the treatment. The following should be found in the medical authorization form for it to be valid:
1. Patient Profile
This section allows patient identification: name, address, birth date, physical limitations, and so forth. The details are important to provide treatment for the patient. For example, the weight of the patient is an important consideration for the administration of anesthesia. This page should also indicate the information on the patient’s medical insurance provider. The patient profile is vital for correct clinical assessment.
2. Emergency Contacts
The form should indicate the people who must be informed should anything happen to the patient. When the patient is a minor or part of the protected vulnerable group, the emergency contact information of the parents or legal guardian should be written. The name of the patient’s physician has to be stated so that the attending medical personnel can contact the doctor for information.
3. Medical Information
For the attending doctors to know the right medical treatment to provide the patient, they must be aware of the patient’s medical and family history. The history lists down the patient’s medical conditions from hereditary and lifestyle diseases to their allergies. The maintenance and prescription medication list needs to be indicated because knowledge about such can help avoid complications in treatments.
4. Authorization Clause
Medical institutions and health care providers should adhere to the HIPAA confidentiality agreement. These paragraphs state what action is granted to the attending medical professionals or requesting institution. This clause limits the power of these people to do only what is necessary. The provision should be clear on whom the authority is granted. The specifics will avoid ambiguity and unconsented practices. If the authority is meant to grant information disclosure, the clause should clearly indicate what kind of information is allowed to be released. Make sure that the medical authorization form granted is temporary. Specify the duration when the authorization is effective.
Not everyone can provide free, informed consent for medical treatments or data disclosure. That is why the law protects these people from abuse and negligence. Respect for individual autonomy does not stop when that person is not in the right state and condition to decide. The use of medical authorization forms protects the vulnerable group from exploitation. It is required before administering interventions or disclosing confidential data. Different institutions and care providers should have these forms as an in-case measure to safeguard the health of their members.