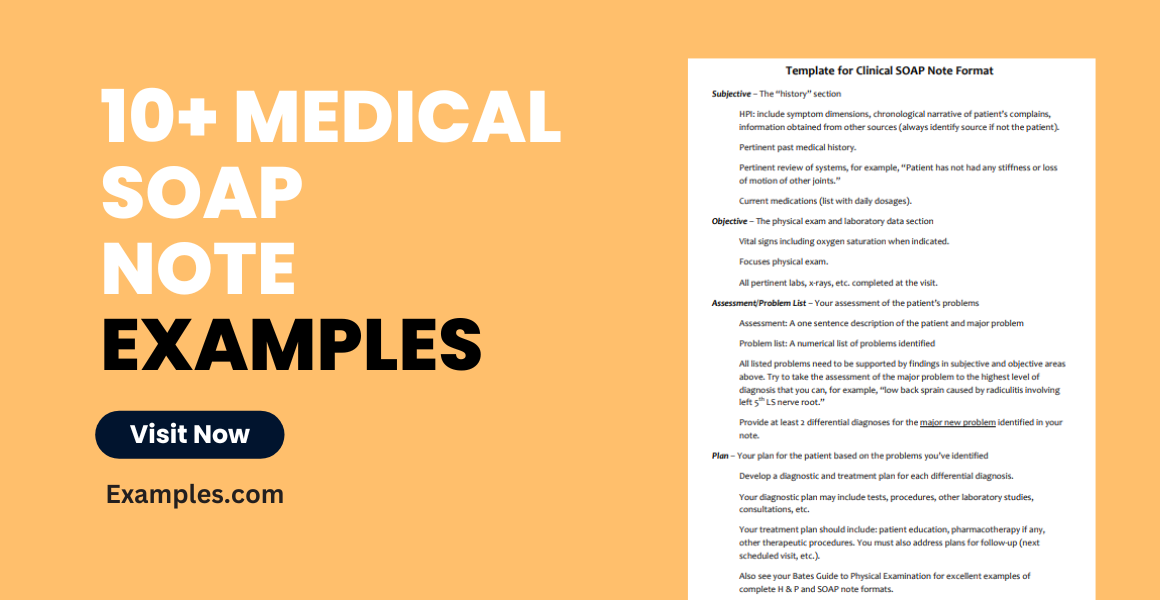
10+ Medical SOAP Note Examples to Download
A medical professional’s scope of work is a lot more complicated than what you imagine it to be. In addition to providing treatment to patients, doctors, dentists, therapists, and nurses also have piles of documents sitting on their desks by the end of each shift. One of which includes the medical SOAP note. The Note is a highly structured format required to communicate information to other healthcare providers, to provide proof of contact with the patient, and to document the procedure taken for treatment.
Medical SOAP Note Examples
1. Medical Doctors Note for Pregnancy
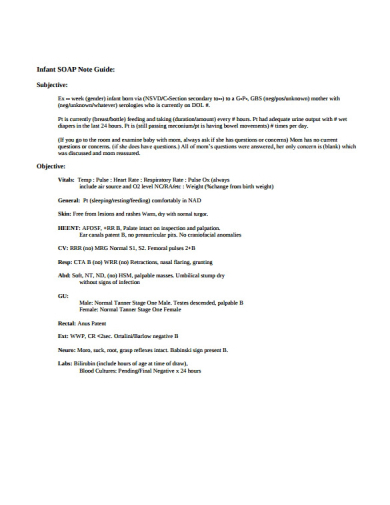
2. Infant Medical SOAP Note Example
The body of an infant is extremely delicate and sensitive to any infections, diseases, or injuries obtained. This is one of the reasons why parents and guardians are strictly advised to have their child checked once certain symptoms become apparent. Medical practitioners typically conduct a series of tests to clear the infant before he or she may be taken home. Infants who were born prematurely, for instance, have to be monitored by the hospital’s staff members for the time being. Medical SOAP notes and growth charting are just a few of the important documents filed by pediatricians and nurses upon the infant’s evaluation.
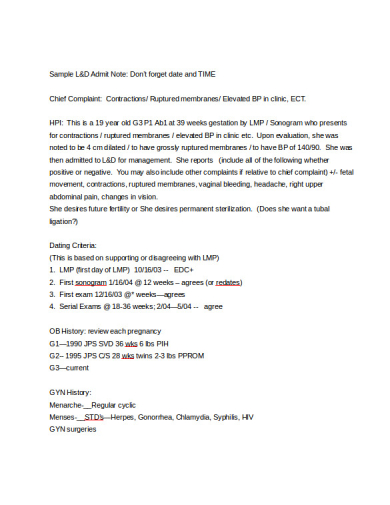
3. Labor & Delivery Medical SOAP Note
Every case at the hospital demands the time and attention of the staff on duty, especially when dealing with cases of labor and delivery. Although expectant mothers go through similar experiences, medical professionals still need to keep a close eye on every patient. A medical SOAP note is written to report on the patient’s current status for further evaluation. This will also help determine whether the mother has made any progress note or regress after a specified period.
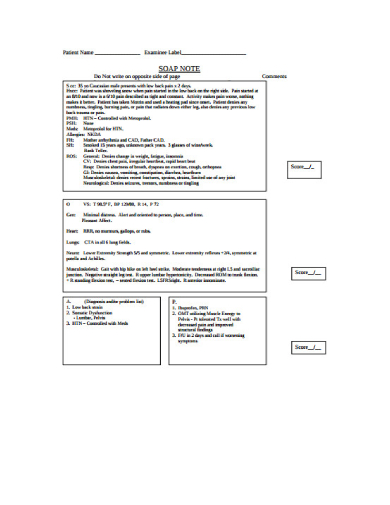
4. Medical Examine SOAP Note Assessment
Defining a SOAP Medical Note:
The SOAP medical note is an organized approach to documentation used by healthcare providers to write out notes in a patient’s chart, along with other common formats, such as the admission note. Standing for Subjective, Objective, Assessment, and Plan, the SOAP note method is a clear-cut and standardized way to note important patient information, enabling a systematic and qualitative approach to patient care.
Understanding the Subjective Component:
The ‘Subjective’ section is the narrative part where the patient’s current condition is described in their own words. It captures the chief complaint, the symptoms described by the patient, and their duration, as well as the patient’s personal experiences of their illness or condition. This section often includes the patient’s medical history, lifestyle, and background, offering context to the symptoms and conditions presented.
Delving into the Objective Section:
Here, the ‘Objective’ observations during the clinical encounter are recorded. This includes vital signs like temperature, blood pressure, and heart rate, as well as findings from physical examinations and measurable data obtained through diagnostics such as lab reports, X-rays, and MRIs. This section provides factual data that does not rely on patient feedback.
Making the Assessment:
The ‘Assessment’ is the healthcare provider’s diagnosis of the patient’s condition. This can include a list of possible diagnoses, which are narrowed down through differential diagnosis techniques. The assessment may also include reflections on the progression of the condition, especially for follow-up visits.
Formulating the Plan:
This final ‘Plan’ section outlines the steps to address the patient’s condition. It covers medications prescribed, therapies initiated, and additional tests or procedures ordered. It also includes patient education, follow-up appointments, and referrals to specialists. The plan is tailored to the patient’s needs and is guided by evidence-based practices.
Integrating the Components for Comprehensive Care:
A SOAP note is only as effective as its integration into the patient’s broader care plan. This documentation helps ensure continuity of care, provides a clear communication trail for future interactions, and can be a critical component in care coordination across different services.
Patient Participation and Education:
Patients are encouraged to be active participants in their healthcare, and SOAP notes can serve as a tool for patient education. The notes should be written in a manner that is accessible to patients, should they request to view their records, fostering transparency and trust between the patient and the healthcare provider.
Legal and Ethical Implications:
In the realm of legal and ethical medical practice, SOAP notes serve as an important record. They can be used in legal situations to verify the care provided and can be subject to audits and reviews in compliance with healthcare regulations.
Advancing Patient Care with SOAP Notes:
The meticulous structure of SOAP notes contributes to a detailed, organized medical record that enhances the quality of patient care. These notes are integral for providers to track the progress of a patient, make informed decisions, and provide a framework for the patient’s journey through the healthcare system.
Medical examinations can be scary for patients who are eager to find out if there’s anything wrong with them. But to a health professional, it’s all in a day’s work. A SOAP note is often used to document this assessment. It can be as brief or as detailed as possible, depending on the amount of information that needs to be acquired.
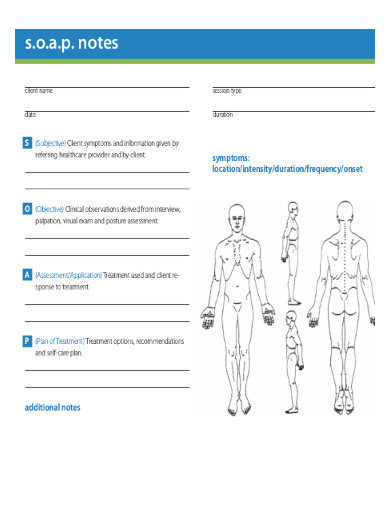
5. Simple Medical Massage Therapy SOAP Note
What is a SOAP Medical Note?
A SOAP Medical Note is a structured method of documentation used by healthcare providers to write out notes in a patient’s chart. SOAP stands for Subjective, Objective, Assessment, and Plan:
- Subjective: The patient’s description of their problem or condition.
- Objective: Observable and measurable facts, such as vital signs and examination findings.
- Assessment: The healthcare provider’s diagnosis or interpretation of the patient’s condition.
- Plan: The proposed treatment strategy, including medications, therapies, and follow-up requirements.
What is an example of a Medical SOAP Note?
Here is an example of a medical SOAP note for a patient with a suspected upper respiratory infection:
Subjective:
The patient reports a persistent cough, sore throat, and nasal congestion for the past three days. They note a low-grade fever at home. The patient denies shortness of breath or chest pain.
This section includes information that the patient reports. It can contain the chief complaint, the patient’s description of the symptoms, the history of the present illness, and a review of systems if relevant. It represents the patient’s perspective on their condition.
Example: The patient complains of severe abdominal pain that started 6 hours ago, which she describes as a constant, sharp stabbing sensation around her navel, now localized to the right lower quadrant, with a severity of 9/10. No appetite since yesterday. Nausea without vomiting. Last bowel movement was this morning, normal in consistency. No changes in diet or recent travel. No prior history of similar pain. No urinary symptoms. Patient appears anxious and reports being worried about appendicitis.
Objective:
- Temperature: 99.8°F
- Heart Rate: 78 bpm
- Respiratory Rate: 16 breaths/min
- Blood Pressure: 120/80 mmHg
- Physical Exam: Throat is erythematous with no exudate. Nasal mucosa is swollen with clear discharge. Lungs are clear to auscultation.
This part includes factual, measurable data. It typically contains vital signs (blood pressure, heart rate, respiratory rate, and temperature), findings from physical examinations, and results from laboratory tests or imaging studies.
Example: Vital signs on examination: BP 125/75 mmHg, HR 98 bpm, Temp 99.5°F, RR 18 bpm. Abdominal examination reveals rebound tenderness at McBurney’s point, positive Rovsing’s sign, no guarding or rigidity. Bowel sounds are normal. No flank tenderness. Murphy’s sign negative. The rest of the physical examination is unremarkable.
Assessment:
The patient presents with symptoms consistent with an upper respiratory infection, likely viral in etiology.
This section is the healthcare provider’s interpretation of the subjective and objective data. It includes the differential diagnosis, which lists the possible conditions that might be causing the patient’s symptoms, and often the working or final diagnosis.
Example: The clinical presentation is suggestive of acute appendicitis. Differential diagnoses include gastroenteritis, ectopic pregnancy (patient is a 28-year-old female), and mesenteric lymphadenitis.
Plan:
- Advise rest and increase fluid intake.
- Recommend over-the-counter acetaminophen for fever and pain.
- Suggest saline nasal spray and throat lozenges for symptomatic relief.
- Instruct the patient to return if symptoms worsen or do not improve in 3-5 days, or if difficulty breathing develops.
This final part outlines the steps that will be taken to further diagnose or treat the patient. It can include ordering additional tests, starting or adjusting medications, referrals to specialists, or providing patient education.
Example: Plan to admit for surgical consultation. CBC, electrolytes, and CRP ordered, along with a pelvic ultrasound to rule out gynecological pathology. Administer IV fluids for hydration and analgesia with IV morphine for pain control. NPO (nothing by mouth) in case of surgical intervention. Instructed patient on the importance of timely surgical evaluation and potential risks if untreated. Will notify the surgical team immediately for further assessment.
This SOAP note provides a concise yet comprehensive overview of the patient’s current complaint, the provider’s findings, their assessment, and the recommended plan of action.
In spite of our ability to do just about anything, the human body does have its limits. Strenuous activities and the lack of proper rest can often lead to muscle pain and other similar conditions. Patients who experience these symptoms are often forwarded to a massage therapist who may help them recover. Massage therapy is highly recommended to relieve pain, rehabilitate sports injuries, provide relaxation, and address anxiety and depression. To help meet these objectives, medical SOAP notes are included in a report.
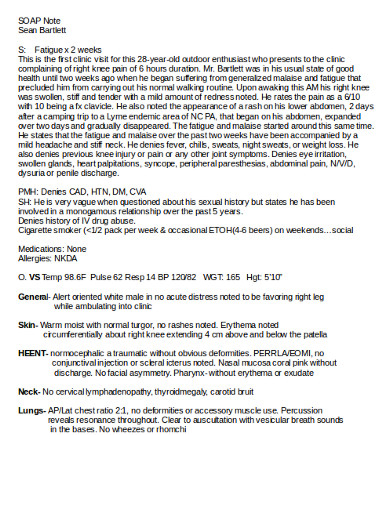
6. Medical SOAP Note of Patient Format
Even though SOAP notes are shared among professionals in the medical field for the purpose of study and advancement, these documents mainly focus on the better treatment of patients. Shown above is an example of a medical SOAP note that discusses the present state of a patient who came to the clinic to seek answers for a few complaints. Practitioners tend to go into detail with their analysis to gather a sufficient amount of information for their records.
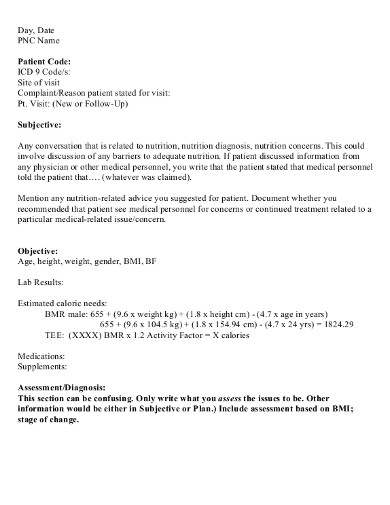
7. Nutrition Medical Student SOAP Note
How to write Medical SOAP Notes?
Writing effective Medical SOAP notes is a critical skill for healthcare providers. It ensures clear communication and documentation of patient encounters. Here is a guideline on how to write a SOAP note:
Subjective:
Begin with the patient’s chief complaint, or reason for the visit. Document the patient’s symptoms and their duration, intensity, and character. Include relevant medical, personal, and family history. Record the patient’s own words or concerns.
Example: “Patient reports sharp chest pain radiating to the left shoulder, began 3 hours ago, 8/10 in severity, feeling short of breath.”
Objective:
This section should include vital signs (e.g., blood pressure, heart rate, respiratory rate, temperature), results from physical examinations, and findings from any investigations (e.g., lab tests, imaging).
Example: “BP 150/90, HR 110, RR 22, Temp 98.6°F. Physical exam shows decreased breath sounds in left lower lung quadrant.”
Assessment:
Analyze the subjective and objective findings to make a clinical SOAP Note. List the differential diagnoses, but ensure to identify a primary diagnosis. This section may also include the rationale for ruling out other diagnoses.
Example: “Primary assessment is acute coronary syndrome. Differential diagnoses include pulmonary embolism and costochondritis.”
Plan:
Outline the management plan. This includes medications prescribed, tests ordered, referrals made, patient education given, and follow-up care.
Example: “Administering aspirin 325mg and nitroglycerin sublingually. Ordering ECG and cardiac enzymes. Referral to cardiology for further evaluation. Follow-up in 24 hours.”
Living with health issues is never easy. You could be put on a meal plan, an exercise regimen, and prescription pills for the rest of your life. Seeing a professional to help you with your struggles is one way to get by. A nutritionist may provide you with some guidelines to prevent your health from deteriorating and causing further problems. To determine which program will suit your condition and assess whether or not it is effective, a medical SOAP is written for documentation and reference. The information found in the medical note may also be discussed with other healthcare personnel to offer proper treatment.
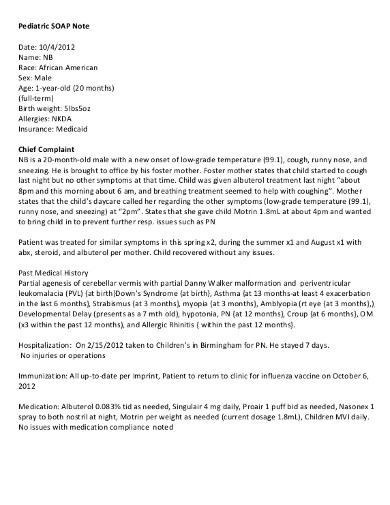
8. Child Pediatric Medical SOAP Note
Being a pediatrician, you deal with various patients who face different types of conditions. But because infants, children, and adolescents can be quite vague with how they express their feelings, creating a medical SOAP note has proven to be a challenge. In such cases, you may have to consult the patient’s parent or guardian for further details. The doctor’s note is essential to aid the healthcare provider in their diagnosis.
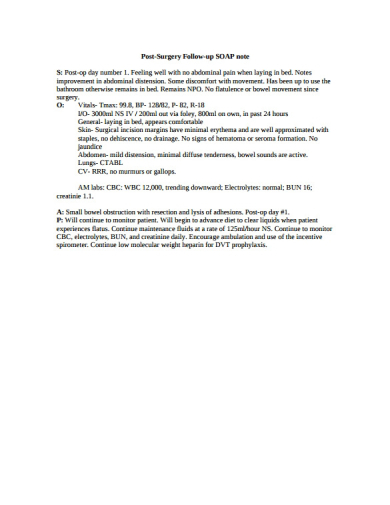
9. Post-Surgery Follow-Up Medical SOAP Note
What is the use of Medical SOAP Note?
In modern clinical practice, doctors share medical information primarily via oral presentations and written SOAP progress notes, which include histories, physicals and SOAP notes. SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
The Utility of Medical SOAP Notes:
Medical SOAP Notes are a universally recognized method for healthcare providers to document patient encounters in a clear, systematic, and efficient manner. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, each representing a critical component of the patient’s healthcare record.
Subjective:
This section captures the patient’s personal narrative of their symptoms and medical concerns. It includes the patient’s descriptions of pain, discomfort, the onset of symptoms, and their own perceptions of their health condition.
Objective:
Objective data encompasses measurable, observable, and reproducible findings during the clinical evaluation. This includes vital signs, physical examination results, laboratory data, and imaging findings.
Assessment:
The assessment is the healthcare provider’s professional diagnosis or interpretation of the patient’s condition based on the subjective and objective information gathered. It may also include differential diagnoses—other potential conditions that could present with similar symptoms.
Plan:
The plan outlines the next steps for managing the patient’s condition. This could involve ordering further tests, prescribing medications, initiating therapies, patient education, and scheduling follow-up visits.
Uses of Medical SOAP Notes:
- Continuity of Care: They provide a comprehensive record that ensures continuity of care across different healthcare providers and over time.
- Communication: SOAP notes facilitate clear communication among healthcare team members, which is essential for coordinated and effective patient care.
- Legal Documentation: These notes form part of the legal document that can be used in court, if necessary, to demonstrate the care provided to the patient.
- Billing and Coding: Accurate SOAP notes are crucial for billing and coding purposes, ensuring that healthcare providers are properly reimbursed for their services.
- Quality Assurance: They serve as a tool for healthcare facilities to perform quality assurance checks and improve healthcare services.
- Education and Research: SOAP notes are valuable for educational purposes, teaching students about patient care, and can be used in research to improve clinical outcomes.
SOAP Note Example for Speech-Language Pathologists (SLPs):
Subjective: The patient’s mother reports that he is struggling with pronouncing “r” sounds and becomes frustrated when he’s not understood by peers.
Objective:
- Articulation assessment reveals substitution of “w” for “r” in most positions.
- Difficulty with “r” sound noted in both isolated and conversational speech.
- Patient able to follow directions and demonstrates good receptive language skills.
Assessment: The patient exhibits developmental articulation disorder characterized by the consistent misarticulation of the “r” phoneme, known as rhotacism.
Plan: Target optimal voicing in functional environments with CTT techniques. Introduce additional compensatory strategies to manage vocal load across vocational and social settings.
- Initiate therapy focusing on the correct articulation of “r” sounds, starting with isolation and moving towards syllables, words, and conversational speech.
- Implement home practice program with exercises for daily practice.
- Schedule sessions twice a week for 30 minutes each.
- Reassess articulation skills in 4 weeks to monitor progress and adjust the therapy plan as needed.
This SOAP note outlines the patient’s concerns, the SLP’s objective findings, the assessment of the speech issue, and a clear plan for therapy moving forward.
Patients who have undergone surgery for a major or minor problem are likely to stay at the hospital at the doctor’s advice. That’s because some patients require post-surgery treatment due to a few complications, while others still need to be assessed during their recovery period to see whether the surgery was a success. Monitoring a patient during this time is crucial to one’s overall health. Thus, the SOAP notes made as a follow-up to the patient’s surgery must be written and studied carefully before any medical decisions are implemented.
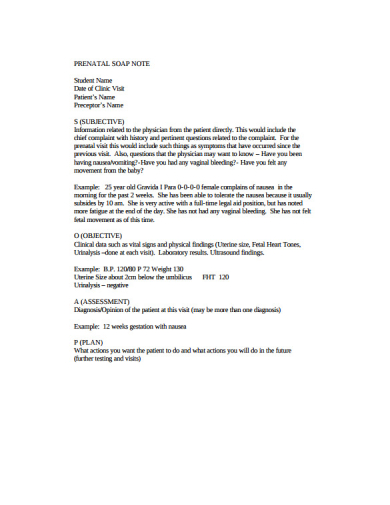
10. Prenatal Medical SOAP Note
How to sign a Medical SOAP Note?
Signing a Medical SOAP Note is an important step that validates the information within the note and identifies the healthcare provider responsible for the patient’s care at that time.
Here’s how to properly sign a Medical SOAP Note:
- Complete the Note: Ensure that all sections of the SOAP note (Subjective, Objective, Assessment, Plan) are filled out thoroughly and accurately.
- Review: Before signing, review the note to ensure that it accurately reflects the patient’s visit and that there are no omissions or errors.
- Identification: At the end of the SOAP note, provide your full name, professional title, and credentials. For example, “John Doe, MD” or “Jane Smith, RN.”
- Signature: Sign your name as you would on any official document. This can be a handwritten signature on a paper document or an electronic signature if the note is part of an Electronic Health Record (EHR) system.
- Date and Time: Include the date and time when the note was completed and signed. This is crucial for maintaining an accurate timeline of patient care.
- Contact Information: If it’s standard practice in your facility, include your contact information or extension number for easy follow-up if there are questions about the note.
- Co-Signature: If you are a medical student, intern, or resident, you may need a supervising physician to co-sign the note. Their signature validates the note and indicates their oversight. You may also see medical student SOAP Note.
Remember, the signature on a Medical SOAP Note is a legal attestation to the care provided, so it’s important to ensure the note is complete and accurate before adding your signature.
During your hospital trips to meet with an OB-GYN, you might have noticed your doctor take down a few notes for assessment. Patients are often asked to discuss the symptoms that they have experienced since their last prenatal visit. If the doctor notices something serious or alarming about these symptoms, you may be advised to undergo a few more tests to see if the baby is doing all right. This is necessary to make sure that the mother and her baby are taken care of for the duration of one’s pregnancy.
11. Simple Medical SOAP Note
Different Types of Therapy SOAP Note Examples:
Here are examples of SOAP notes for different types of therapy sessions:
Physical Therapy SOAP Note:
Subjective: The patient reports increased knee pain (6/10) when climbing stairs. States that the pain has been worsening over the past week.
Objective:
- Swelling noted around the right knee
- Limited range of motion: 0-90 degrees flexion
- Strength 3/5 in the right quadriceps muscle group
Assessment: The patient’s symptoms and examination are consistent with exacerbation of osteoarthritis in the right knee.
Plan:
- Continue with current physical therapy regimen
- Apply ice to reduce swelling
- Introduce low-impact exercises to strengthen the quadriceps
- Re-evaluate in one week
Occupational Therapy SOAP Note:
Subjective: The patient expresses frustration with difficulty in gripping objects, which affects the ability to dress independently.
Objective:
- Grip strength measured at 20 lbs, decreased from 30 lbs
- Difficulty manipulating buttons and zippers observed
Assessment: Decreased fine motor skills and hand strength likely due to recent wrist sprain.
Plan:
- Implement adaptive strategies for dressing
- Begin hand-strengthening exercises
- Use of assistive devices to improve grip
- Follow-up in one week to monitor progress
Speech Therapy SOAP Note:
Subjective: The patient’s parent reports that the child is stuttering more frequently, especially when excited or anxious.
Objective:
- Disfluencies observed in 15% of spoken sentences
- Tension noted in facial muscles during speech
Assessment: The patient’s stuttering appears to be exacerbated by anxiety and excitement.
Plan:
- Practice relaxation techniques prior to speaking
- Continue with fluency-shaping strategies
- Parental guidance on creating a supportive speaking environment
- Review progress in two weeks
Mental Health Therapy SOAP Note:
Subjective: The patient states feeling overwhelmed and anxious about upcoming exams, reporting difficulty sleeping.
Objective:
- Appears restless and has trouble maintaining eye contact
- Speaks rapidly and reports racing thoughts
Assessment: Symptoms suggest an increase in anxiety, possibly related to academic stress.
Plan:
- Explore stress-reduction techniques and coping strategies
- Discuss time management and study skills
- Consider referral for medication evaluation if no improvement
- Schedule weekly sessions for the next month
Massage Therapy SOAP Note for Back Pain & Stress Relief:
Subjective: The client reports chronic lower back pain, rating it a 7 out of 10 on the pain scale. They mention the pain increases after long periods of sitting at work. The client reports high levels of stress from work, leading to tension headaches and difficulty relaxing in the evenings.
Objective:
- Observation of slight lumbar lordosis.
- Palpation reveals tightness and tenderness in the lumbar paraspinal muscles.
- Limited range of motion during forward flexion due to discomfort.
- Muscle tightness observed in the trapezius and neck muscles.
- Client exhibits shallow breathing and inability to relax fully on the massage table.
Assessment: The client’s symptoms are indicative of muscle tension and possible myofascial trigger points in the lower back, contributing to the pain and limited mobility. The physical manifestations of stress are evident in muscle tightness, which may be contributing to the client’s tension headaches.
Plan:
- Focus on Swedish massage techniques for general relaxation.
- Apply deep tissue massage to the lumbar paraspinal muscles to reduce muscle tension.
- Use trigger point therapy to address specific areas of tightness.
- Recommend the client take stretch breaks during work hours and consider ergonomic adjustments to their workstation.
- Schedule a follow-up session in one week to reassess and continue treatment.
- Implement a full-body relaxation massage with an emphasis on the shoulders, neck, and scalp to alleviate muscle tension.
- Introduce aromatherapy with lavender oil to promote relaxation.
- Teach the client breathing exercises to use when feeling tense.
- Suggest scheduling regular bi-weekly massage sessions to manage stress levels and prevent the recurrence of tension headaches.
Each SOAP note reflects the unique aspects of the therapy provided, documenting the patient’s current status and the healthcare provider’s plan for treatment. They are tailored to the specific therapeutic area and the individual needs of the patient.
Difference between SOAP Note and Progress Note?
SOAP notes and progress notes are both fundamental tools used in documenting patient care, but they serve slightly different purposes and follow different structures.
Here’s a table differentiating the two:
| Feature | SOAP Note | Progress Note |
|---|---|---|
| Definition | A method of documentation employing a structured format that stands for Subjective, Objective, Assessment, and Plan. | A broader term for notes detailing the progress of a patient, which may or may not follow the structured SOAP format. |
| Purpose | To create a standardized and organized way of recording a patient encounter that includes specific clinical reasoning and a treatment plan. | To provide a chronological update on a patient’s status and developments during their care. |
| Structure | Highly structured around the four components: Subjective, Objective, Assessment, and Plan. | Can be more flexible in structure; may include SOAP elements but isn’t restricted to them. |
| Content | – Subjective: Patient’s reported symptoms and history.
– Objective: Observable data and findings. – Assessment: Diagnosis or evaluation of patient’s condition. – Plan: Treatment and management plan. |
Contains observations and updates on the patient’s condition, treatment response, and any changes to the management plan. Might include test results, medication adjustments, and patient feedback. |
| Frequency of Use | Typically used for each patient encounter or visit. | Can be written less frequently, such as in response to a significant change in condition or at regular intervals during a hospital stay. |
| Used By | Mainly by healthcare providers who need to document detailed findings and treatment plans after a clinical evaluation. | Used by any healthcare team member tracking the ongoing status or changes in the patient’s condition. |
| Legal Documentation | Often used as a legal document in medical records for audits, billing, and in cases of litigation. | Also used for legal documentation but may vary in the level of detail and standardization. |
| Typical Length | Can be longer due to the need to address all four components with enough detail for clinical reasoning. | May be shorter if only noting updates or significant changes without a full reassessment. |
| Focus on Treatment | The plan is a definitive part of the note, with clear next steps for treatment. | Treatment updates are included but may not be as detailed as the plan in a SOAP note. |
| Interdisciplinary Use | SOAP notes are mostly used by clinicians who are directly managing patient care. | Progress notes can be used and read by a multidisciplinary team, including nurses, therapists, and social workers. |
While both SOAP notes and progress notes are integral to patient care documentation, SOAP notes provide a more systematic approach to individual patient encounters, and progress notes offer a more fluid and continual update on the patient’s condition over time.
Who typically uses SOAP Medical Notes?
SOAP Medical Notes are typically used by a wide range of healthcare professionals including physicians, nurses, physical therapists, occupational therapists, mental health therapists, chiropractors, and other allied health providers to document patient encounters, track progress, and communicate care plans within the healthcare team.
What should be included in the Assessment portion of a SOAP Medical Note?
In the Assessment portion of a SOAP Medical Note, the healthcare provider should include their professional judgment about the patient’s condition, which may involve diagnosing the issue, understanding its severity, considering potential complications, and sometimes, listing differential diagnoses that could explain the symptoms.
How does the Plan section of a SOAP Note benefit patient care?
The Plan section of a SOAP Note benefits patient care by outlining the next steps for treatment, including medications, therapies, tests, patient education, and follow-up appointments. It ensures a structured approach to managing the patient’s condition, promoting consistency and continuity in care, and facilitating clear communication among healthcare providers.
In what way does the Assessment help in planning patient treatment?
The Assessment in a SOAP note helps in planning patient treatment by providing a diagnosis or a list of possible diagnoses based on the subjective and objective information gathered. It guides the healthcare provider in selecting the most appropriate treatment options and interventions tailored to the patient’s specific health needs.
What is the significance of the Objective data in a SOAP Note?
The Objective data in a SOAP Note is significant because it provides unbiased, measurable facts about the patient’s current health status. This includes vital signs, examination findings, lab results, and imaging studies, which are crucial for making an accurate diagnosis and monitoring the progress of the patient’s condition over time.
How to use SOAP notes with your practice management system
To use SOAP notes with your practice management system, input notes directly into the patient’s electronic health record during or after the encounter. Utilize templates or standardized fields to ensure consistency. Regularly update and review notes to reflect the current status and treatment plans, ensuring seamless integration with billing and scheduling modules.
Most hospitals and clinics follow a standard format when it comes to producing a medical SOAP note. Apart from maintaining consistency, this also makes it easier for healthcare providers to read and find what they need from the document. The content of the note must be relevant and specific to the matter at hand, which is why most doctors and nurses try to simplify these records as much as they can. Fortunately, medical professionals are trained to report and understand these notes to ensure the proper treatment of patients.