Counseling SOAP Note Examples to Download
Counseling is an important job to maintain a person’s mental health. Some stressful situations in life can negatively impact individuals causing them to undergo a life crisis. In these situations, people tend to seek help from professionals in dealing with their problems. As a counselor, it is your responsibility and obligation to write a detailed counseling SOAP note.
3+ Counseling SOAP Note Examples
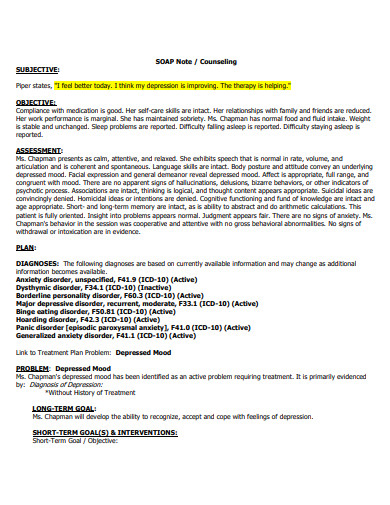
1. Counseling SOAP Note Template
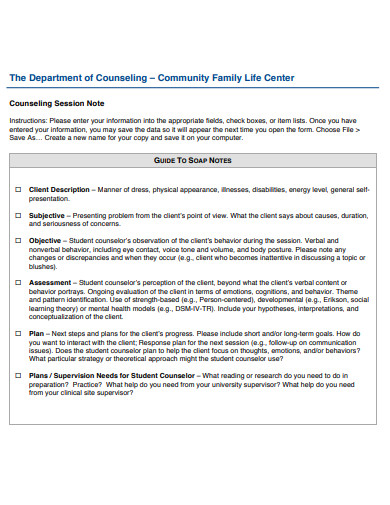
2. Basic Counseling SOAP Note
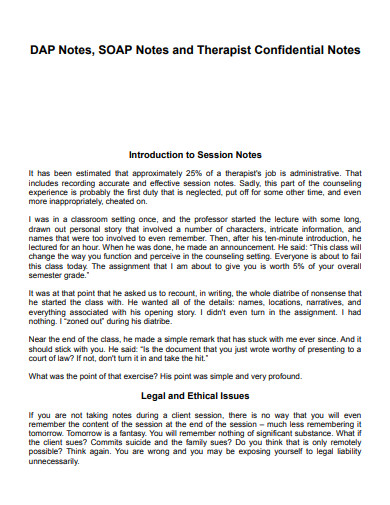
3. Confidential Counseling SOAP Note
4. Counseling SOAP Note in PDF
What Is a Counseling SOAP Note?
A soap note is a necessary document in counseling that details the information a counselor would gather during the whole session with a client. SOAP is an acronym that stands for subjective, objective, assessment, and plan. It is a narrative report that aims to provide documentation of the problems the client is experiencing.
How to Devise a Detailed Counseling Soap Note
Counseling therapy notes are necessary medical records. To make this paper as specific and instructive as possible, you need to compose it by following the appropriate SOAP framework and format. That said, there are several things to take into account in each letter of that acronym. Learn helpful tips on the steps below.
1. Provide a Subjective Description
The first part is the segment where you discuss the clients’ descriptions of their symptoms. You can get this data by asking your clients how they are doing at the beginning of your session. It is advisable to quote their statements directly. That said, you should also include the subjective data they provide regarding their status, progress, their ongoing problems, and their short-term goals for the upcoming sessions.
2. Supply Objective Records
In contrast to the subjective segment, the data in these records would mostly come from you. Your approach in writing your therapy progress note in this step should be objective. How’s their mental health status? Answer that in this record. You should include essential details that you got from the duration of your therapy schedule.
3. Document Your Assessment
This part is where you should analyze and incorporate the data you gathered in both the objective and subjective description. You should interpret the data and include clinical assessment. In addition, you should also provide your professional opinion and the possible factors that mainly influenced your patient’s progress.
4. Discuss Your Plan
After taking everything into account, the last part of this framework is to discuss your recommended action plan. In this procedure, you should create an outline detailing the treatment plan that your client should undergo. Also, if you want to make revisions to the treatment goals, this is the part to discuss them.
FAQs
What makes a SOAP note effective?
A SOAP note is instructive when it documents each letter of the acronym in detail. That said, it should include essential descriptive details of the subjective and objective findings. In addition, it should also outline assessment results and a therapy plan. Remember to keep your notes brief and concise, but remember to maintain necessary therapy information.
When can you use SOAP notes?
Following the SOAP framework is a famous practice for healthcare and psychology practitioners. This procedure in note-taking serves as a guide for the care providers. Especially in regards to the details to write on the medical note and how to organize them. That said, you can use soap notes in writing down essential medical papers for various medical practices.
Why is a counseling SOAP note necessary?
Writing a soap note after counseling is essential to keep track of the progress of the patient. This document details necessary information regarding changes in the client’s behavior and perception in each session. Taking down therapy notes is one of the most crucial records of the interaction between the counselor and the client.
Each session in counseling requires efforts from both the professional and the patient. Recording the progress of your clients would help you determine how far you are in achieving your goals. In addition, it would help you identify the glaring problems that you should focus on solving. The best way to do this is by regularly writing detailed counseling soap notes every session.