5+ Psychiatric SOAP Note Examples to Download
SOAP notes are communication documents written with the description of a patient’s condition. These are necessary between health care workers like physicians, psychiatrists and other medical specialties. We may have encountered this type of document, but we do not know its uses and how it is made. In this article, we will be talking about mental health. In psychology and psychiatry, writing SOAP notes must be clear and concise because it involves patients’ information which essential for his or her continuum of care. Read the entire article to know more about psychiatric SOAP notes and how to create one.
5+ Psychiatric SOAP Note Examples
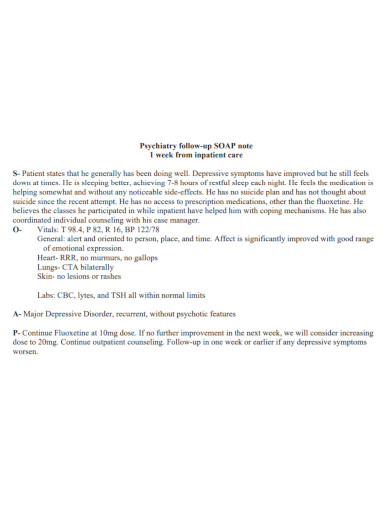
1. Psychiatry Follow-Up SOAP Note
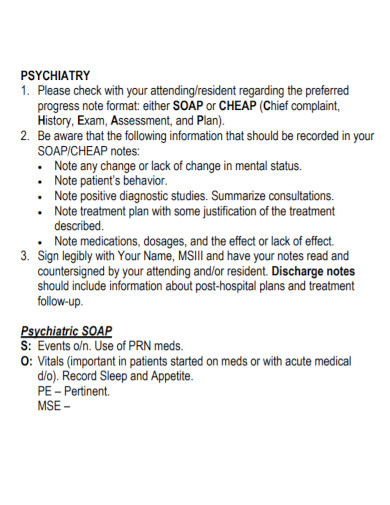
2. Psychiatric Clerkship SOAP Note
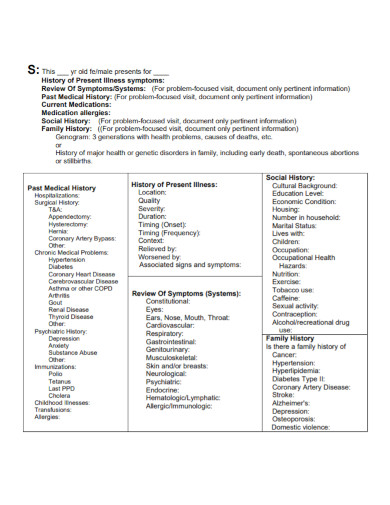
3. Psychiatric SOAP Note Format
4. Psychiatric SOAP Note Template
5. Syllabus Psychiatric SOAP Note
6. Basic Psychiatric SOAP Note
All the notes that you will be taking will determine the quality of care you give to the patients. It takes time to master the skill of creating comprehensive notes that are easy to use especially for other medical professionals. SOAP notes are among the most effective method to use in behavioral health and medical-related documents.
What are SOAP Notes?
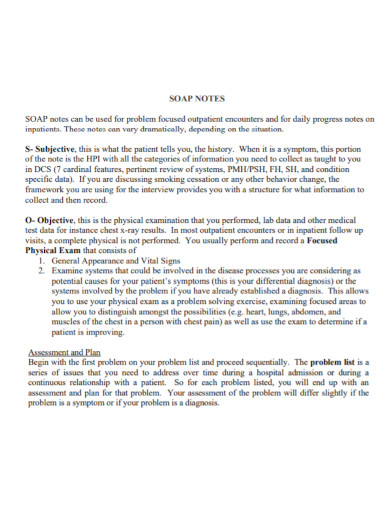
SOAP stands for Subjective, Objective, Assessment and Plan. This is a kind of document that keeps track or record about the condition of a particular patient. These four components should be the basis when gathering information for a patient’s treatment.
Subjective
This is the first step in writing SOAP notes. In this section, you are going to gather information about the complaints or symptoms that a client experienced. This will also be the time when you are able to know what are the other needs of the patient with regards to their treatment. The subjective summary must include a statement from the client which may serve as an insight into their condition. You may also be required to place the comments from your patients, their family or their caretakers. Upon presenting the problem, you may use the following elements: Onset, Location, Duration, Characterization, Alleviating Factors, Radiation, Temporal Pattern and Severity.
Onset – the day or time when the symptom started
Location – primary location of pain
Duration – time period that the patient dealt with the symptom
Characterization – the type of pain
Alleviating Factors – actions that contribute to the severity of the pain or symptom
Radiation – an instance if the pain radiates to other parts of the body
Temporal pattern – tells whether the symptoms only occur at night or after a meal
Severity – tells how severe the pain is
Objective
These contains detailed observation of the patient’s behavior, appearance, mood and body language. You should only write facts and provide raw data.
Assessment
This is where you are going to put your impressions and interpretations based on the information you have gathered. This may or may not include the diagnosis. For common mental issues, the assessment can lead into a diagnosis in the first or second visit. In case of rare mental issues, you may take more time to gather information on the subjective and objective section before you arrive for a diagnosis.
Just like any other SOAP notes, your assessment should only contain relevant details. This may be longer than the other sections.
Plan
This contain information on the treatment you gave during the session, the patient’s response to the treatment, the schedule for next appointment, the instructions you gave to the patient and the outcome measures. The goal of this section is to make plans about the patient’s continuing treatment.
Tips in Writing SOAP Notes
Make sure that you take down notes for data gathering. Use template to save time and to focus on the content quality rather than the structure. Keep your information concise and specific. Avoid jargons and irrelevant abbreviations that will lead to confusion. The person that should be mentioned in the document is the name of the patient only. Wrap up you SOAP notes after.
FAQs
Who uses SOAP notes?
It is commonly used by doctors, nurses, pharmacists, therapists and other healthcare workers.
What is the benefit of using SOAP notes?
The benefit of a SOAP note is to help organize information or data such that it will be placed in areas that makes it easy to find.
Is patient history subjective or objective?
It is written in the subjective section. Subjective section includes the patient’s demographic information and their history of medical conditions.
Psychiatric SOAP notes are documents involving patients with mental health problems. They are progressive notes that contains a reminders of the kind of information that mental health workers should collect to provide the patient with the right treatment.