19+ Principles of Therapeutic Communication Examples
What are Principles of Therapeutic Communication?
The principles of therapeutic communication are guidelines that healthcare professionals follow to enhance their interactions with patients. These principles aim to create a supportive, empathetic, and understanding dialogue that promotes healing and trust. Key principles include active listening, showing empathy, being non-judgmental, maintaining confidentiality, and providing clear and honest information. These guidelines help in building a strong, trusting relationship between the caregiver and the patient, ensuring the communication is beneficial for the patient’s mental, emotional, and physical well-being. They are essential in all areas of healthcare to ensure effective and compassionate patient care.
20 Principles of Therapeutic Communication
Therapeutic communication in healthcare is more than just a conversation; it’s a strategic approach to enhancing patient care. This guide outlines 20 key principles that are foundational to effective communication in medical settings. Each principle not only facilitates better dialogue but also strengthens the caregiver-patient relationship, ensuring that patients feel heard, understood, and respected. These principles cover a range of techniques, from empathetic listening to clear and respectful information sharing, and are essential for any healthcare professional aiming to provide high-quality, patient-centered care.
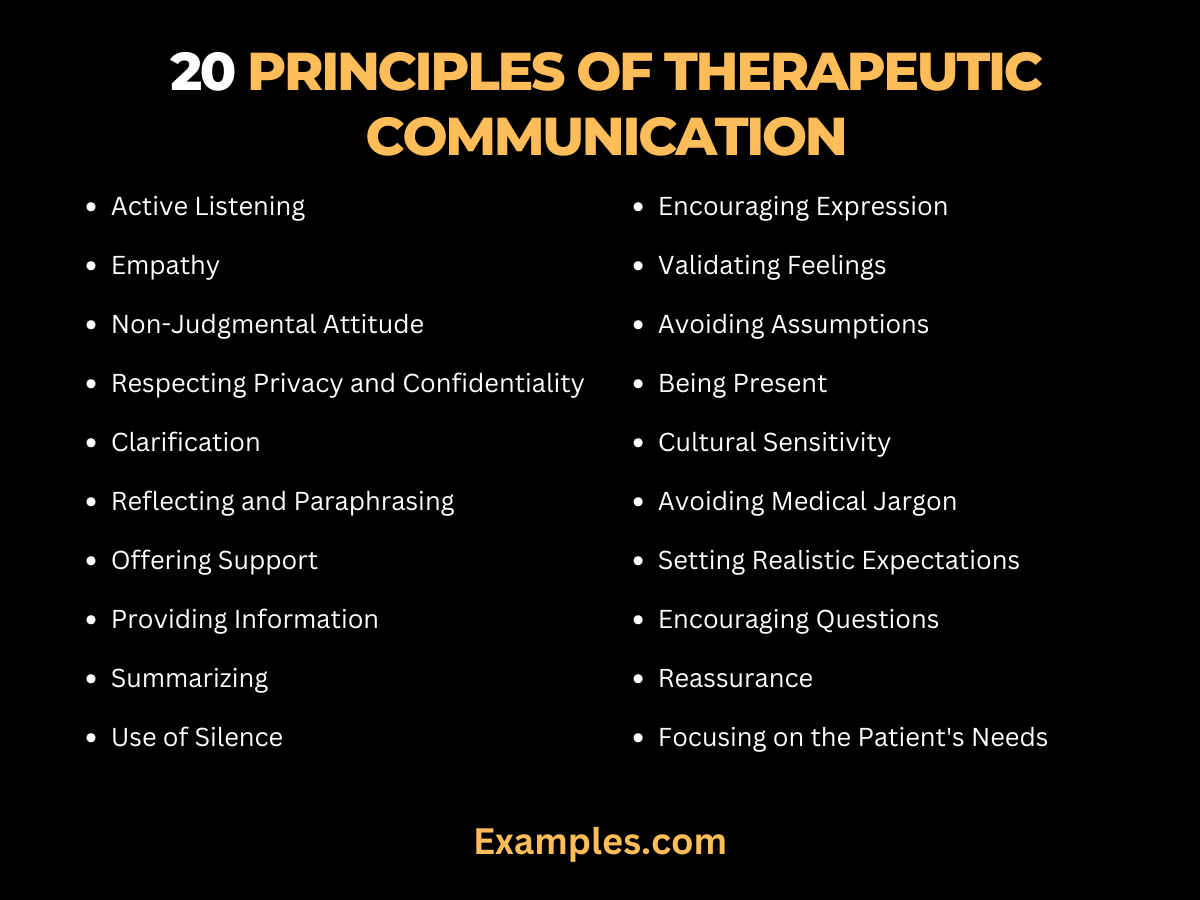
- Active Listening: Involves not just hearing words but also understanding the emotions and meanings behind them, essential for effective communication.
- Empathy: This is about genuinely understanding and sharing the feelings of the patient, creating a connection that transcends mere words.
- Non-Judgmental Attitude: It’s important to create a space where patients feel safe to express themselves without fear of judgment or criticism.
- Respecting Privacy and Confidentiality: Maintaining patient confidentiality is not only a legal requirement but also a cornerstone of trust in healthcare.
- Clarification: Asking questions and rephrasing ensures that both the healthcare provider and the patient are on the same page, avoiding miscommunication.
- Reflecting and Paraphrasing: By reflecting or paraphrasing, healthcare providers show patients that their words are being carefully considered.
- Offering Support: This principle is about being there for the patient, both emotionally and physically, throughout their healthcare journey.
- Providing Information: Giving patients clear and accurate information empowers them to make informed decisions about their health.
- Summarizing: A summary helps both the patient and the healthcare provider to focus on key aspects of the conversation and plan accordingly.
- Use of Silence: Silence can be a powerful tool, giving patients time to process information and gather their thoughts.
- Encouraging Expression: Allowing patients to express their feelings and thoughts openly can provide valuable insights into their health and well-being.
- Validating Feelings: Acknowledging and validating a patient’s feelings can help them feel supported and understood.
- Avoiding Assumptions: Each patient is unique, and assumptions can lead to misunderstandings and ineffective care.
- Being Present: This means giving patients undivided attention, showing them that they are the primary focus during the interaction.
- Cultural Sensitivity: Understanding and respecting cultural differences is key to effective and respectful communication.
- Avoiding Medical Jargon: Using simple, clear language ensures that patients understand their health conditions and the proposed treatments.
- Setting Realistic Expectations: Clear communication about what to expect can help manage patient anxiety and improve treatment compliance.
- Encouraging Questions: Questions from patients are a sign of engagement and understanding, and should be encouraged.
- Reassurance: Comforting patients can ease their anxiety and build a sense of trust and safety.
- Focusing on the Patient’s Needs: Tailoring communication to meet the specific needs of each patient ensures that they feel valued and cared for.
Principles of Therapeutic Communication in Nursing
Therapeutic communication in nursing is a foundational element of patient care, pivotal for building rapport, understanding patient needs, and delivering effective healthcare. This comprehensive guide delves into the principles of therapeutic communication specific to nursing, emphasizing how these practices can significantly enhance patient interactions and outcomes.

Active Listening and Empathy
Active listening and empathy are at the heart of therapeutic communication in nursing. Nurses must attentively listen to patients’ verbal and nonverbal cues to fully understand their concerns and feelings. This involves not just hearing the words but also comprehending the emotions behind them. Empathy allows nurses to connect with patients on a deeper level, showing that they care and understand, which can be particularly comforting in times of stress or illness.
Clear and Honest Communication
Clarity and honesty in communication are crucial. Nurses should communicate medical information and care plans in a straightforward, jargon-free manner, ensuring patients understand their health status and treatment options. Being honest, even when conveying difficult news, helps in building trust and integrity in the nurse-patient relationship.
Cultural Sensitivity and Personalization
Recognizing and respecting cultural differences in communication styles and preferences is essential. Nurses should tailor their communication approach to align with the cultural, linguistic, and personal backgrounds of their patients, ensuring inclusive and sensitive care.
Maintaining Confidentiality and Professional Boundaries
Confidentiality is a key ethical principle in nursing. Respecting patient privacy and maintaining discretion in all communications fosters trust and respect. Additionally, nurses should balance empathy with professional boundaries, ensuring a supportive yet professional relationship.
Patient Education and Empowerment
Nurses play a significant role in patient education. By effectively communicating health information, they empower patients to make informed decisions about their care and treatment. This involves simplifying complex medical information, encouraging patient questions, and ensuring they understand the implications of different treatment options.
Providing Emotional Support and Reassurance
Offering emotional support and reassurance is another important aspect of therapeutic communication. Nurses should recognize and address the emotional and psychological needs of patients, providing comfort and reassurance during challenging times.
Utilizing Nonverbal Communication
Nonverbal cues, such as body language, facial expressions, and eye contact, are powerful tools in therapeutic communication. Nurses can use these cues to convey compassion, understanding, and attentiveness, often speaking louder than words.
Feedback and Follow-Up
Effective communication in nursing also involves giving and receiving feedback. Nurses should encourage patients to share their thoughts and feelings about their care and be open to feedback to improve their communication strategies. Regular follow-up conversations can also help in monitoring progress and adjusting care plans as needed.
Ethical Principles of Therapeutic Communication
Ethical principles in therapeutic communication are foundational in establishing trust and integrity within healthcare interactions. These principles guide healthcare professionals in conducting conversations that respect patient dignity, privacy, and autonomy. This comprehensive guide explores the critical ethical principles that underpin therapeutic communication, ensuring that patient interactions are not only effective but also adhere to high ethical standards.

Respecting Patient Autonomy
One of the foremost ethical principles is respecting patient autonomy. This involves acknowledging and supporting patients’ rights to make informed decisions about their care. Communicating in a way that empowers patients to express their wishes and choices is vital. For instance, when discussing treatment options, it’s important to present information clearly and neutrally, allowing patients to make decisions based on their values and preferences.
Upholding Confidentiality
Confidentiality is a cornerstone of therapeutic communication. It’s essential to maintain the privacy of patient information, ensuring that discussions and medical records are kept secure and private. This principle builds trust and encourages patients to share openly without fear of their personal information being disclosed inappropriately.
Practicing Non-Maleficence and Beneficence
Non-maleficence and beneficence are twin pillars in healthcare ethics, emphasizing the need to do no harm and to act in the best interests of the patient. In therapeutic communication, this means being cautious about the language used, avoiding causing distress or misunderstanding, and ensuring that the communication is always aimed at benefiting the patient.
Ensuring Veracity
Veracity, or truthfulness, is crucial in building a transparent and trusting relationship between healthcare providers and patients. This involves providing accurate information, being honest about diagnoses and prognoses, and avoiding misleading or withholding information. Practicing veracity helps in making informed decisions and setting realistic expectations.
Demonstrating Cultural Sensitivity
Cultural sensitivity is increasingly recognized as an essential aspect of ethical therapeutic communication. This involves understanding and respecting cultural differences in values, beliefs, and communication styles. Healthcare providers should strive to be culturally competent, tailoring their communication to be respectful and relevant to each patient’s cultural background.
Commitment to Professionalism
Professionalism in communication is about maintaining a respectful, empathic, and appropriate demeanor. It involves adhering to the standards of the profession, including ethical guidelines and boundaries in patient interactions. Professionalism ensures that the therapeutic relationship remains beneficial and supportive.
Balancing Empathy with Boundaries
Empathy is a key component of therapeutic communication, but it must be balanced with professional boundaries. Healthcare providers should strive to understand and share patients’ feelings while maintaining an appropriate professional distance. This balance is crucial in providing compassionate care without overstepping professional limits.
Ensuring Informed Consent
Informed consent is an ethical and legal requirement. It involves making sure that patients understand their treatment options and the potential risks and benefits. Effective therapeutic communication is essential in this process, as it helps patients to make informed decisions about their care.
What are the Principles of Therapeutic Effects?
Therapeutic effects in healthcare revolve around the positive outcomes achieved through effective treatment and communication strategies. The principles underlying these effects include a blend of clinical expertise, patient-centered care, and empathetic communication. This guide dives deep into these principles, highlighting how each contributes to successful therapeutic outcomes.
- Evidence-Based Practice: Integrating the best current research with clinical expertise to make patient care decisions. This approach ensures treatments are grounded in solid scientific evidence, enhancing their effectiveness.
- Individualized Care: Tailoring treatment and communication strategies to meet the unique needs of each patient. Recognizing individual differences in health conditions, preferences, and responses to treatment is crucial for maximizing therapeutic effects.
- Empathetic Communication: Using therapeutic communication techniques to understand and empathize with patients’ experiences and emotions. This kind of communication fosters a supportive environment, which is key to patient healing and well-being.
- Collaborative Decision-Making: Involving patients in their own care decisions to empower them and improve treatment adherence. When patients are active participants in their care, they are more likely to follow through with treatment plans and report better outcomes.
- Holistic Approach: Considering the physical, emotional, and psychological aspects of patient health in treatment planning. This comprehensive view ensures that all aspects of a patient’s well-being are addressed, leading to more effective therapeutic outcomes.
What are the Principles of Therapeutic Nurse-Patient Relationship?
The therapeutic nurse-patient relationship is fundamental in nursing and is built on several key principles that promote healing, trust, and effective care. This relationship is at the heart of nursing practice, and understanding these principles is essential for any nurse seeking to provide high-quality care.
- Trust: Establishing a foundation of trust is the first step in a therapeutic nurse-patient relationship. Trust is built through consistent, reliable, and honest communication, as well as through the demonstration of professional competence.
- Empathy: Demonstrating empathy towards patients helps nurses to understand and relate to their experiences. This empathetic approach fosters a deeper connection and a more meaningful nurse-patient relationship.
- Respect for Patient Autonomy: Respecting patients’ rights to make decisions about their own care is a fundamental principle. This involves acknowledging and supporting patients’ choices and preferences.
- Confidentiality: Maintaining confidentiality is vital in establishing trust. Patients need to feel confident that their personal and health information is secure and protected.
- Professional Boundaries: Understanding and maintaining professional boundaries is crucial. While empathy and compassion are important, it is also necessary to keep the relationship professional to ensure objective and effective care.
- Effective Communication: Clear, honest, and compassionate communication forms the backbone of the therapeutic nurse-patient relationship. This includes not only verbal communication but also non-verbal cues and active listening.
- Cultural Competence: Being culturally competent and sensitive to the diverse backgrounds and beliefs of patients is essential in modern nursing. This ensures that care is respectful, relevant, and responsive to patients’ cultural needs.
- Patient-Centered Care: Placing the patient at the center of care planning and decision-making. This involves considering their individual needs, values, and preferences in all aspects of their care.
In summary, the principles of therapeutic effects and the therapeutic nurse-patient relationship are centered on empathy, respect, patient involvement, and effective communication. These principles guide healthcare providers in delivering care that is not only clinically effective but also emotionally supportive and respectful of patient needs and preferences.