49+ Nonverbal Communication for Nurses Examples
In the realm of nursing, mastering nonverbal communication is as crucial as any medical skill. This complete guide delves into the nuanced world of nonverbal communication for nurses, providing a wealth of nonverbal communication examples to enhance your understanding. From facial expressions to body language, discover how these silent signals can significantly impact patient care. Whether you’re a seasoned nurse or a novice in the field, this guide offers invaluable insights into the art of nonverbal interaction in healthcare settings.
What is Nonverbal Communication in Nursing? – Definition
Nonverbal communication in nursing involves conveying messages without spoken words. It includes body language, facial expressions, and gestures, crucial for effective nonverbal communication in healthcare. This form of communication is essential in nursing, as it helps convey empathy and understanding, building trust between nurses and patients. It’s particularly significant in scenarios where nonverbal communication for pain assessment is required, offering an alternative way to understand patients’ needs.
What is the Best Example of Nonverbal Communication for Nurses?
A prime example of nonverbal communication for nurses is using empathetic facial expressions and attentive body language. A nurse’s reassuring smile, coupled with direct eye contact, exemplifies nonverbal communication skills in nursing. This approach is not only comforting but also builds a rapport, essential in nonverbal communication in daily life of a healthcare setting. Such nonverbal cues are crucial in showing support and compassion, often having a more significant impact than verbal communication in patient care.
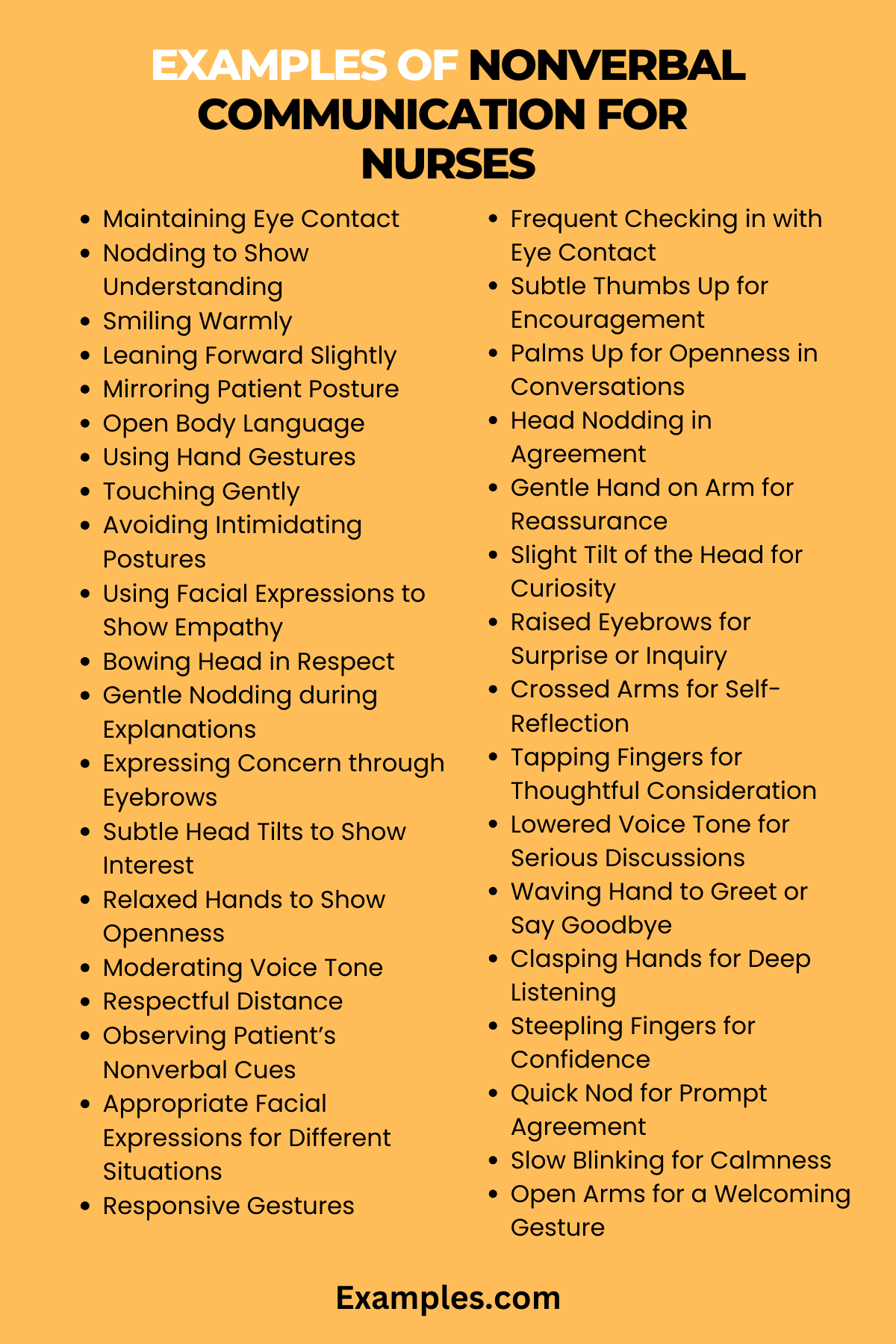
50 Examples of Nonverbal Communication for Nurses
Nonverbal communication is a vital aspect of nursing, offering a profound way to connect with patients beyond words. This guide focuses on 50 unique and distinct examples of nonverbal communication for nurses, enriched with detailed explanations and how-to-communicate example sentences. Emphasizing key aspects like empathy, attentiveness, and cultural sensitivity, these examples are crafted to enhance patient care and understanding in diverse healthcare settings, underscoring the importance of nonverbal communication in nursing.
- Maintaining Eye Contact: By holding eye contact, nurses show they are fully engaged and listening.
Example: When a patient is speaking, maintain steady eye contact to convey, “I am here with you and for you.” - Nodding to Show Understanding: A simple nod can reassure the patient that their concerns are being heard.
Example: As a patient explains their symptoms, nod subtly to signal, “I understand what you’re saying.” - Smiling Warmly: A warm smile can be comforting, especially in stressful situations.
Example: Greet your patient with a gentle smile to convey, “You are in a safe and caring environment.” - Leaning Forward Slightly: This posture indicates attentiveness and interest.
Example: Lean in slightly during conversations to show, “I am focused on your care.” - Mirroring Patient Posture: Reflecting a patient’s posture can create rapport and empathy.
Example: If a patient is sitting relaxed, mirror their posture to communicate, “I am with you in this experience.” - Open Body Language: Keeping arms uncrossed and posture open demonstrates receptiveness.
Example: Maintain open body language when discussing care plans, signaling, “I am open to your thoughts and concerns.” - Using Hand Gestures: Hand gestures can aid in explaining medical procedures or instructions.
Example: Use clear hand movements to describe a procedure, making it easier for the patient to understand. - Touching Gently: Appropriate, gentle touch can be very reassuring.
Example: A light touch on the shoulder can signify, “I am here to support you.” - Avoiding Intimidating Postures: Avoiding towering over or standing too close to the patient.
Example: Stand at a comfortable distance, ensuring, “You are in a safe space.” - Using Facial Expressions to Show Empathy: Expressions like a furrowed brow or a soft smile can communicate empathy.
Example: Show concern through your facial expression when a patient expresses discomfort, signifying, “I hear your concern.” - Bowing Head in Respect: A slight bow can show respect for the patient’s condition or feelings.
Example: Bow your head lightly when a patient shares something personal, indicating, “I respect your privacy and feelings.” - Gentle Nodding during Explanations: Nodding gently while explaining care plans or procedures.
Example: As you explain a treatment, nod to emphasize key points, showing, “This information is important for your care.” - Expressing Concern through Eyebrows: Raised eyebrows can express concern or surprise.
Example: Raise your eyebrows slightly when a patient reveals a sudden symptom, conveying, “I am concerned about this new development.” - Subtle Head Tilts to Show Interest: Tilting the head slightly can demonstrate you are actively listening.
Example: Tilt your head when a patient speaks about their feelings, indicating, “I am genuinely interested in what you are saying.” - Relaxed Hands to Show Openness: Keeping hands relaxed at your sides or in front to appear approachable.
Example: Keep your hands relaxed during interactions to signify, “I am approachable and here to help.” - Moderating Voice Tone: Using a calm, gentle voice tone to soothe and reassure.
Example: Speak in a soft, calm tone when addressing a patient’s concerns, suggesting, “I am here to calm and reassure you.” - Respectful Distance: Maintaining a respectful physical distance while interacting.
Example: Stand at an arm’s length to respect the patient’s personal space, conveying, “I respect your comfort zone.” - Observing Patient’s Nonverbal Cues: Paying close attention to a patient’s own nonverbal communication.
Example: Notice if a patient leans away or looks uncomfortable and adjust accordingly, showing, “I am attentive to your comfort.” - Appropriate Facial Expressions for Different Situations: Adjusting your facial expressions according to the context of the conversation.
Example: Show a concerned expression when discussing serious matters, indicating, “I understand the gravity of this situation.” - Responsive Gestures: Using gestures like nodding or tilting the head in response to patient queries.
Example: Nod affirmatively when a patient asks a question, showing, “I acknowledge your query.” - Frequent Checking in with Eye Contact: Regular eye contact during care shows attentiveness.
Example: Make eye contact frequently while administering medication, signaling, “I am fully focused on your care.” - Subtle Thumbs Up for Encouragement: A thumbs-up gesture can provide positive reinforcement.
Example: Give a small thumbs-up after a successful procedure to convey, “You did well.” - Palms Up for Openness in Conversations: Presenting palms up during discussions shows openness.
Example: Use palms-up gestures when asking about a patient’s feelings, indicating, “I am open to hearing about your experience.” - Head Nodding in Agreement: Nodding in agreement to affirm patient’s statements.
Example: Nod in agreement when a patient expresses concerns, showing, “I validate your feelings.” - Gentle Hand on Arm for Reassurance: A light hand on the arm can comfort.
Example: Place a gentle hand on the arm when a patient is anxious, reassuring, “You are not alone.” - Slight Tilt of the Head for Curiosity: Tilt your head to show curiosity and engagement.
Example: Tilt your head when a patient describes unusual symptoms, suggesting, “I am intrigued and want to understand more.” - Raised Eyebrows for Surprise or Inquiry: Use raised eyebrows to express surprise or ask questions.
Example: Raise your eyebrows when a patient mentions something unexpected, indicating, “That’s interesting, tell me more.” - Crossed Arms for Self-Reflection: Cross arms when pondering or reflecting, showing deep thought.
Example: Cross your arms while considering a patient’s condition, conveying, “I am deeply contemplating the best course of action.” - Tapping Fingers for Thoughtful Consideration: Tap fingers lightly when thinking or making decisions.
Example: Tap your fingers lightly when discussing treatment options, signifying, “I am carefully considering each possibility.” - Lowered Voice Tone for Serious Discussions: Lower your voice tone during critical conversations.
Example: Use a lower voice tone when discussing serious diagnoses, suggesting, “This is a significant matter.” - Waving Hand to Greet or Say Goodbye: A friendly wave can be welcoming or comforting.
Example: Wave lightly when a patient arrives or leaves, indicating, “You are welcomed here.” - Clasping Hands for Deep Listening: Clasp your hands together while listening intently.
Example: Clasp your hands when a patient shares complex emotions, showing, “I am fully attentive to your story.” - Steepling Fingers for Confidence: Steeple your fingers to show confidence and authority.
Example: Steeple your fingers when explaining a crucial point, conveying, “I am confident in this information.” - Quick Nod for Prompt Agreement: A quick nod can show immediate agreement or understanding.
Example: Give a quick nod when a patient makes a straightforward request, indicating, “I agree and will act promptly.” - Slow Blinking for Calmness: Slowly blink to convey a sense of calm and patience.
Example: Blink slowly when a patient is upset, suggesting, “I am calm and here to help you relax.” - Open Arms for a Welcoming Gesture: Open arms to express a welcoming and inclusive attitude.
Example: Extend open arms when introducing a new treatment plan, indicating, “I am welcoming your input and participation.” - Squinting Eyes for Concentration: Squint slightly to show concentration and focus.
Example: Squint your eyes while examining patient data, conveying, “I am closely analyzing this information.” - Pointing for Direction or Emphasis: Point to direct attention or emphasize key points.
Example: Point to areas on a chart to highlight important health trends, suggesting, “This is crucial for your understanding.” - Winking for Encouragement or Agreement: Occasionally wink to show encouragement or shared understanding.
Example: Wink lightly after a patient makes a light-hearted joke, indicating, “I appreciate your sense of humor.” - Shaking Head for Disagreement or Concern: Shake your head when expressing concern or disagreement.
Example: Shake your head gently when debunking a medical myth, conveying, “That’s not quite accurate.” - Tapping Foot for Urgency: Tap your foot to express urgency or the need to act swiftly.
Example: Tap your foot lightly when time is critical, signaling, “We need to move quickly.” - Frowning in Sympathy or Concern: Frown to show sympathy or concern for a patient’s situation.
Example: Frown slightly when a patient shares distressing news, showing, “I empathize with your situation.” - Rubbing Chin for Thoughtfulness: Rub your chin when pondering or considering options.
Example: Rub your chin while discussing potential treatment paths, indicating, “I am thoughtfully considering each option.” - Pursed Lips for Disapproval or Uncertainty: Pursed lips can signify disapproval or uncertainty.
Example: Pursed your lips when you are uncertain about a patient’s self-diagnosis, suggesting, “I’m not sure that’s correct.” - Hand Over Heart for Sincerity or Empathy: Place your hand over your heart to show sincerity or empathy.
Example: Place your hand over your heart when expressing condolences or empathy, signaling, “I truly feel for you.” - Wide Eyes for Surprise or Realization: Widen your eyes to express surprise or sudden realization.
Example: Widen your eyes when a patient reveals an unexpected health improvement, showing, “That’s fantastic news!” - Cupping Ear for Active Listening: Cup your ear to show you are actively listening or to encourage the patient to speak up.
Example: Cup your ear when a patient speaks softly, indicating, “I am listening closely.” - Blinking Rapidly for Surprise or Alarm: Blink rapidly to express surprise or alarm.
Example: Blink rapidly when a patient describes an alarming symptom, conveying, “I am surprised and taking this seriously.” - Hands on Hips for Readiness or Determination: Place hands on hips to show readiness or determination.
Example: Put your hands on your hips when preparing for an urgent procedure, suggesting, “I am ready and determined.” - Patting Back for Comfort or Encouragement: Gently pat a patient’s back for comfort or encouragement.
Example: Pat a patient’s back lightly after a difficult procedure, indicating, “You did well, and I’m here for you.”
Methods of Nonverbal Communication for Nurses
Understanding and effectively using nonverbal communication methods is a vital skill for nurses. These methods encompass a range of behaviors and actions that can significantly impact patient care and communication. Here are some key nonverbal methods that nurses can employ:
- Facial Expressions: A nurse’s facial expressions can convey a multitude of emotions, from empathy and concern to happiness and reassurance. These expressions are often the first thing a patient notices.
- Body Language: The way a nurse stands, sits, or moves can communicate confidence, openness, or comfort. Body posture is a powerful tool in nonverbal communication, especially in nonverbal communication for nurses.
- Gestures: Hand gestures can be used to direct attention, demonstrate care procedures, or simply to communicate more effectively with patients.
- Eye Contact: Maintaining appropriate eye contact is essential in building trust and rapport with patients. It shows attentiveness and interest in what the patient is saying or experiencing.
- Touch: When appropriate, touch can be a powerful tool for comforting patients. A reassuring pat on the back or a gentle touch on the arm can provide a sense of safety and care.
- Proximity: The physical distance a nurse maintains with a patient can communicate comfort and respect for personal space, or closeness and empathy.
- Silence: Sometimes, silence can be a powerful form of communication, providing a patient with time to think or demonstrating patience and understanding from the nurse.
By mastering these methods, nurses can enhance their ability to connect with and support their patients, making nonverbal communication for nurses a cornerstone of excellent patient care.
Nonverbal Communication Tips For Nurses
Nonverbal communication is a nuanced and vital aspect of nursing. Here are some tips to help nurses improve their nonverbal communication skills:
- Be Conscious of Your Own Nonverbal Cues: Self-awareness is key. Understand how your own body language, facial expressions, and gestures can be perceived.
- Learn to Read Patient’s Nonverbal Cues: Patients often communicate their feelings and needs nonverbally, especially in situations where they cannot express themselves verbally.
- Practice Cultural Sensitivity: Be aware of cultural differences in nonverbal communication. What is considered comforting in one culture may be perceived differently in another.
- Match Nonverbal Communication with Verbal: Ensure that your nonverbal cues match the message you are conveying verbally. Inconsistencies can lead to confusion and mistrust.
- Use Nonverbal Communication to Reinforce Verbal Messages: Gestures, facial expressions, and other nonverbal methods should be used to reinforce what you are saying verbally.
- Be Mindful of Personal Space: Every patient has different comfort levels with personal space. Be attentive to how close you stand or sit to a patient.
- Adapt to Each Patient’s Needs: Tailor your nonverbal communication style to suit the individual needs and preferences of each patient.
- Continuous Learning and Practice: Regularly update your skills and knowledge in nonverbal communication. Practice makes perfect, especially in an area as dynamic as nonverbal communication for nurses.
By following these tips, nurses can enhance their nonverbal communication skills, leading to better patient interactions, increased patient comfort, and overall improved patient care.
Importance of Verbal and Non-Verbal Communication in Nursing
The world of nursing is profoundly impacted by both verbal and non-verbal communication. Each type plays a distinct and crucial role in patient care, and understanding their importance is key to effective nursing. This comprehensive guide, optimized for “Nonverbal Communication for Nurses,” is presented in a table format to highlight the unique contributions and significance of both verbal and non-verbal communication in the nursing profession.
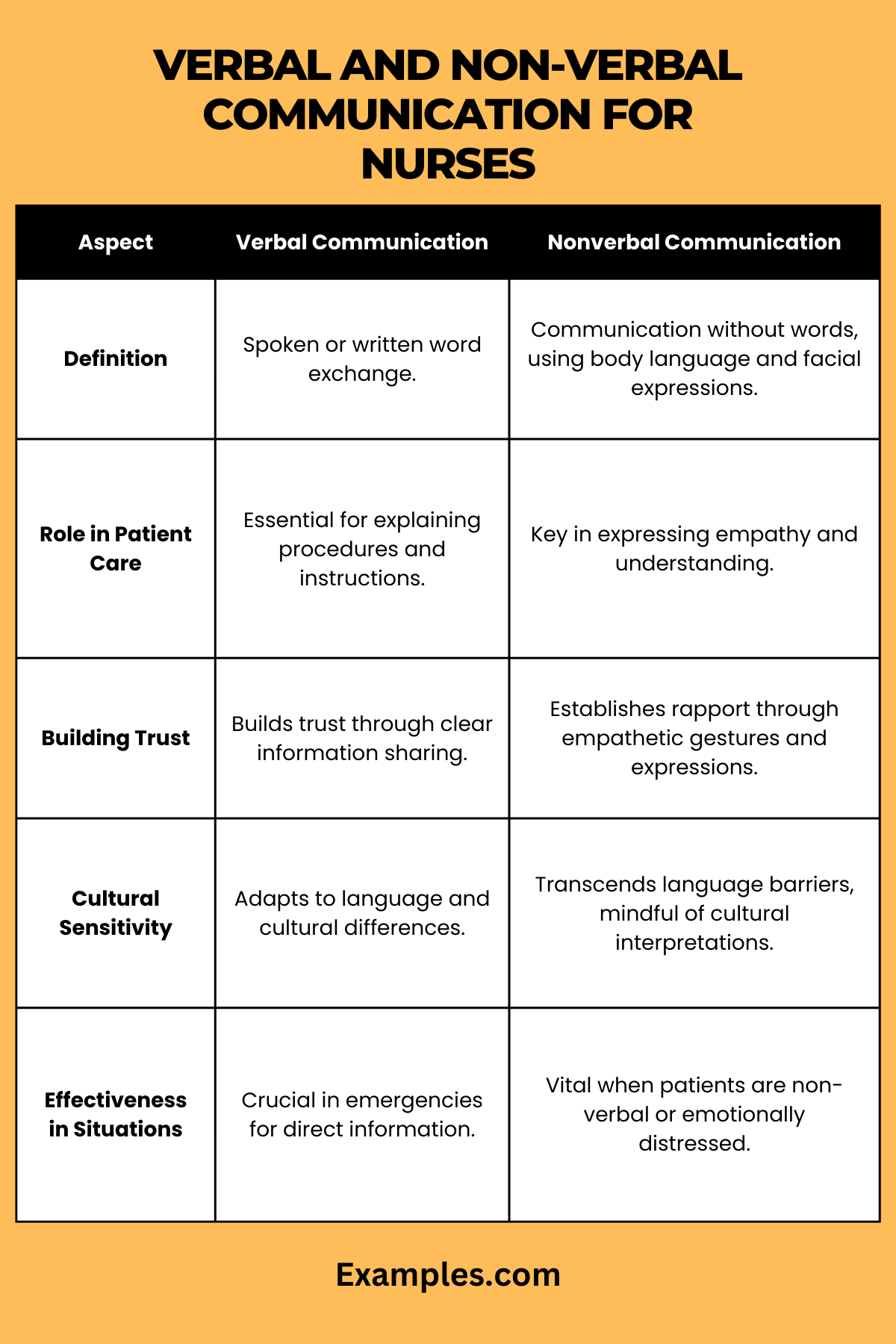
| Aspect | Verbal Communication | Non-Verbal Communication |
|---|---|---|
| Definition | Verbal communication in nursing involves the use of spoken or written words to convey information, emotions, and instructions to patients. It includes explaining medical procedures, patient education, and the exchange of information with colleagues. | Non-verbal communication in nursing encompasses all forms of communication that do not involve words. This includes facial expressions, body language, gestures, touch, and even the use of space. It’s about conveying empathy, care, and understanding without speaking. |
| Role in Patient Care | Verbal communication is crucial for clearly explaining health conditions, treatment plans, and answering patient queries. It’s essential for educating patients about their health and ensuring they understand their care. | Non-verbal communication plays a significant role in creating a therapeutic and comforting environment. It helps in building rapport, demonstrating empathy, and providing emotional support to patients, especially when they are anxious or fearful. |
| Building Trust and Rapport | Effective verbal communication helps in building trust between the nurse and patient. When patients understand their health situations and care plans clearly, it fosters trust and cooperation. | Non-verbal cues like a reassuring smile, eye contact, and a calm demeanor are powerful in building rapport. They help in making patients feel seen, heard, and cared for, which is essential in establishing a trusting relationship. |
| Cultural Sensitivity | Verbal communication must be adapted to respect and accommodate cultural differences in language, dialects, and health beliefs. It’s important for nurses to be aware of and sensitive to these differences to avoid misunderstandings. | Non-verbal communication can sometimes transcend cultural and language barriers. However, nurses must be aware of cultural differences in interpreting non-verbal cues, as gestures and expressions can have different meanings in different cultures. |
| Effectiveness in Different Situations | In emergencies or when dealing with critical information, verbal communication is key for its clarity and directness. It’s essential for quickly conveying important information and instructions. | In situations where patients are non-verbal, in pain, or experiencing emotional distress, non-verbal communication becomes especially important. It allows nurses to convey care and concern effectively when words may be insufficient. |
How do you Communicate Nonverbally with a Patient?
Communicating nonverbally with patients is an essential skill in nursing, providing a silent yet powerful means of connection and understanding. This method of communication, integral to nonverbal communication in healthcare, involves a keen awareness of one’s own gestures, facial expressions, and posture. Here are several key approaches:
- Facial Expressions: Utilize expressions to convey empathy and understanding, an essential aspect of nonverbal communication for nurses.
- Body Language: Adopt open body language, crucial in nonverbal communication at the workplace, particularly in healthcare settings.
- Eye Contact: Maintain eye contact to show attentiveness, a fundamental component of nonverbal communication skills.
- Gestures: Use clear gestures, especially when explaining medical procedures, demonstrating effective nonverbal communication for nurses.
- Touch: Apply appropriate and consensual touch, a key element in nonverbal communication for pain assessment and comfort.
- Proximity: Be conscious of physical proximity, respecting personal space while offering supportive presence.
- Listening Cues: Display active listening through nods and gestures, encouraging patient communication.
- Silence: Employ silence as a tool for giving patients time to process information, a subtle yet powerful aspect of nonverbal communication in healthcare.
Non Verbal Communication Nursing Strategies
Nonverbal communication is a cornerstone in nursing, enhancing patient care and trust. Here are strategies to refine nonverbal communication skills, essential in nonverbal communication for nurses:
- Self-Awareness: Be aware of personal nonverbal cues, an important aspect of nonverbal communication skills in nursing.
- Observation Skills: Develop skills to interpret patient nonverbal cues, key in nonverbal communication for pain and discomfort assessment.
- Cultural Competence: Understand cultural variations in nonverbal communication, vital for nonverbal communication in different cultures within healthcare.
- Consistency: Align nonverbal cues with verbal communication, ensuring clarity and trust, a crucial part of nonverbal communication for nurses.
- Training and Education: Engage in ongoing learning about nonverbal communication methods, enhancing skills in nonverbal communication in healthcare.
- Feedback and Reflection: Seek and reflect on feedback about nonverbal communication styles, an important practice for nonverbal communication skills development.
- Role-Playing: Practice nonverbal communication in various scenarios, crucial for refining nonverbal communication for nurses.
Implementing these strategies helps nurses to effectively use nonverbal communication, improving patient interactions and the overall quality of nursing care.
In conclusion, mastering nonverbal communication is vital for nurses, enhancing patient care and fostering trust. This guide has provided comprehensive examples and practical tips on nonverbal cues and strategies, emphasizing their significance in healthcare. By integrating these insights, nurses can improve their interactions, ensuring compassionate and effective patient care.