10 Therapeutic Communication with Suicidal Patient Examples
Therapeutic communication is a cornerstone in supporting suicidal patients, offering a lifeline through empathetic and understanding dialogue. This complete guide delves into real-world examples and provides essential tips, highlighting how therapeutic strategies can significantly impact patient care. From active listening to empathetic responses, discover the transformative power of effective communication in the delicate context of mental health support.
What is Therapeutic Communication with Suicidal Patient?
Therapeutic communication with suicidal patients involves specialized techniques used by healthcare professionals to engage with individuals experiencing suicidal thoughts. It focuses on establishing a safe, non-judgmental environment that fosters trust and open dialogue. This approach utilizes empathy, active listening, and supportive responses to understand the patient’s feelings and perspectives, ultimately aiding in their mental health journey.
What is the Best Example of Therapeutic Communication with Suicidal Patient?

One of the best examples of therapeutic communication with a suicidal patient is an empathetic and patient-centered conversation where the healthcare provider actively listens and responds with understanding and compassion. This might involve acknowledging the patient’s feelings, asking open-ended questions to encourage them to express themselves, and offering reassurances without judgment. Such communication aims to build a rapport, understand the patient’s emotional state, and provide support tailored to their specific needs.
15 Therapeutic Communication with Suicidal Patient Examples
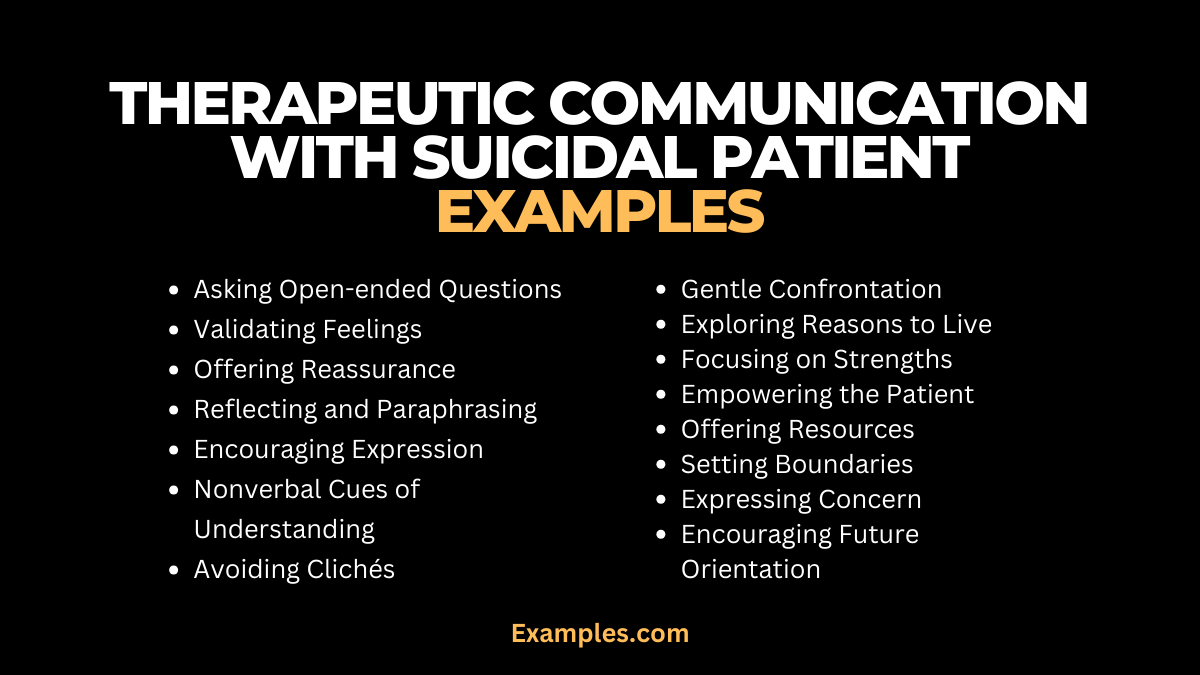
Exploring therapeutic communication with suicidal patients is crucial for effective mental health care. This guide presents 15 distinct examples, each illustrating key communication skills such as empathy, active listening, and nonjudgmental support. These examples demonstrate how to navigate sensitive conversations, offering hope and understanding in critical moments. Each example provides insights into crafting meaningful dialogues that can make a significant difference in a patient’s life.
- Asking open-ended questions: “Can you tell me more about what you’re feeling right now?” This approach encourages the patient to express their emotions and thoughts, facilitating a deeper understanding of their mental state.
- Validating feelings: “It sounds like you’re going through a really tough time.” This conveys empathy and acknowledges the patient’s struggles without judgment.
- Offering reassurance: “I’m here for you, and we’ll get through this together.” This statement provides comfort and a sense of partnership in facing their challenges.
- Reflecting and paraphrasing: “It seems like you feel hopeless because of your current situation.” Reflective statements show that the healthcare provider is actively listening and understanding the patient’s perspective.
- Encouraging expression: “It’s okay to share your feelings here. I want to understand your pain.” This invitation creates a safe space for the patient to communicate openly.
- Nonverbal cues of understanding: Nodding and maintaining eye contact. These nonverbal signals demonstrate attentiveness and concern.
- Avoiding clichés: “Every situation is unique, including yours.” Steering clear of generic responses respects the individuality of the patient’s experience.

- Exploring reasons to live: “What are some things that have been important to you in your life?” This question helps to identify positive aspects that might foster hope.
- Gentle confrontation: “You mentioned feeling useless, but I see someone with a lot of strength.” This technique challenges negative self-perceptions in a supportive way.
- Focusing on strengths: “You’ve shown a lot of courage by talking about these feelings.” Highlighting the patient’s strengths can boost their self-esteem and resilience.
- Empowering the patient: “What do you think would help you feel better?” This encourages the patient to take an active role in their recovery process.
- Offering resources: “There are people who specialize in helping with exactly what you’re going through.” Providing information about additional support options shows proactive care.

- Setting boundaries: “Let’s discuss what’s troubling you, but also how we can keep you safe.” This statement balances understanding with the need for safety.
- Expressing concern: “I’m worried about you, and I want to help.” Directly stating concern shows the patient they are valued and not alone.
- Encouraging future orientation: “Let’s talk about what we can do today to help you feel a bit better.” This shifts the focus towards positive actions and future improvements.
Therapeutic Communication with Suicidal Patient Examples in Nursing
Nurses play a crucial role in therapeutic communication with suicidal patients, employing compassion, empathy, and specialized communication skills. This segment focuses on 10 distinct examples of nurse-patient interactions, showcasing effective communication strategies tailored for mental health care. These examples highlight the importance of verbal and nonverbal communication, patient-centered dialogue, and the use of therapeutic techniques to build trust and provide emotional support in critical situations.
- Using silence effectively: “…” Allowing moments of silence can give the patient space to process their thoughts and feelings.
- Expressing empathy through touch: A gentle hand on the shoulder. This nonverbal gesture can convey warmth and understanding without words.
- Normalizing their experience: “Many people feel overwhelmed in situations like yours.” This helps the patient understand that their feelings are not uncommon.
- Clarifying statements: “Could you help me understand what you mean by…?” Asking for clarification ensures accurate understanding of the patient’s feelings.
- Offering hope in a realistic way: “We may not have all the answers, but we’ll find the best way forward together.” This provides encouragement while acknowledging the complexity of their situation.
- Acknowledging their distress: “It’s clear that you’re in a lot of pain right now.” Recognizing and validating their distress shows empathy.
- Encouraging participation in care: “What are some ways we can make you feel more comfortable here?” Involving the patient in their care plan fosters a sense of control and collaboration.
- Using metaphors to connect: “It sounds like you’re in a dark tunnel. Let’s find some light together.” Metaphors can help articulate complex emotions and create a shared understanding.
- Offering consistent reassurance: “I’m here for you, and I’ll check in on you regularly.” Consistent support helps build a trusting relationship.
- Encouraging small steps: “What’s one thing we can do today that might make a small difference for you?” This approach focuses on achievable goals, fostering a sense of progress.
What is Therapeutic Communication with Suicidal Patient in Healthcare?
-
Definition and Importance:
Therapeutic communication in healthcare, especially with suicidal patients, involves specialized interactions aimed at understanding and supporting individuals at risk. This type of communication is crucial in assessing risk factors, building rapport, and providing emotional support.
-
Creating a Safe Environment:
Healthcare professionals strive to create a non-threatening environment. Techniques such as open body language and a calm tone, pivotal in assertive communication, encourage patients to share their thoughts without fear of judgment.
-
Active Listening:
Active listening, a core aspect of effective communication, is essential. It involves paying full attention, understanding the patient’s verbal and nonverbal cues, and responding appropriately to convey understanding.
-
Empathy and Validation:
Showing empathy and validating a patient’s feelings are key. This approach helps in building trust, a critical aspect in managing the emotional turmoil experienced by suicidal patients.
-
Assessing and Responding to Risk:
An accurate assessment of suicide risk is vital. Healthcare professionals must employ assertive communication to ask direct yet sensitive questions to gauge the level of risk.
How does Therapeutic Communication Help Suicidal Patients?
- Establishing a Safe Environment: Creating a non-judgmental space where patients feel comfortable sharing their feelings, fostering trust and openness. Assertive communication aids in setting clear boundaries and expectations.
- Active Listening: Demonstrating genuine interest and concern through attentive listening. This helps the patient feel valued and understood.
- Validating Emotions: Acknowledging and validating the patient’s emotions, which helps in building rapport and conveying empathy.
- Empathy and Compassion: Showing empathy and compassion, which are central to therapeutic communication, makes the patient feel seen and heard.
- Risk Assessment: Using assertive communication to directly and sensitively assess the risk of self-harm or suicide, essential for ensuring patient safety.
- Crisis Intervention: Effectively intervening in crisis situations by utilizing therapeutic communication skills to de-escalate emotions and provide immediate support.
- Developing Coping Strategies: Assisting patients in identifying and developing healthy coping mechanisms to manage their distress.
- Encouraging Future Orientation: Focusing on future goals and positive outcomes, helping patients see beyond their current state of mind.
Therapeutic Communication with Suicidal Patients offers invaluable insights and practical examples for healthcare professionals. It emphasizes the importance of empathy, active listening, and assertive communication in forming a supportive connection with patients. These strategies are crucial for effectively navigating sensitive conversations, providing hope, and fostering a therapeutic environment essential for the well-being and recovery of those struggling with suicidal thoughts.