Preparing for the MCAT requires a comprehensive understanding of the circulatory system, a central element of the Organ Systems foundation. Mastery of cardiovascular physiology, including heart functions, blood flow, and vessel dynamics, provides essential insights into systemic health and is crucial for achieving a high MCAT score.
Learning Objective
In studying the "Circulatory System" for the MCAT, you should aim to understand the structure and function of the heart, blood vessels, and blood components. Learn how blood circulates through systemic and pulmonary circuits, and how oxygen, nutrients, and hormones are transported. Evaluate the physiological mechanisms regulating blood pressure, blood flow, and heart rate. Additionally, explore the pathophysiological aspects of cardiovascular diseases such as hypertension, atherosclerosis, and heart failure. Apply this knowledge to solve complex clinical scenarios, interpret diagnostic data, and tackle MCAT practice questions, focusing on how the circulatory system maintains homeostasis and responds to various stressors.
Understanding the Circulatory System Components and Function
The circulatory system consists of the heart, blood vessels, and blood, working together to transport oxygen, nutrients, hormones, and waste products throughout the body. The heart pumps blood through a network of arteries, veins, and capillaries. Oxygen-rich blood is carried from the lungs to body tissues via arteries, while veins return oxygen-depleted blood to the heart. Capillaries facilitate the exchange of gases, nutrients, and waste between blood and tissues. The circulatory system plays a vital role in maintaining homeostasis, regulating body temperature, and ensuring the proper functioning of organs by delivering essential substances and removing metabolic byproducts.
Key components and functions include:
Heart: Acts as a pump to circulate blood throughout the body.
The right side pumps deoxygenated blood to the lungs.
The left side pumps oxygenated blood to the body.
Blood vessels: Include arteries, veins, and capillaries.
Arteries: Carry oxygen-rich blood away from the heart.
Veins: Return oxygen-depleted blood back to the heart.
Capillaries: Small vessels where the exchange of gases, nutrients, and waste occurs between blood and tissues.
Blood: Transports oxygen, nutrients, hormones, and waste products.
Red blood cells carry oxygen.
White blood cells help fight infections.
Plasma transports nutrients, hormones, and waste.
Functions:
Delivers oxygen and nutrients to cells.
Removes carbon dioxide and other waste products.
Helps regulate body temperature.
Transports hormones that regulate body functions.
Maintains blood pressure and fluid balance.
Structure of the Circulatory System
The circulatory system is broadly composed of the heart, blood vessels, and blood.
Heart:
The heart is a muscular organ located in the thoracic cavity, slightly left of the center. It functions as a pump to circulate blood throughout the body.
It has four chambers: two upper chambers called atria and two lower chambers called ventricles. The right side of the heart pumps blood to the lungs (pulmonary circulation), and the left side pumps it to the rest of the body (systemic circulation).
Blood Vessels:
Blood vessels are tubular structures (arteries, veins, capillaries) that transport blood throughout the body, delivering oxygen and nutrients.
Arteries: Thick-walled vessels that carry oxygen-rich blood away from the heart (except for the pulmonary arteries, which carry oxygen-poor blood to the lungs).
Veins: Thinner-walled vessels that carry oxygen-poor blood back to the heart (except for the pulmonary veins, which carry oxygen-rich blood from the lungs).
Capillaries: The smallest blood vessels where the exchange of water, oxygen, carbon dioxide, and many other nutrients and waste substances occurs between blood and tissues.
Blood:
Composed of red blood cells (carry oxygen), white blood cells (immune defense), platelets (blood clotting), and plasma (liquid component that carries nutrients, hormones, and proteins).
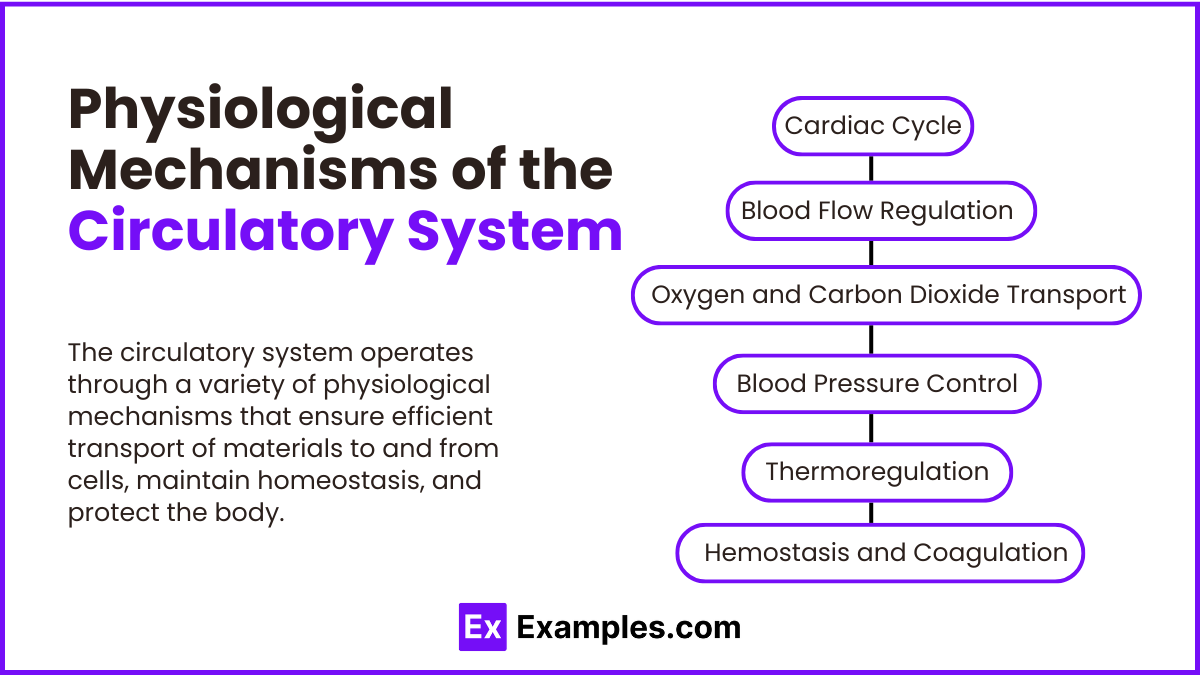
Physiological Mechanisms of the Circulatory System
The circulatory system operates through a variety of physiological mechanisms that ensure efficient transport of materials to and from cells, maintain homeostasis, and protect the body. Here are some key mechanisms and processes involved:
1. Cardiac Cycle
The cardiac cycle includes all the events that occur from one heartbeat to the next. It consists of two main phases: diastole (relaxation phase, when the heart chambers fill with blood) and systole (contraction phase, when the heart ejects blood).
During diastole, the atria and ventricles are relaxed and the ventricles fill with blood. This is followed by the atrial contraction which tops off the ventricular filling.
Systole begins with ventricular contraction, pushing blood into the pulmonary artery (from the right ventricle) and the aorta (from the left ventricle), while the atria relax and start to refill.
2. Blood Flow Regulation
Vascular Resistance: Blood flow is regulated by changes in the diameter of the blood vessels. For instance, vasoconstriction (narrowing of blood vessels) increases resistance and decreases blood flow, while vasodilation (widening of blood vessels) decreases resistance and increases flow.
Autoregulation: Local conditions within tissues can cause automatic adjustments in blood vessel diameter to meet varying demands for oxygen and nutrients (e.g., during exercise or in response to temperature changes).
3. Oxygen and Carbon Dioxide Transport
Oxygen: Most oxygen is bound to hemoglobin in red blood cells. Hemoglobin binds oxygen in the lungs, where oxygen concentration is high, and releases it in tissues, where oxygen concentration is low.
Carbon Dioxide: CO2, a waste product of metabolism, is transported back to the lungs in three main ways: dissolved in plasma, bound to hemoglobin, or as bicarbonate ions. The majority is transported as bicarbonate, formed in the reaction of CO2 with water, catalyzed by the enzyme carbonic anhydrase in red blood cells.
4. Blood Pressure Control
Blood pressure is regulated by hormonal and neural mechanisms:
Baroreceptor Reflex: Specialized sensors in the arteries (baroreceptors) detect changes in blood pressure and send signals to the brain, which adjusts heart rate and vessel diameter to stabilize pressure.
Renin-Angiotensin-Aldosterone System (RAAS): This hormonal system is activated when blood pressure is perceived to be low, leading to the secretion of aldosterone, which increases sodium and water reabsorption by the kidneys to increase blood volume and pressure.
5. Thermoregulation
The circulatory system plays a critical role in maintaining body temperature by controlling blood flow to the skin. During high temperatures, blood vessels in the skin dilate, allowing more blood to flow near the surface and heat to dissipate. In cold conditions, these vessels constrict to retain heat.
6. Hemostasis and Coagulation
When a vessel is damaged, the circulatory system initiates a cascade of events to stop bleeding:
Vascular Spasm: Immediate constriction of the blood vessel.
Platelet Plug Formation: Platelets adhere to the damaged area and aggregate to form a temporary plug.
Coagulation: A complex series of steps involving clotting factors leads to the transformation of fibrinogen into fibrin, which stabilizes the platelet plug into a durable clot.
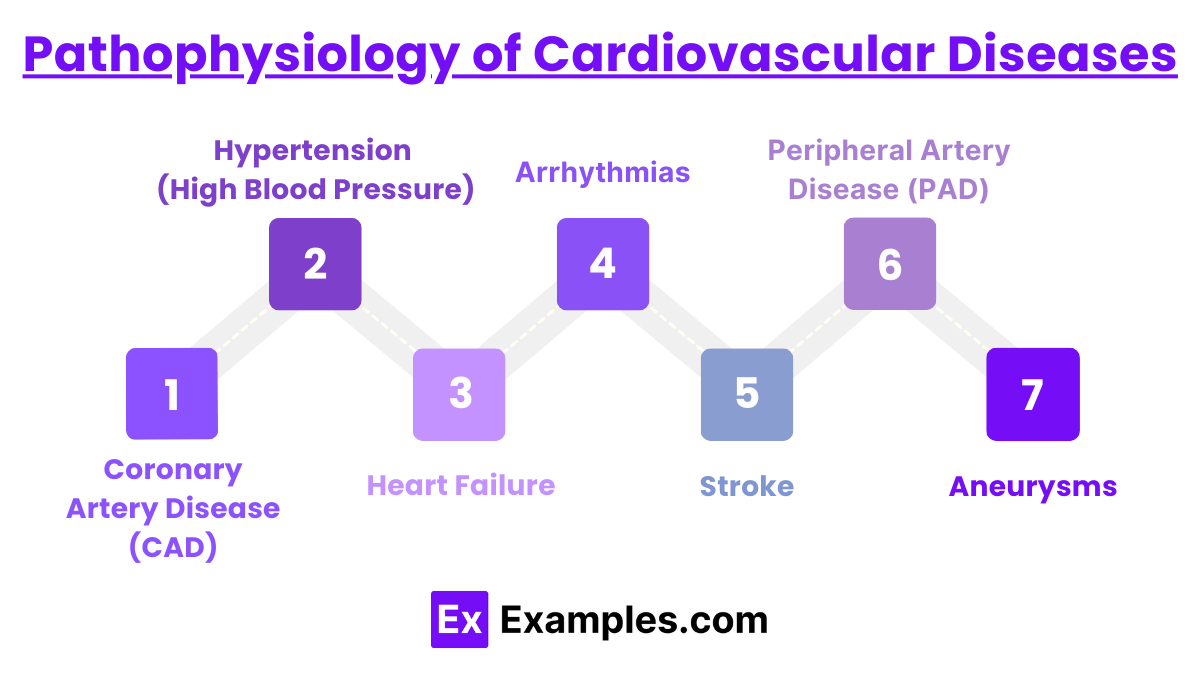
Pathophysiology of Cardiovascular Diseases
The pathophysiology of cardiovascular diseases (CVD) involves various disorders that affect the heart and blood vessels, each with distinct mechanisms and consequences. Here's an overview of the pathophysiological aspects of common cardiovascular conditions:
1. Coronary Artery Disease (CAD)
Cause: Accumulation of atherosclerotic plaques in the coronary arteries, which supply blood to the heart muscle.
Pathophysiology: Plaque buildup narrows the arteries, reducing blood flow to the heart. This can lead to myocardial ischemia (reduced oxygen to the heart muscle), causing angina (chest pain) and potentially myocardial infarction (heart attack) if a plaque ruptures and forms a clot.
2. Hypertension (High Blood Pressure)
Cause: Often multifactorial, including genetic predisposition, lifestyle factors, and other diseases (e.g., kidney disease).
Pathophysiology: Increased blood pressure can cause endothelial damage and is a major risk factor for stroke, heart attack, and aneurysms. It also puts a strain on the heart, leading to hypertensive heart disease.
3. Heart Failure
Cause: Inability of the heart to pump sufficiently to meet the body's needs. Can result from chronic high blood pressure, heart attack, valve disorders, or cardiomyopathy.
Pathophysiology: Heart failure leads to systemic and pulmonary congestion due to fluid backup, as the heart cannot keep up with the return flow of blood. This results in symptoms like shortness of breath, edema, and fatigue.
4. Arrhythmias
Cause: Abnormal electrical impulses in the heart, which can stem from heart damage, electrolyte imbalances, or changes in heart tissue.
Pathophysiology: Arrhythmias (such as atrial fibrillation, ventricular tachycardia) disrupt the normal rhythm of the heart, which can impair its efficiency and lead to reduced cardiac output and even sudden cardiac death.
5. Stroke
Types: Ischemic (due to blocked blood vessels) and hemorrhagic (due to bleeding).
Pathophysiology:
Ischemic Stroke: Most common type, occurring when a blood clot blocks or narrows an artery leading to the brain, causing reduced blood flow.
Hemorrhagic Stroke: Occurs when a blood vessel in the brain bursts, leading to localized bleeding in the surrounding tissues and damage to brain cells.
6. Peripheral Artery Disease (PAD)
Cause: Atherosclerosis in the peripheral arteries, particularly those supplying the legs.
Pathophysiology: Similar to CAD, PAD reduces blood flow to the extremities, causing symptoms like pain, difficulty walking, and, in severe cases, gangrene.
7. Aneurysms
Cause: Weakening of an artery wall, which can expand and rupture.
Pathophysiology: Pressure from blood flow can cause the weakened area to bulge outwards, potentially leading to a life-threatening rupture if not treated.
Examples
Example 1: Cardiac Cycle
Scenario: Understanding the phases of the cardiac cycle.
Process: The cardiac cycle includes the diastole phase where the heart relaxes and fills with blood, followed by the systole phase where the heart contracts and pumps blood out. The coordination of these phases ensures efficient blood circulation through the pulmonary and systemic circuits.
Example 2: Regulation of Blood Pressure
Scenario: Acute response to a drop in blood pressure.
Process: When blood pressure drops, sensors in the carotid arteries and aorta detect the change and send signals to the brain. The brain then increases heart rate and constricts blood vessels via the sympathetic nervous system, raising the blood pressure to normal levels.
Example 3: Arterial Plaque and Atherosclerosis
Scenario: Development of atherosclerosis in coronary arteries.
Process: Atherosclerosis begins with the damage to the endothelium of arteries, followed by the accumulation of lipids and formation of a plaque. This plaque can narrow the artery and reduce blood flow to the heart muscle, potentially leading to ischemic heart disease.
Example 4: Gas Exchange in Capillaries
Scenario: Oxygen and carbon dioxide exchange during systemic circulation.
Process: In systemic capillaries, oxygen diffuses out of the blood into the tissues while carbon dioxide diffuses into the blood from the tissues. This gas exchange is critical for cellular respiration and the removal of metabolic waste.
Example 5: Heart Failure
Scenario: Compensatory mechanisms in early heart failure.
Process: In response to reduced cardiac output in heart failure, the body activates neurohormonal systems like the renin-angiotensin-aldosterone system (RAAS) to increase blood volume and pressure. While initially helpful, these mechanisms can worsen heart failure by increasing the workload on the heart.
Practice Questions
Question 1: Cardiac Output
What increases cardiac output in response to increased physical activity?
A) Decrease in heart rate
B) Increase in heart rate and stroke volume
C) Increase in systemic vascular resistance
D) Decrease in stroke volume
Correct Answer: B) Increase in heart rate and stroke volume
Explanation:
Cardiac output, which is the volume of blood the heart pumps per minute, increases in response to physical activity primarily through an increase in heart rate and stroke volume. Increased heart rate speeds up the pumping action, while increased stroke volume allows more blood to be ejected with each heartbeat, meeting the body's elevated demand for oxygen and nutrients during activity.
Question 2: Blood Pressure Regulation
Which hormone plays a critical role in increasing blood pressure by promoting sodium retention in the kidneys
A) Insulin
B) Aldosterone
C) Glucagon
D) Epinephrine
Correct Answer: B) Aldosterone
Explanation:
Aldosterone, a hormone secreted by the adrenal cortex, helps regulate blood pressure by increasing sodium retention in the kidneys, which leads to water retention and increased blood volume, ultimately raising blood pressure. This mechanism is part of the renin-angiotensin-aldosterone system (RAAS), which is activated in response to decreased blood pressure or blood flow.
Question 3: Pathophysiology of Atherosclerosis
What is the initial event that leads to the development of atherosclerosis?
A) Plaque rupture
B) Endothelial injury
C) Smooth muscle proliferation
D) Formation of a fibrous cap
Correct Answer: B) Endothelial injury
Explanation:
The development of atherosclerosis begins with injury to the endothelium, the inner lining of the artery. This damage can be caused by factors such as high blood pressure, smoking, or high cholesterol. The injury triggers an inflammatory response that leads to the accumulation of lipids and other substances, eventually forming plaques that narrow and stiffen the arteries, potentially leading to more serious cardiovascular complications.