Preparing for the MCAT requires a thorough understanding of the gastrointestinal system, a central element of the Organ Systems foundation. Mastery of digestive processes, nutrient absorption, and the regulation of these functions is crucial. This knowledge provides insights into how the body processes food and maintains nutrient homeostasis, essential for achieving a high MCAT score.
Learning Objective
In studying the "Gastrointestinal System" for the MCAT, you should aim to understand the anatomy and physiology of the digestive tract, from ingestion to excretion. Learn the roles and functions of each organ in the digestion and absorption of nutrients, and the enzymatic breakdown of food. Explore how the GI system regulates these processes via neural and hormonal signals. Additionally, examine common gastrointestinal disorders such as GERD, peptic ulcers, and inflammatory bowel disease. Apply this knowledge to interpret diagnostic tests and treatments, and solve MCAT practice questions that test your ability to integrate and apply comprehensive knowledge of gastrointestinal physiology and pathology.
Anatomy of Gastrointestinal System
The gastrointestinal (GI) system, also known as the digestive system, is responsible for the breakdown and absorption of food, converting it into energy and nutrients that the body can use, and eliminating waste. It consists of various organs that work together to digest food, absorb nutrients, and expel waste. Here’s a detailed overview of its anatomy and physiology:
Mouth:
Begins the digestive process through mechanical (chewing) and chemical (enzymes in saliva) means.
Saliva contains amylase that starts the breakdown of carbohydrates.
Esophagus:
A muscular tube that connects the mouth to the stomach.
Swallowed food is pushed down by peristaltic movements to the stomach.
Stomach:
A hollow organ that secretes acid and enzymes to further break down food.
The stomach churns food to mix it with gastric juices, producing a semi-liquid substance called chyme.
Small Intestine:
Comprises three parts: the duodenum, jejunum, and ileum.
The duodenum receives bile from the liver and gallbladder, and pancreatic juices from the pancreas, aiding in fat and protein digestion.
The jejunum and ileum mainly absorb nutrients and water from digested food.
Large Intestine (Colon):
Absorbs water and salts from the material that has not been digested as food, and is thus responsible for forming solid waste (feces).
Ends in the rectum and anus where feces are expelled.
Liver:
Produces bile that emulsifies fats to aid in their digestion.
Has multiple roles including detoxification, protein synthesis, and the metabolism of fats and carbohydrates.
Gallbladder:
Stores and concentrates bile, releasing it into the small intestine to aid in digestion.
Pancreas:
Produces digestive enzymes and bicarbonate, which are released into the small intestine to aid in digestion.
Also has endocrine functions, secreting insulin and glucagon into the bloodstream to regulate blood sugar levels.
Regulation of Digestive Functions
The regulation of digestive functions is managed through an intricate system of neural, hormonal, and local mechanisms that work together to ensure efficient digestion, absorption, and excretion. Here are the key points summarized:
1. Neural Regulation
Enteric Nervous System (ENS): Controls local gut activities independently but coordinates with the central nervous system.
Autonomic Nervous System (ANS):
Parasympathetic Nervous System: Enhances digestion by increasing secretions and motility.
Sympathetic Nervous System: Inhibits digestion during stress or physical activity.
2. Hormonal Regulation
Gastrin: Stimulates stomach acid secretion and motility.
Secretin: Promotes bicarbonate secretion from the pancreas to neutralize stomach acid in the small intestine.
Cholecystokinin (CCK): Triggers bile release from the gallbladder and enzyme secretion from the pancreas; slows gastric emptying.
Motilin: Regulates intestinal contractions during fasting.
Ghrelin: Signals hunger and stimulates stomach motility and acid production.
3. Local Factors
Chemoreceptors and Mechanoreceptors: Detect changes in the GI tract's environment, adjusting motility and secretion.
pH and Osmolarity Changes: Influence enzyme activity and electrolyte movement.
4. Feedback Mechanisms
Negative Feedback: Controls the pace of digestion, such as slowing stomach emptying when the small intestine is full.
Positive Feedback: Enhances certain digestive processes, although less common.
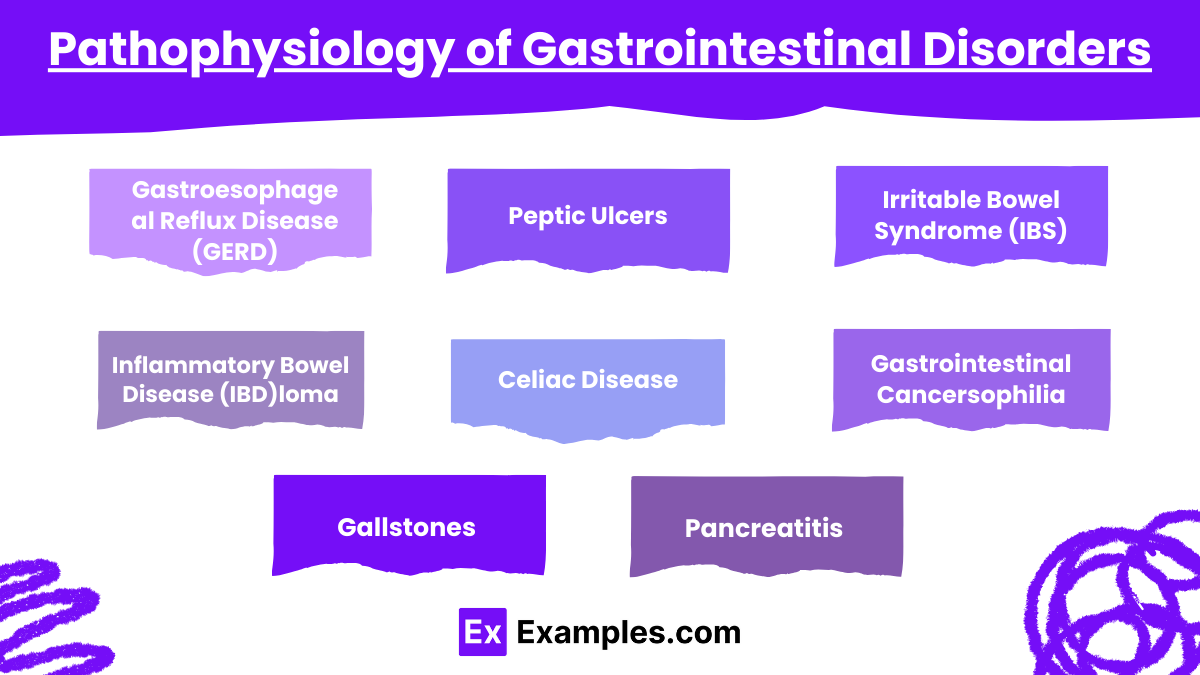
Pathophysiology of Gastrointestinal Disorders
The pathophysiology of gastrointestinal (GI) disorders encompasses a wide range of conditions that can affect any part of the digestive system, from the esophagus to the colon. These disorders can impair the body's ability to digest food, absorb nutrients, and expel waste. Here’s a detailed overview of common gastrointestinal disorders and their underlying pathophysiological mechanisms:
1. Gastroesophageal Reflux Disease (GERD)
Pathophysiology: Caused by dysfunction of the lower esophageal sphincter allowing stomach acid to enter the esophagus.
Implications: Results in heartburn, potential esophageal damage.
2. Peptic Ulcers
Pathophysiology: Ulcers form due to an imbalance between digestive acids and mucosal defense, often exacerbated by Helicobacter pylori or NSAIDs.
Implications: Can cause bleeding, stomach perforation.
3. Irritable Bowel Syndrome (IBS)
Pathophysiology: Functional disorder with symptoms like pain, bloating, and altered bowel habits without clear damage to the tissues.
Implications: Managed with diet and lifestyle modifications.
4. Inflammatory Bowel Disease (IBD)
Pathophysiology: Includes Crohn’s disease and ulcerative colitis with chronic intestinal inflammation due to immune dysregulation.
Implications: Persistent symptoms, risk of intestinal complications, and increased cancer risk.
5. Celiac Disease
Pathophysiology: Autoimmune response to gluten in genetically susceptible people causing intestinal damage.
Implications: Leads to nutrient malabsorption and associated symptoms.
6. Gastrointestinal Cancers
Pathophysiology: Malignant growths in the GI tract; often develop from benign polyps.
Implications: Symptoms depend on tumor location and can include blockage and bleeding.
7. Gallstones
Pathophysiology: Cholesterol or bilirubin crystallizes in the gallbladder, forming stones.
Implications: Can cause pain and block bile ducts, leading to pancreatitis or cholecystitis.
8. Pancreatitis
Pathophysiology: Inflammation of the pancreas, usually due to gallstones or alcohol abuse.
Implications: Severe abdominal pain, digestion issues.
Examples
Example 1: Digestion and Absorption of Nutrients
Scenario: A meal containing carbohydrates, proteins, and fats.
Process: Carbohydrates begin to break down in the mouth by salivary amylase, proteins are denatured and digested by stomach acid and pepsin, and fats are emulsified by bile in the small intestine before being digested by pancreatic lipase. Nutrients are absorbed primarily in the small intestine through various transport mechanisms.
Example 2: Hormonal Regulation of Digestion
Scenario: Eating a protein-rich meal.
Process: Proteins in the stomach stimulate G cells to release gastrin, which promotes gastric acid secretion for further protein digestion. The presence of fats and proteins in the small intestine triggers the release of cholecystokinin (CCK), which stimulates the gallbladder to release bile and the pancreas to secrete digestive enzymes.
Example 3: Gastroesophageal Reflux Disease (GERD)
Scenario: A patient experiences heartburn and acid reflux.
Process: GERD occurs when the lower esophageal sphincter is weak or relaxes inappropriately, allowing stomach acid to flow back into the esophagus. This can cause symptoms like heartburn, chest pain, and potential damage to the esophageal lining.
Example 4: Inflammatory Bowel Disease (IBD)
Scenario: A patient with Crohn's disease.
Process: Crohn’s disease is characterized by inflammation that can occur anywhere in the GI tract but most commonly affects the end of the small intestine and beginning of the colon. Symptoms include abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition, resulting from inflammation that can spread into deeper layers of the bowel.
Example 5: Colon Cancer Screening
Scenario: Routine screening in a 50-year-old patient.
Process: Screening methods such as colonoscopy are recommended to detect early signs of colon cancer. During a colonoscopy, a long, flexible tube with a camera on the end is used to view the entire colon and rectum. Any polyps found can be removed, and suspicious areas biopsied to check for cancer cells.
Practice Questions
Question 1: Enzyme Function in Digestion
Which enzyme is responsible for the breakdown of fats into fatty acids and glycerol?
A) Amylase
B) Pepsin
C) Lipase
D) Trypsin
Correct Answer: C) Lipase
Explanation:
Lipase is the enzyme that specifically breaks down fats into fatty acids and glycerol. It is primarily produced by the pancreas and functions in the small intestine, where it acts on the emulsified fats to facilitate their absorption into the body. Amylase breaks down carbohydrates, while pepsin and trypsin are involved in protein digestion.
Question 2: Role of Bile
What is the primary function of bile in the digestive system?
A) To neutralize stomach acid as it enters the small intestine
B) To emulsify fats to increase their surface area for enzyme action
C) To increase the pH of the small intestine
D) To break down proteins into amino acids
Correct Answer: B) To emulsify fats to increase their surface area for enzyme action
Explanation:
Bile, produced by the liver and stored in the gallbladder, plays a crucial role in digestion by emulsifying fats. This process increases the surface area of fat droplets, making them more accessible to digestive enzymes like pancreatic lipase. Bile does not neutralize stomach acid nor does it directly affect pH or protein digestion.
Question 3: Gastrointestinal Hormones
Which hormone stimulates the pancreas to release bicarbonate-rich fluid into the small intestine?
A) Gastrin
B) Secretin
C) Cholecystokinin (CCK)
D) Ghrelin
Correct Answer: B) Secretin
Explanation:
Secretin is a hormone released by the duodenum in response to acidic chyme entering from the stomach. Its primary function is to stimulate the pancreas to release a bicarbonate-rich fluid, which neutralizes the acid in the chyme, protecting the intestinal lining and providing an optimal pH for enzymatic activity in the small intestine.