Preparing for the MCAT requires a solid understanding of the hematologic system, crucial for the Organ Systems foundation. Mastery of blood components, their functions, and hematopoiesis, along with disorders like anemia and leukemia, provides essential insights into how blood supports health and fights disease, critical for a high MCAT score.
Learning Objective
In studying the “Hematologic System” for the MCAT, you should aim to understand the components of blood, including red and white blood cells, platelets, and plasma, and their respective functions in transport, defense, and coagulation. Learn about the processes of hematopoiesis, erythropoiesis, and leukopoiesis, and how they are regulated by various hormones and growth factors. Explore common hematologic disorders like anemia, leukemia, and clotting dysfunctions. Additionally, examine how blood components interact with the immune system and other physiological systems, and apply this knowledge to diagnose and interpret clinical scenarios and laboratory results in MCAT practice passages.
Understanding the Hematologic System
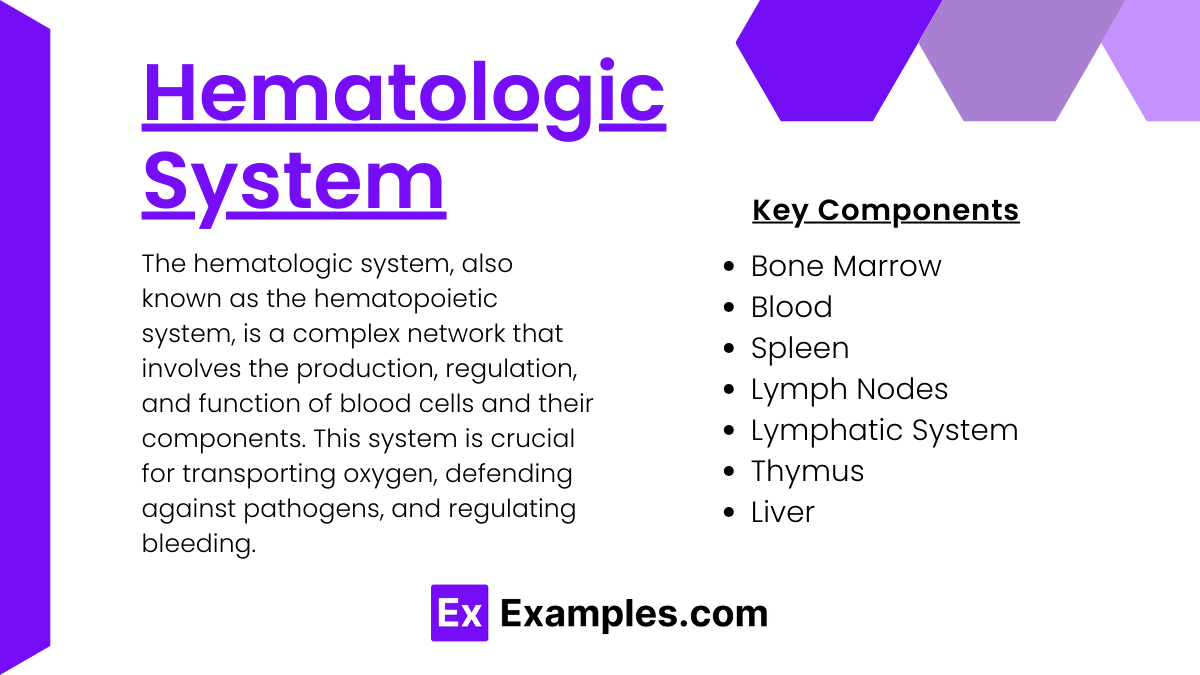
The hematologic system, also known as the hematopoietic system, is a complex network that involves the production, regulation, and function of blood cells and their components. This system is crucial for transporting oxygen, defending against pathogens, and regulating bleeding. Here’s a detailed overview of the components and functions of the hematologic system:
Key Components of the Hematologic System
- Bone Marrow
- Primary site for hematopoiesis, the process of blood cell production.
- Produces red blood cells, white blood cells, and platelets from hematopoietic stem cells.
- Blood
- Red Blood Cells (Erythrocytes): Carry oxygen from the lungs to the body’s tissues and bring carbon dioxide back to the lungs for exhalation.
- White Blood Cells (Leukocytes): Part of the immune system, responsible for fighting infections and other diseases.
- Platelets (Thrombocytes): Essential for clot formation to stop bleeding.
- Spleen
- Filters blood, removes old and damaged blood cells, and helps fight certain kinds of bacteria.
- Stores white blood cells and platelets.
- Lymph Nodes and Lymphatic System
- Part of the immune system, lymph nodes filter lymph fluid and store lymphocytes (a type of white blood cell).
- Helps in the removal of toxins and waste from the body.
- Thymus
- Site of T-cell maturation, a specific type of white blood cell important for immune response.
- Liver
- Produces clotting factors, clears toxins from blood, and metabolizes various components of blood.
- Stores extra iron from hemoglobin.
Functions of the Hematologic System
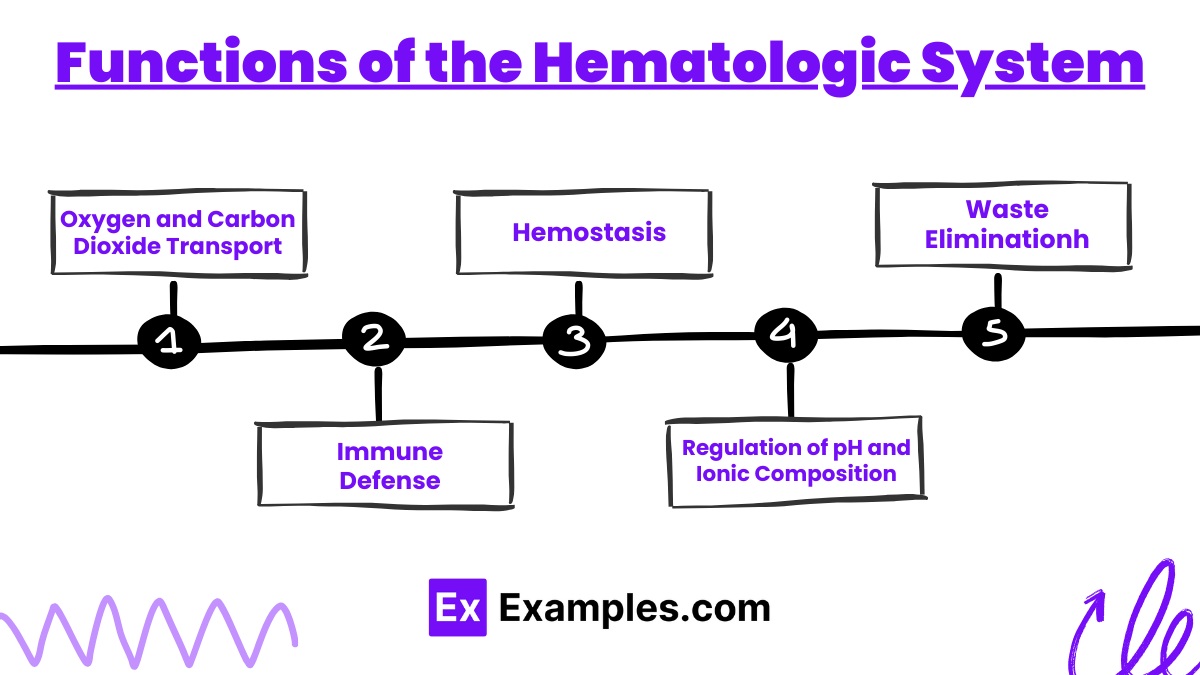
- Oxygen and Carbon Dioxide Transport
- Red blood cells contain hemoglobin, which binds to oxygen and carbon dioxide, facilitating their transport.
- Immune Defense
- White blood cells protect the body from infection and facilitate the inflammatory process to isolate and destroy pathogens.
- Different types of white blood cells (neutrophils, lymphocytes, monocytes, eosinophils, and basophils) play specific roles in defense and immunity.
- Hemostasis
- The process of blood clotting involves a cascade of events that lead to the formation of a clot, which seals damaged vessels to prevent blood loss.
- Platelets adhere to the site of vessel damage, form a plug, and help in the activation of clotting factors that stabilize the blood clot.
- Regulation of pH and Ionic Composition
- Blood acts as a buffer, maintaining the pH and ionic balance of the body’s fluids, which is crucial for normal cellular function.
- Waste Elimination
- Blood transports waste products from cellular metabolism (like urea and creatinine) to organs like the kidneys for excretion.
Physiological Processes and Regulation
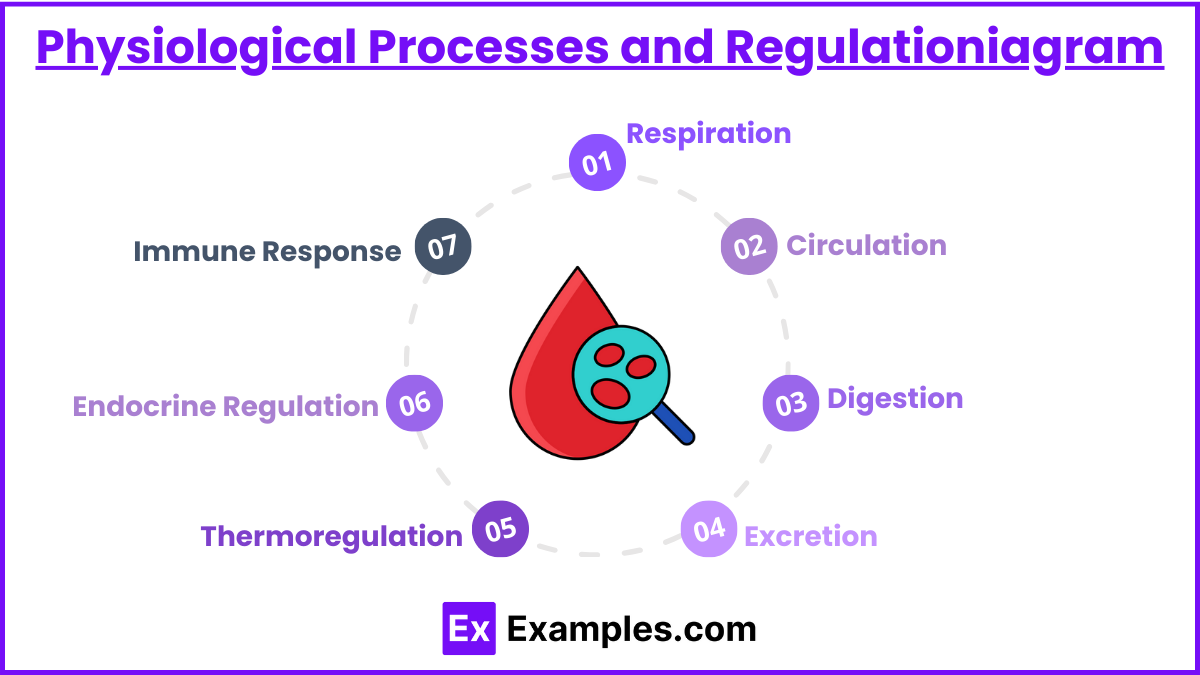
Physiological processes are the series of chemical reactions and activities that occur within the body to maintain life. These processes are tightly regulated through complex feedback mechanisms and systems to ensure homeostasis, or the stable condition of an organism and its internal environment. Here’s an overview of key physiological processes and their regulation:
1. Respiration
- Process: The act of inhaling oxygen and exhaling carbon dioxide, carried out by the respiratory system. This includes external respiration (gas exchange between air and blood in the lungs) and cellular respiration (use of oxygen for metabolism and energy production in cells).
- Regulation: Controlled primarily by the respiratory center in the brainstem, which adjusts the rate of breathing based on CO2 levels, pH, and oxygen in the blood, monitored through chemoreceptors in the body.
2. Circulation
- Process: The movement of blood throughout the body via the heart and blood vessels, delivering nutrients and oxygen, and removing waste products.
- Regulation: The cardiovascular system is regulated by neural and hormonal signals that control heart rate, blood pressure, and the distribution of blood to various tissues. Baroreceptors and chemoreceptors provide feedback to the central nervous system to adjust these variables.
3. Digestion
- Process: The breakdown of food into smaller components that can be absorbed by the body, involving both mechanical and chemical processes.
- Regulation: Digestive processes are regulated by the nervous system and hormones such as gastrin, cholecystokinin, and secretin, which control the release of digestive enzymes and bile, and the motility of the gastrointestinal tract.
4. Excretion
- Process: The removal of waste products from the body, primarily carried out by the kidneys (urine), lungs (CO2), and skin (sweat).
- Regulation: Kidney function is regulated by hormones such as antidiuretic hormone (ADH), aldosterone, and the renin-angiotensin system, which adjust blood flow, water, and electrolyte balance based on the body’s needs.
5. Thermoregulation
- Process: The maintenance of body temperature within a range that allows cells to function efficiently.
- Regulation: Regulated through mechanisms such as sweating, shivering, and changes in blood flow to the skin. The hypothalamus acts as the control center, responding to temperature receptors in the skin and changes in blood temperature.
6. Endocrine Regulation
- Process: The secretion of hormones by endocrine glands that control or affect various physiological processes.
- Regulation: Governed by feedback loops where the effects of hormones can promote or inhibit further hormone release. For example, high blood sugar levels stimulate the release of insulin, which helps lower glucose levels, reducing further insulin release.
7. Immune Response
- Process: The body’s defense mechanism against pathogens, involving both innate (non-specific) and adaptive (specific) responses.
- Regulation: Components of the immune system, like T cells and B cells, are regulated by cytokines and other immune mediators, which coordinate the body’s response to infections or inflammation.
Pathophysiology of Hematologic Disorders
Hematologic disorders encompass a wide range of conditions affecting the blood and its components, including red blood cells, white blood cells, platelets, and the clotting system. These disorders can have significant impacts on overall health, stemming from various pathophysiological processes. Here’s an overview of the pathophysiology behind some common hematologic disorders:
1. Anemia
- Cause: Anemia results from a deficiency in the number or quality of red blood cells (RBCs) or hemoglobin, which impairs oxygen delivery to tissues.
- Types and Pathophysiology:
- Iron Deficiency Anemia: Caused by a lack of iron, which is necessary for hemoglobin synthesis. Common in populations with poor diet or chronic bleeding.
- Megaloblastic Anemia: Due to a deficiency in vitamin B12 or folate, critical for DNA synthesis, leading to the production of abnormally large and dysfunctional red blood cells.
- Hemolytic Anemia: RBCs are destroyed faster than they are made, due to factors like autoimmune diseases, infections, or hereditary conditions (e.g., sickle cell disease).
2. Leukemia
- Cause: A type of cancer that starts in the bone marrow, leading to the overproduction of abnormal white blood cells (WBCs).
- Pathophysiology: These abnormal WBCs are not fully developed and are ineffective at fighting infections. They also crowd out normal blood cells, leading to increased susceptibility to bleeding, anemia, and infections.
3. Lymphoma
- Cause: Cancer of the lymphatic system, affecting lymphocytes, a type of white blood cell.
- Pathophysiology: Malignant lymphocytes accumulate in lymph nodes and other tissues, impairing immune function and sometimes spreading to other organs.
4. Myeloma
- Cause: Cancer involving plasma cells (mature B lymphocytes) that produce antibodies.
- Pathophysiology: Abnormal plasma cells multiply in the bone marrow, producing large amounts of a single type of antibody that is nonfunctional, leading to reduced immunity and interference with the production of normal blood cells.
5. Thrombocytopenia
- Cause: Low platelet count, which can result from a variety of conditions, including bone marrow disorders, autoimmune diseases, or certain medications.
- Pathophysiology: Insufficient platelets impair the blood clotting process, increasing the risk of excessive bleeding.
6. Hemophilia
- Cause: A genetic disorder leading to deficiency in one of the clotting factors (Factor VIII or IX).
- Pathophysiology: The deficiency in clotting factors prevents the normal clotting cascade, leading to prolonged bleeding even with minor injuries.
7. Polycythemia Vera
- Cause: A rare blood cancer in which the bone marrow makes too many red blood cells.
- Pathophysiology: Excessive RBCs increase blood viscosity, which can slow blood flow and increase the risk of clots.
Examples
Example 1: Erythropoiesis and Anemia
- Scenario: A patient with chronic kidney disease experiencing anemia.
- Process: Due to the kidneys’ reduced ability to produce erythropoietin in response to low oxygen levels in the blood, erythropoiesis in the bone marrow is decreased, leading to fewer red blood cells and resulting in anemia. This condition manifests as fatigue and pallor due to insufficient oxygen delivery to tissues.
Example 2: Hemostasis and Clotting Cascade
- Scenario: A cut on the finger initiates the clotting process.
- Process: Damage to blood vessels exposes collagen and tissue factor, triggering the clotting cascade. Platelets adhere to the damaged site and form a plug. Concurrently, the cascade activates thrombin, which converts fibrinogen to fibrin, solidifying the platelet plug into a stable clot that stops bleeding.
Example 3: Acute Myelogenous Leukemia (AML)
- Scenario: A patient presents with fatigue, bruising, and frequent infections.
- Process: AML involves the rapid growth of abnormal myeloid cells in the bone marrow, crowding out normal blood cells. This leads to a decrease in healthy white blood cells, red blood cells, and platelets, causing the symptoms observed in the patient.
Example 4: Immune Response by White Blood Cells
- Scenario: Response to a bacterial infection.
- Process: Neutrophils and macrophages are among the first responders to a bacterial invasion. Neutrophils engulf and destroy bacteria through phagocytosis, while macrophages present antigens from the bacteria to T cells, initiating a specific immune response and producing antibodies to target the bacteria.
Example 5: Thrombocytopenia and Bleeding
- Scenario: A patient with unusually severe and frequent nosebleeds.
- Process: Thrombocytopenia, a condition characterized by abnormally low platelet counts, impairs the blood clotting process. The deficiency in platelets prevents the formation of an effective platelet plug at the site of blood vessel injury, leading to prolonged bleeding and symptoms such as nosebleeds.
Practice Questions
Question 1: Erythropoiesis Regulation
What stimulates erythropoiesis?
A) Decreased oxygen saturation in the lungs
B) Increased erythropoietin production by the liver
C) Increased erythropoietin production by the kidneys
D) Decreased carbon dioxide levels in the blood
Correct Answer: C) Increased erythropoietin production by the kidneys
Explanation:
Erythropoiesis is stimulated by erythropoietin, a hormone predominantly produced by the kidneys. This process is typically triggered when oxygen levels in the blood decrease (hypoxia), prompting the kidneys to produce more erythropoietin, which then stimulates the bone marrow to produce more red blood cells. This mechanism helps to enhance the blood’s oxygen-carrying capacity.
Question 2: Functions of Blood Platelets
Which function is primarily associated with platelets?
A) Transport of oxygen
B) Defense against pathogens
C) Blood clotting
D) Hormone production
Correct Answer: C) Blood clotting
Explanation:
Platelets, or thrombocytes, play a critical role in hemostasis, the process of blood clotting. When a blood vessel is injured, platelets adhere to the vessel’s exposed collagen and form a plug, initiating a series of reactions that culminate in the formation of a blood clot. This process prevents excessive bleeding.
Question 3: Consequences of Leukemia
What is a common symptom of leukemia?
A) Elevated hemoglobin levels
B) Reduced risk of infections
C) Increased number of functional white blood cells
D) Frequent infections
Correct Answer: D) Frequent infections
Explanation:
Leukemia typically involves the proliferation of abnormal white blood cells in the bone marrow, which can crowd out normal blood cells. The abnormal white blood cells are often dysfunctional, leading to a compromised immune system. As a result, individuals with leukemia are more susceptible to infections.