Preparing for the MCAT requires a comprehensive understanding of the immune system, a pivotal component of the Organ Systems foundation. Mastery of immune responses, including innate and adaptive immunity, cellular and humoral components, and immunological memory, is crucial for insights into disease defense mechanisms, essential for a high MCAT score.
Learning Objective
In studying the "Immune System" for the MCAT, you should aim to understand the structures and functions of innate and adaptive immunity. Learn the roles of key immune cells like macrophages, T-cells, B-cells, and antibodies in defending against pathogens. Explore how the immune system recognizes and remembers foreign antigens, leading to a faster response upon re-exposure. Additionally, examine the pathophysiology of immune disorders such as allergies, autoimmune diseases, and immunodeficiencies. Apply this knowledge to interpret clinical case studies, laboratory data, and research findings in MCAT practice passages, focusing on the immune system's role in health and disease management.
Understanding the Immune System
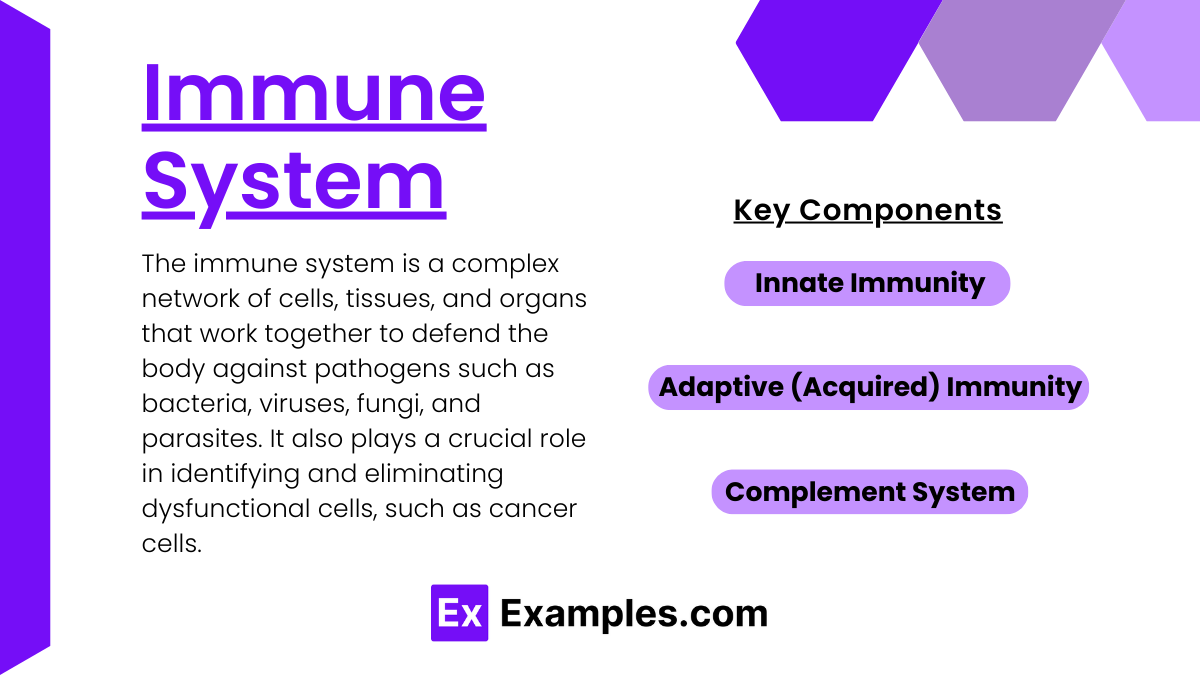
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against pathogens such as bacteria, viruses, fungi, and parasites. It also plays a crucial role in identifying and eliminating dysfunctional cells, such as cancer cells. Here’s an overview of how the immune system functions:
Components of the Immune System:
Innate Immunity:
The first line of defense, providing immediate response to invaders.
Includes physical barriers like the skin and mucous membranes, chemical barriers like stomach acid, and cellular defenses such as phagocytes (e.g., neutrophils and macrophages) that engulf and destroy pathogens.
Also involves natural killer (NK) cells that target and kill virus-infected cells and certain types of tumor cells.
Adaptive (Acquired) Immunity:
Develops as people are exposed to diseases or immunized through vaccination.
Consists of lymphocytes known as B cells and T cells which originate from stem cells in the bone marrow.
B cells: Mature in the bone marrow and are responsible for antibody production. Antibodies bind to specific antigens on pathogens, marking them for destruction.
T cells: Mature in the thymus and are crucial for cell-mediated immunity. Helper T cells activate other immune cells, while cytotoxic T cells directly kill infected or cancerous cells.
Features a memory component that allows for a faster and more effective response upon repeated exposure to the same pathogen.
Complement System:
A series of proteins that circulate in the blood and fluids. Upon recognition of a pathogen, they work in a cascade to lyse (break down) the pathogen’s cell wall, enhance phagocytosis, and stimulate inflammation.
Functions of the Immune System:
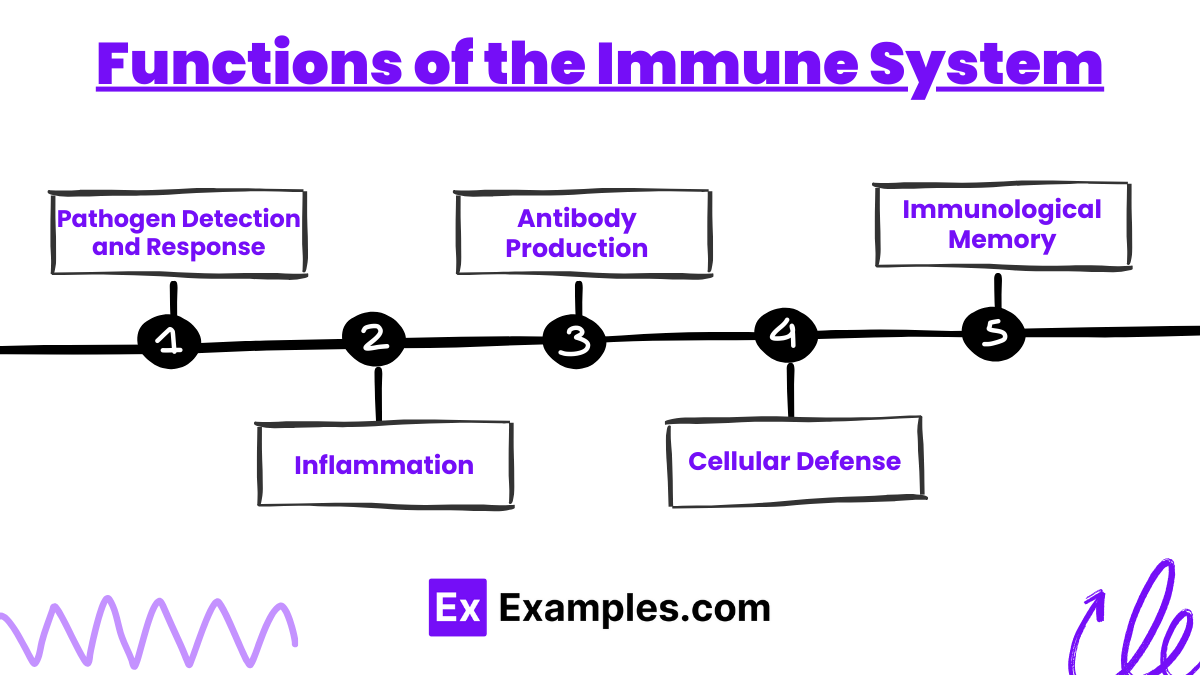
Pathogen Detection and Response:
Identifies harmful organisms and substances and initiates an immune response to neutralize or destroy them.
Inflammation:
A protective tissue response to injury or infection, resulting in increased blood flow (bringing more immune cells to the site), and the release of chemicals that promote healing and defend against pathogens.
Antibody Production:
B cells produce antibodies that specifically target antigens presented by pathogens, facilitating their destruction or removal.
Cellular Defense:
T cells and NK cells destroy infected or malignant cells directly, preventing the spread of infection and tumorigenesis.
Immunological Memory:
After an initial response, the immune system creates memory B cells and T cells that "remember" the pathogen, leading to a quicker and more efficient response to future infections by the same pathogen.
Pathophysiology of Immune Disorders
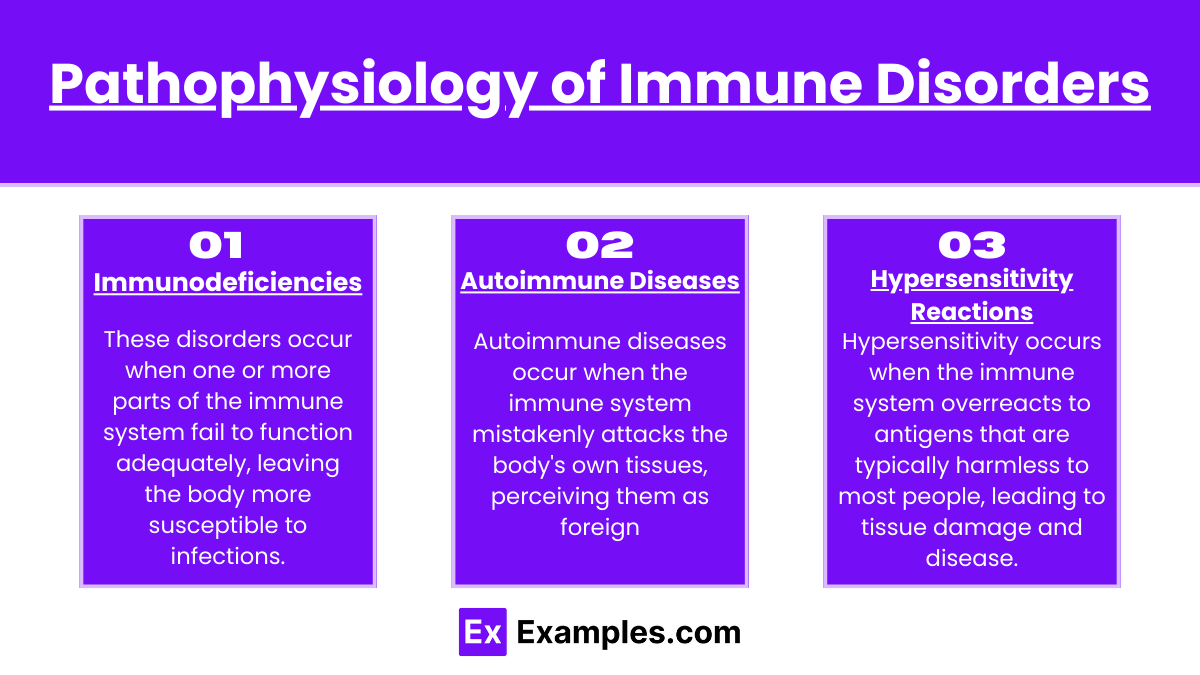
Immune disorders encompass a range of conditions that arise from improper function of the immune system. These can be broadly categorized into three main types: immunodeficiencies, autoimmune diseases, and hypersensitivity reactions. Here’s how these disorders affect the body:
1. Immunodeficiencies
These disorders occur when one or more parts of the immune system fail to function adequately, leaving the body more susceptible to infections.
Primary Immunodeficiencies are congenital and often genetic, such as Severe Combined Immunodeficiency (SCID) or Common Variable Immunodeficiency (CVID).
Secondary Immunodeficiencies are acquired due to external factors like infections (e.g., HIV/AIDS), malnutrition, or certain medications (e.g., chemotherapy).
Pathophysiology: In immunodeficiencies, the body lacks functional immune cells or molecules, such as antibodies or lymphocytes, leading to recurrent infections, delayed recovery from illnesses, and increased risk of developing certain cancers.
2. Autoimmune Diseases
Autoimmune diseases occur when the immune system mistakenly attacks the body's own tissues, perceiving them as foreign.
Examples include Type 1 Diabetes, where the immune system attacks pancreatic cells, Rheumatoid Arthritis (joint inflammation), and Systemic Lupus Erythematosus (affects skin, joints, kidneys, brain, and other organs).
Pathophysiology: Autoimmune reactions involve the production of autoantibodies or the activation of T cells that attack healthy cells and tissues. This can cause chronic inflammation, tissue damage, and functional impairments in the affected organs.
3. Hypersensitivity Reactions
Hypersensitivity occurs when the immune system overreacts to antigens that are typically harmless to most people, leading to tissue damage and disease.
Types:
Type I (Immediate) Hypersensitivity: Includes allergies to foods, pollens, and some medications, leading to symptoms from mild rashes to anaphylaxis (a severe, potentially life-threatening allergic reaction).
Type II (Cytotoxic) Hypersensitivity: The body makes antibodies that react with antigens on the surface of specific cells or tissues (e.g., blood transfusion reactions).
Type III (Immune Complex) Hypersensitivity: Formation of antigen-antibody complexes that deposit in tissues, causing inflammation and damage, such as in systemic lupus erythematosus.
Type IV (Delayed-Type) Hypersensitivity: Cell-mediated responses where T cells release cytokines that attract macrophages, leading to tissue damage; an example is contact dermatitis from poison ivy.
Diagnostic Techniques of Immune Disorders
The diagnosis and treatment of immune disorders are tailored to the specific type of immune dysfunction, whether it's an immunodeficiency, autoimmune disease, or hypersensitivity reaction. Advanced diagnostic techniques help identify the nature of the disorder, and treatments aim to manage symptoms and correct the underlying immune imbalance.
Blood Tests
Complete Blood Count (CBC): Assesses the levels and types of blood cells.
Immunoglobulin Levels: Measure the levels of various antibodies to assess immune function.
Autoantibody Tests: Identify antibodies that target the body's own tissues, indicative of autoimmune diseases.
Flow Cytometry: Analyzes the types of cells in the blood and can identify specific immune deficiencies.
ELISA (Enzyme-Linked Immunosorbent Assay): Detects and measures specific proteins or antibodies in the blood, useful for diagnosing allergies and autoimmune conditions.
Skin Tests
Allergy Testing: Exposes the skin to allergens and observes reactions, indicating hypersensitivity to specific substances.
Genetic Testing
Used to diagnose certain genetic immunodeficiencies and predict susceptibility to autoimmune diseases.
Imaging Studies
X-rays, CT scans, and MRI: These imaging modalities can identify structural abnormalities and inflammations in organs affected by autoimmune diseases.
Examples
Example 1: Inflammation Response to Bacterial Infection
Scenario: A cut on the skin becomes infected with bacteria.
Process: The innate immune system responds first with inflammation. Blood vessels dilate to increase blood flow, bringing more immune cells to the site. Neutrophils and macrophages enter the tissue from the bloodstream to phagocytize the bacteria, while cytokines attract more immune cells and cause fever and swelling.
Example 2: T-Cell Activation in Viral Infection
Scenario: Infection with a common virus like the flu.
Process: Virus-infected cells present viral antigens via MHC class I molecules. CD8+ cytotoxic T cells recognize these antigens, become activated, and kill the infected cells. Simultaneously, CD4+ helper T cells help activate B cells to produce virus-specific antibodies, enhancing the immune response.
Example 3: Formation of Immunological Memory After Vaccination
Scenario: Administration of a measles vaccine.
Process: The vaccine, containing live attenuated measles virus, stimulates the immune system without causing disease. B and T cells specific to measles virus antigens proliferate and form memory cells. These memory cells ensure a rapid and effective response to future measles infections, often preventing the disease entirely.
Example 4: Autoimmune Attack in Type 1 Diabetes
Scenario: Autoimmune destruction of pancreatic beta cells.
Process: In type 1 diabetes, the immune system mistakenly identifies beta cells in the pancreas as foreign and attacks them. This results in the inability to produce insulin, leading to elevated blood glucose levels. T cells infiltrate the pancreas, and antibodies against beta cells can be detected in the blood.
Example 5: Allergic Reaction to Bee Stings
Scenario: Severe allergic reaction (anaphylaxis) after a bee sting.
Process: In some individuals, the immune system overreacts to the venom in a bee sting. IgE antibodies bound to mast cells recognize the venom, triggering the cells to release large amounts of histamine. This leads to vasodilation, increased permeability of blood vessels, and symptoms like swelling, redness, difficulty breathing, and potentially, anaphylactic shock.
Practice Questions
Question 1: Immune Cell Functions
Which type of immune cell is primarily responsible for antibody production?
A) Macrophages
B) Cytotoxic T cells
C) B cells
D) Neutrophils
Correct Answer: C) B cells
Explanation:
B cells, a type of lymphocyte, are primarily responsible for the production of antibodies. Upon activation, B cells differentiate into plasma cells, which secrete large volumes of antibodies specific to the antigen encountered. These antibodies are crucial for identifying and neutralizing pathogens during an immune response.
Question 2: Immune Responses
What is the role of helper T cells in the adaptive immune response?
A) Directly kill infected cells
B) Phagocytize pathogens
C) Release cytokines to stimulate other immune cells
D) Produce antibodies
Correct Answer: C) Release cytokines to stimulate other immune cells
Explanation:
Helper T cells (CD4+ T cells) play a pivotal role in the adaptive immune response by releasing cytokines that stimulate and regulate the activity of other immune cells, including B cells, cytotoxic T cells, and macrophages. They are essential for both cell-mediated and humoral immune responses, coordinating the overall immune reaction.
Question 3: Pathological Conditions
Which condition is characterized by an excessive immune response to harmless antigens in the environment
A) Autoimmunity
B) Immunodeficiency
C) Hypersensitivity
D) Inflammation
Correct Answer: C) Hypersensitivity
Explanation:
Hypersensitivity refers to excessive or inappropriate immune responses to antigens that are typically harmless, such as pollen, pet dander, or certain foods. Common types of hypersensitivity reactions include allergies, where the immune system's overreaction can lead to symptoms ranging from mild irritation to life-threatening anaphylaxis.