Preparing for the MCAT requires a thorough understanding of the renal system, crucial for the Organ Systems foundation. Mastery of kidney functions, fluid and electrolyte balance, and waste excretion provides vital insights into maintaining homeostasis and is essential for achieving a high MCAT score.
Learning Objective
In studying the "Renal System" for the MCAT, you should aim to understand the structure and function of the kidneys, including nephron anatomy and the processes of glomerular filtration, tubular reabsorption, secretion, and excretion. Learn how the kidneys regulate volume, electrolyte balance, and acid-base status through hormonal influences like antidiuretic hormone (ADH), aldosterone, and the renin-angiotensin system. Additionally, explore renal compensation mechanisms in response to systemic changes, and understand common renal pathologies such as acute kidney injury and chronic kidney disease. Apply this knowledge to solve MCAT practice questions that test your ability to integrate and apply complex physiological concepts.
Understanding the Renal System
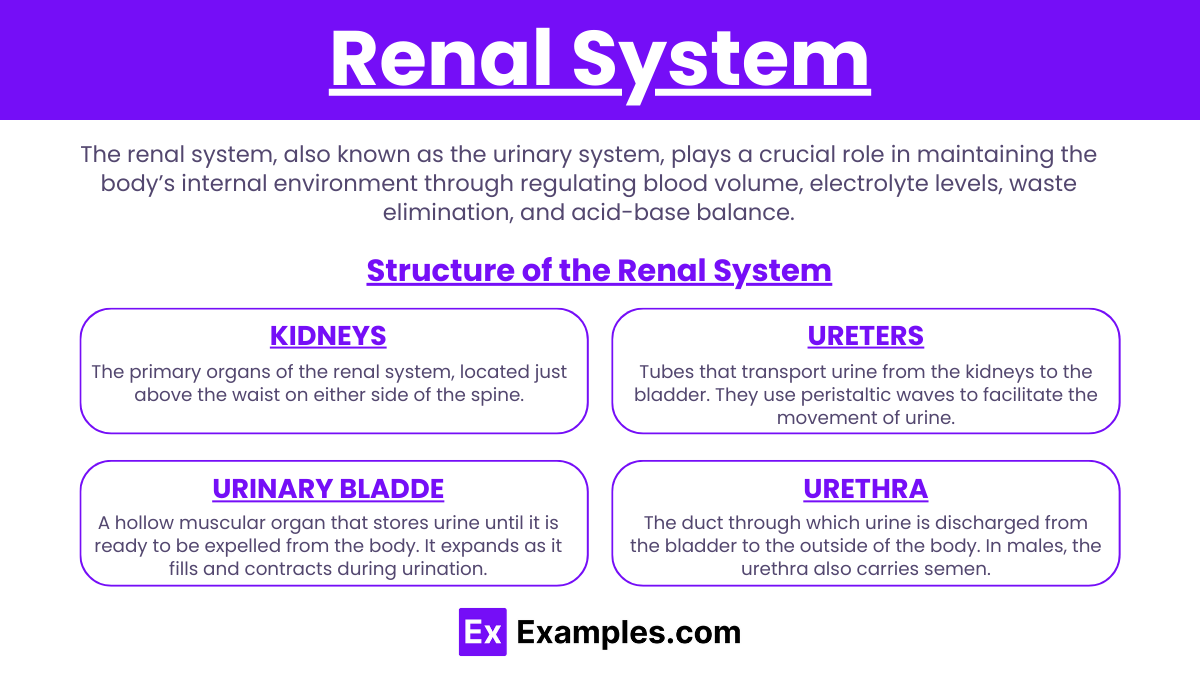
The renal system, also known as the urinary system, plays a crucial role in maintaining the body’s internal environment through regulating blood volume, electrolyte levels, waste elimination, and acid-base balance. Here's an overview of the structure of the renal system:
Structure of the Renal System
Kidneys:
The primary organs of the renal system, located just above the waist on either side of the spine. Each kidney contains about a million nephrons, the functional units that filter blood and produce urine.
Kidneys receive blood through the renal arteries and drain it via the renal veins.
Ureters:
Tubes that transport urine from the kidneys to the bladder. They use peristaltic waves to facilitate the movement of urine.
Urinary Bladder:
A hollow muscular organ that stores urine until it is ready to be expelled from the body. It expands as it fills and contracts during urination.
Urethra:
The duct through which urine is discharged from the bladder to the outside of the body. In males, the urethra also carries semen.
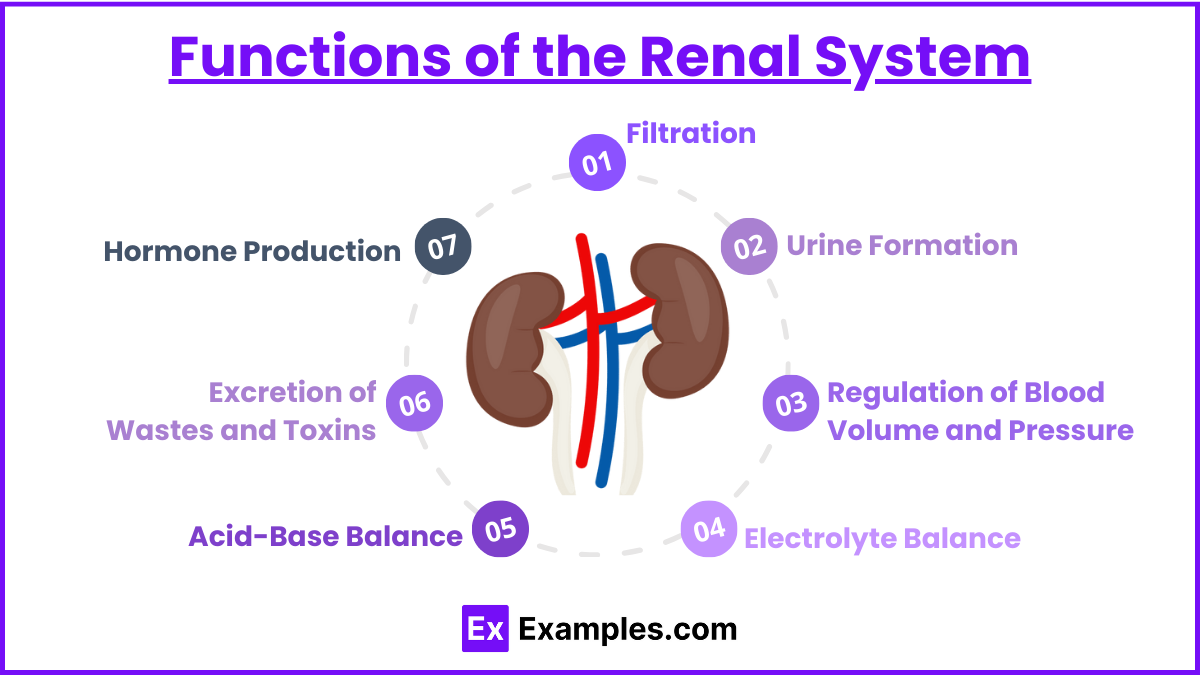
Functions of the Renal System
Filtration:
Blood enters the kidneys through the renal arteries, and nephrons filter out wastes, excess salts, and other substances. Useful substances like glucose, amino acids, and ions are reabsorbed back into the bloodstream.
Urine Formation:
The filtered fluid passes through the tubules of the nephron, where reabsorption and secretion alter its composition, forming urine.
Regulation of Blood Volume and Pressure:
Kidneys regulate blood volume by adjusting the volume of water excreted in urine. They also secrete renin, an enzyme that helps regulate blood pressure.
Electrolyte Balance:
The renal system regulates the concentration of electrolytes such as sodium, potassium, and chloride ions in the body.
Acid-Base Balance:
Kidneys help maintain the body’s pH by excreting hydrogen ions and reabsorbing bicarbonate from urine.
Excretion of Wastes and Toxins:
Kidneys filter out metabolic wastes (like urea and creatinine), drugs, and toxins from the blood, which are then excreted in urine.
Hormone Production:
Kidneys produce several hormones including erythropoietin, which stimulates red blood cell production; calcitriol, the active form of vitamin D that helps regulate calcium metabolism.
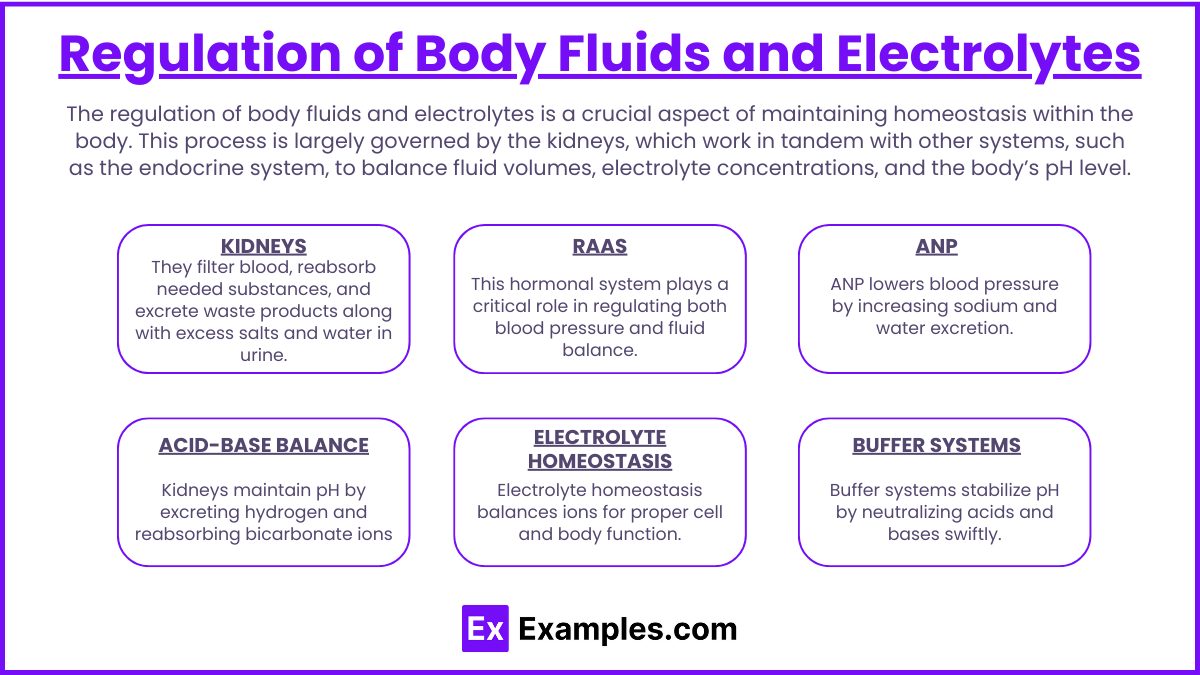
Regulation of Body Fluids and Electrolytes
The regulation of body fluids and electrolytes is a crucial aspect of maintaining homeostasis within the body. This process is largely governed by the kidneys, which work in tandem with other systems, such as the endocrine system, to balance fluid volumes, electrolyte concentrations, and the body’s pH level. Here’s how these components are regulated:
1. Kidneys
The primary regulators of fluid and electrolyte balance are the kidneys. They filter blood, reabsorb needed substances, and excrete waste products along with excess salts and water in urine. This activity is crucial for controlling the volume and composition of body fluids.
Fluid Balance: The kidneys adjust urine output based on hydration levels. This process is influenced by antidiuretic hormone (ADH), which the pituitary gland releases to increase water reabsorption in the kidney tubules when the body is dehydrated.
Electrolyte Balance: Kidneys regulate electrolytes such as sodium, potassium, and chloride by selectively reabsorbing what the body needs and excreting the rest. The reabsorption rates can be adjusted based on dietary intake and other physiological needs.
2. Renin-Angiotensin-Aldosterone System (RAAS)
This hormonal system plays a critical role in regulating both blood pressure and fluid balance.
Renin: Produced by the kidneys, renin converts angiotensinogen (from the liver) into angiotensin I, which is then converted into angiotensin II.
Angiotensin II: A potent vasoconstrictor that also stimulates the release of aldosterone from the adrenal cortex.
Aldosterone: Promotes sodium and water reabsorption in the kidneys, which increases blood volume and pressure.
3. Atrial Natriuretic Peptide (ANP)
Released by heart atria in response to high blood pressure, ANP counteracts the RAAS by promoting the excretion of sodium and water in urine, which decreases blood volume and lowers blood pressure.
4. Electrolyte Homeostasis
Sodium (Na+) is the most significant cation in extracellular fluid, crucial for maintaining osmotic balance and blood pressure.
Potassium (K+) is vital for cell function, including nerve impulse transmission and muscle contraction. It is the major cation within cells.
Calcium (Ca2+) is essential for bone health, muscle function, and neuronal signaling. Its levels are regulated by parathyroid hormone and vitamin D.
5. Acid-Base Balance
The kidneys regulate acid-base balance by excreting hydrogen ions and reabsorbing bicarbonate from urine. This renal regulation works alongside buffering systems in the blood to maintain a stable pH.
6. Buffer Systems
Bicarbonate Buffer System: The primary buffer for maintaining blood pH, which involves a balance between bicarbonate ions (HCO3-) and carbonic acid (H2CO3).
Protein Buffers: Hemoglobin and other proteins help buffer acids and bases within cells and blood.
Phosphate Buffer System: Functions primarily in the kidneys and intracellular fluids, balancing pH by utilizing phosphate ions.
Pathophysiology of Renal Disorders
Renal disorders encompass a broad range of conditions affecting the kidneys’ ability to function effectively, impacting fluid balance, waste elimination, electrolyte management, and blood pressure regulation. Here’s a look at the pathophysiology behind common renal disorders:
1. Chronic Kidney Disease (CKD)
Pathophysiology: CKD is characterized by a gradual loss of kidney function over time. This is often caused by long-term damage from conditions like hypertension, diabetes, or autoimmune diseases, leading to nephron loss and decreased glomerular filtration rate (GFR).
Implications: Reduced kidney function results in the accumulation of waste products, fluid imbalance, electrolyte disturbances, and an increased risk of cardiovascular disease.
2. Acute Kidney Injury (AKI)
Pathophysiology: AKI involves a sudden reduction in kidney function, usually due to acute tubular necrosis from toxins, drugs, or ischemia (lack of oxygen), which damages kidney tissues.
Implications: This can lead to rapid accumulation of waste products, disturbances in electrolyte and acid-base balance, and fluid overload, which can be life-threatening if not promptly addressed.
3. Glomerulonephritis
Pathophysiology: Inflammation of the glomeruli, often caused by autoimmune diseases, infections, or systemic diseases like lupus. The inflammation impairs the kidneys' ability to filter blood.
Implications: Results in proteinuria (protein in urine), hematuria (blood in urine), reduced GFR, and potential progression to chronic kidney disease.
4. Polycystic Kidney Disease (PKD)
Pathophysiology: A genetic disorder characterized by the growth of numerous cysts filled with fluid in the kidneys. These cysts replace much of the mass of the kidneys, reducing kidney function and leading to kidney failure.
Implications: Hypertension, kidney stones, and renal failure are common complications.
5. Nephrolithiasis (Kidney Stones)
Pathophysiology: Crystals of substances such as calcium, oxalate, or uric acid form stones in the kidneys, often when the urine becomes too concentrated.
Implications: Stones can cause severe pain, obstruct urine flow, and lead to infection or kidney damage if they cause persistent blockage.
6. Urinary Tract Infections (UTIs)
Pathophysiology: Infections usually caused by bacteria that enter the urinary tract, which can also ascend to affect the bladder and kidneys.
Implications: If the infection reaches the kidneys, it can cause acute or chronic kidney infections, potentially leading to permanent kidney damage.
Examples
Example 1: Regulation of Blood Pressure via the RAAS
Scenario: Decreased blood pressure detected by the kidneys.
Process: In response to low blood pressure, the juxtaglomerular cells in the kidneys secrete renin, which converts angiotensinogen (from the liver) into angiotensin I. Angiotensin I is then converted to angiotensin II by ACE (angiotensin-converting enzyme) in the lungs. Angiotensin II acts to constrict blood vessels, increase sodium reabsorption (thus increasing water retention), and stimulate aldosterone release, collectively raising blood pressure.
Example 2: Acute Kidney Injury (AKI) Due to Hypovolemia
Scenario: A patient suffers significant blood loss after an accident.
Process: The reduced blood volume leads to decreased renal blood flow, impairing the kidneys' ability to filter blood. This acute drop in filtration can cause a build-up of waste products in the blood, characteristic of AKI, requiring immediate medical intervention to restore renal function and prevent permanent damage.
Example 3: Diuretics' Role in Hypertension
Scenario: A patient with chronic hypertension is prescribed diuretics.
Process: Diuretics work by blocking sodium reabsorption in the nephron, particularly in the loop of Henle, distal convoluted tubule, or collecting duct. This inhibition results in increased sodium and water excretion, decreasing blood volume and, consequently, blood pressure.
Example 4: Glomerulonephritis and Proteinuria
Scenario: Inflammation of the glomeruli due to an autoimmune response.
Process: In glomerulonephritis, the immune system damages the glomeruli, leading to a decrease in their filtering capacity. This allows proteins, which are normally retained in the blood, to pass into the urine, resulting in proteinuria—an early sign of kidney disease.
Example 5: Chronic Kidney Disease (CKD) and Electrolyte Imbalance
Scenario: Progression of CKD in a patient with diabetes.
Process: As kidney function declines due to damage from high blood sugar levels over time, the kidneys' ability to filter blood deteriorates. This results in the accumulation of waste products and imbalances in electrolytes, particularly potassium, which can lead to dangerous conditions such as hyperkalemia.
Practice Questions
Question 1: Glomerular Filtration Rate (GFR)
What effect does constriction of the afferent arteriole have on the glomerular filtration rate (GFR) and renal plasma flow?
A) Increase both GFR and renal plasma flow
B) Decrease both GFR and renal plasma flow
C) Increase GFR and decrease renal plasma flow
D) Decrease GFR and increase renal plasma flow
Correct Answer: B) Decrease both GFR and renal plasma flow
Explanation:
Constriction of the afferent arteriole reduces the amount of blood reaching the glomeruli, which decreases renal plasma flow. This reduction in blood flow leads to a decrease in the pressure inside the glomerular capillaries, thereby lowering the glomerular filtration rate (GFR).
Question 2: Effects of ADH (Antidiuretic Hormone)
Which of the following best describes the action of antidiuretic hormone (ADH) on the kidneys?
A) ADH causes the kidneys to excrete more urine.
B) ADH decreases blood pressure by causing vasodilation.
C) ADH promotes reabsorption of water in the collecting ducts.
D) ADH decreases sodium reabsorption in the distal convoluted tubule.
Correct Answer: C) ADH promotes reabsorption of water in the collecting ducts
Explanation:
Antidiuretic hormone (ADH) acts on the collecting ducts in the kidneys by increasing their permeability to water. This effect allows more water to be reabsorbed back into the bloodstream, reducing urine volume and concentrating the urine, which helps to maintain body water balance.
Question 3: Kidney Response to Acidosis
How do the kidneys compensate for metabolic acidosis?
A) By increasing bicarbonate reabsorption
B) By decreasing bicarbonate reabsorption
C) By increasing bicarbonate secretion
D) By decreasing bicarbonate secretion
Correct Answer: A) By increasing bicarbonate reabsorption
Explanation:
In response to metabolic acidosis, the kidneys compensate by increasing the reabsorption of bicarbonate ions (HCO3-) from the filtrate back into the blood. This process helps to buffer the excess hydrogen ions in the bloodstream, raising the pH towards normal levels.