Preparing for the MCAT requires a comprehensive understanding of the reproductive system, a crucial component of the Organ Systems foundation. Mastery of male and female reproductive anatomy, hormonal regulation, and reproductive cycles is essential. This knowledge provides insights into human development, fertility, and reproductive health, critical for achieving a high MCAT score.
Learning Objective
In studying the "Reproductive System" for the MCAT, you should aim to understand the anatomy, physiology, and hormonal regulation of the male and female reproductive systems. Explore the mechanisms of gametogenesis, fertilization, and embryonic development. Learn the roles of key hormones such as estrogen, progesterone, testosterone, LH, and FSH in regulating reproductive functions and cycles. Additionally, examine common reproductive disorders and their treatments, including infertility issues and hormonal imbalances. Apply this knowledge to solve MCAT practice questions that test your ability to integrate and apply comprehensive knowledge of reproductive health, development, and endocrine regulation.
Anatomy and Physiology of the Reproductive System
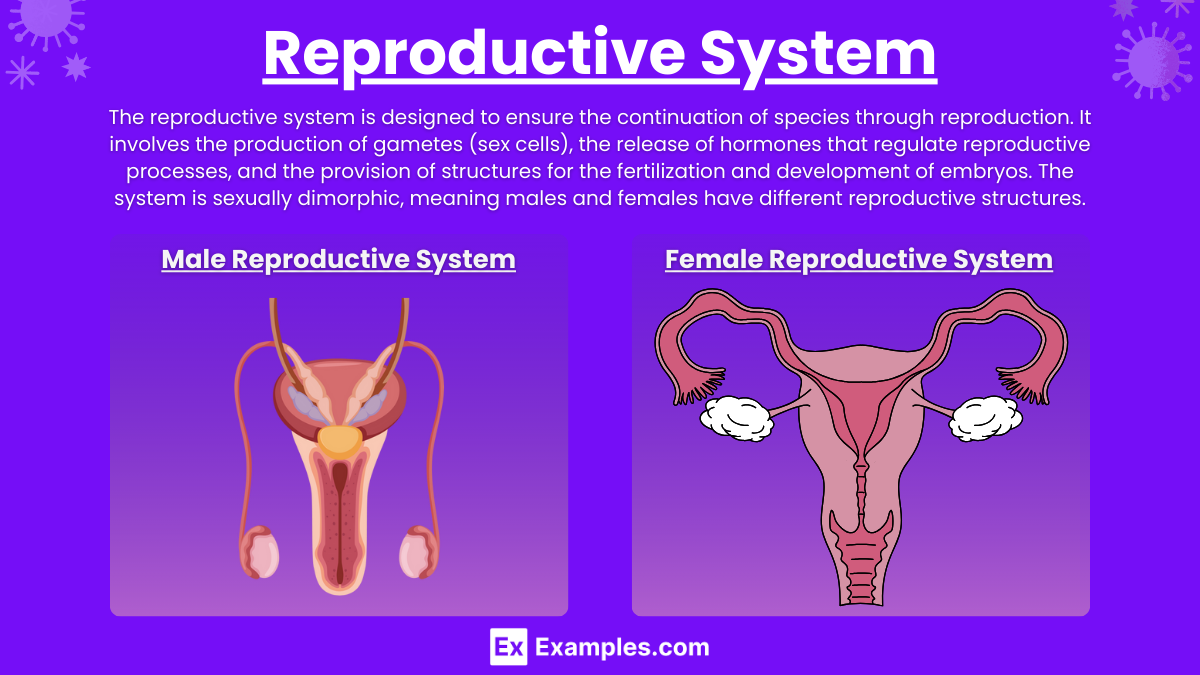
The reproductive system is designed to ensure the continuation of species through reproduction. It involves the production of gametes (sex cells), the release of hormones that regulate reproductive processes, and the provision of structures for the fertilization and development of embryos. The system is sexually dimorphic, meaning males and females have different reproductive structures. Here's an overview of the anatomy and physiology of the reproductive system in humans:
Male Reproductive System
Anatomy:
Testes: Paired organs housed in the scrotum responsible for producing sperm and testosterone.
Epididymis: A coiled tube where sperm mature and are stored.
Vas Deferens: Tubes that transport sperm from the epididymis to the urethra.
Urethra: Conducts sperm (and urine) out of the body through the penis.
Seminal Vesicles, Prostate Gland, and Bulbourethral Glands: Produce seminal fluid, which mixes with sperm to form semen.
Penis: Organ of copulation; delivers semen into the female reproductive tract.
Physiology:
Spermatogenesis: The production of sperm cells in the testes.
Hormonal Regulation: Testosterone, produced in the testes, regulates male sexual development and secondary sexual characteristics. The hypothalamus and pituitary gland control testicular function through the secretion of hormones like gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH).
Female Reproductive System
Anatomy:
Ovaries: Paired organs that produce eggs (ova) and hormones, including estrogen and progesterone.
Fallopian Tubes: Tubes through which eggs travel from the ovaries to the uterus.
Uterus: Hollow organ where a fertilized egg implants and an embryo develops.
Cervix: The lower part of the uterus that opens into the vagina.
Vagina: The canal leading from the cervix to the outside of the body; receives semen during intercourse and serves as the birth canal.
Physiology:
Oogenesis: The production of egg cells.
Menstrual Cycle: Regular changes in the female reproductive system that make pregnancy possible, regulated by cyclic changes in hormone levels.
Hormonal Regulation: The hypothalamus and pituitary gland control ovarian function; hormones such as GnRH, FSH, and LH play key roles. Estrogen and progesterone are crucial for regulating the menstrual cycle and preparing the body for pregnancy.
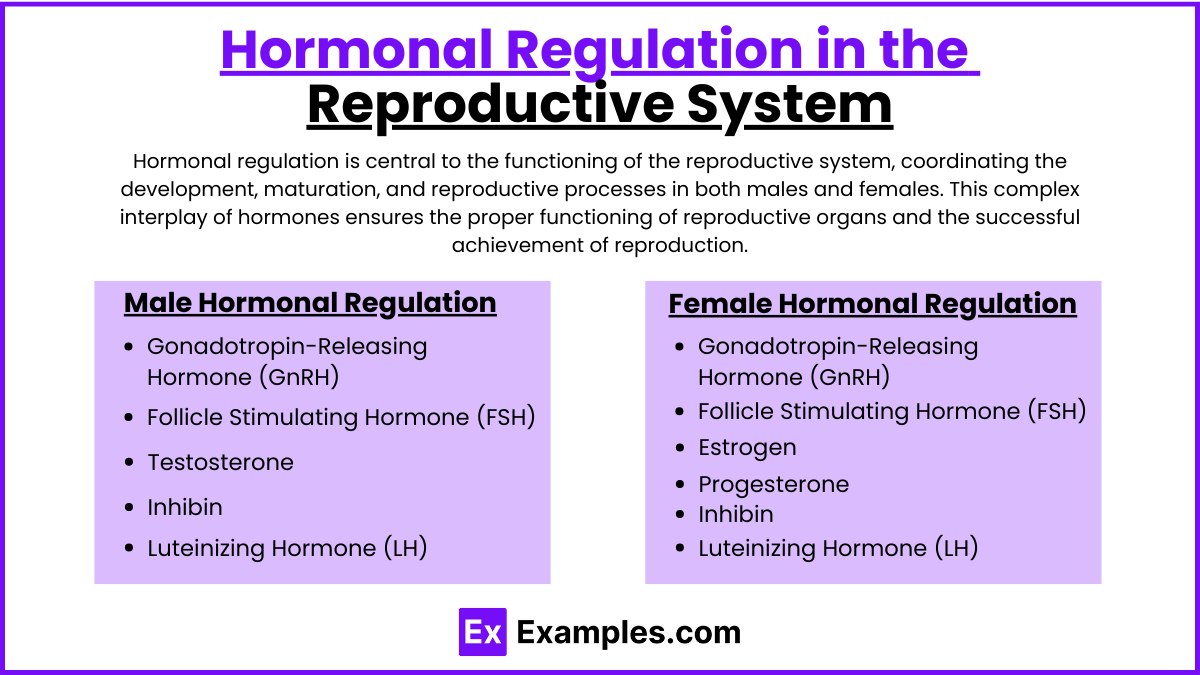
Hormonal Regulation in the Reproductive System
Hormonal regulation is central to the functioning of the reproductive system, coordinating the development, maturation, and reproductive processes in both males and females. This complex interplay of hormones ensures the proper functioning of reproductive organs and the successful achievement of reproduction. Here's a breakdown of how hormones regulate the reproductive system:
Male Hormonal Regulation
Gonadotropin-Releasing Hormone (GnRH):
Secreted by the hypothalamus.
Stimulates the pituitary gland to release Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH).
Follicle Stimulating Hormone (FSH):
In males, FSH stimulates the Sertoli cells in the testes to aid in sperm maturation.
Luteinizing Hormone (LH):
Stimulates the Leydig cells in the testes to produce testosterone.
Testosterone:
Produced by the testes.
Regulates the development of male secondary sexual characteristics (e.g., muscle mass, voice deepening, facial hair).
Plays a key role in the production of sperm.
Inhibin:
Produced by the Sertoli cells in the testes.
Helps regulate the production of FSH via negative feedback to the anterior pituitary.
Female Hormonal Regulation
Gonadotropin-Releasing Hormone (GnRH):
Secreted by the hypothalamus.
Stimulates the pituitary to release FSH and LH.
Follicle Stimulating Hormone (FSH):
In females, FSH stimulates the growth of ovarian follicles in the ovary each month.
Luteinizing Hormone (LH):
Triggers ovulation (release of the mature egg from the ovary).
Promotes the formation of the corpus luteum, which secretes progesterone.
Estrogen:
Produced mainly by the ovaries.
Responsible for the development of female secondary sexual characteristics (e.g., breast development, regulation of menstrual cycle).
Prepares the endometrium for potential pregnancy after ovulation and regulates the menstrual cycle.
Progesterone:
Also produced by the ovaries post-ovulation.
Prepares the uterus for pregnancy and maintains the endometrium throughout pregnancy.
Regulates changes in the cervical mucus.
Inhibin:
Produced by the ovaries.
Inhibits FSH production to prevent the release of multiple eggs during one menstrual cycle.
Reproductive Disorders
Reproductive health is crucial for overall well-being and involves the proper functioning of the reproductive system and the ability to have a responsible, satisfying, and safe sex life. Disorders of the reproductive system can affect both males and females, impacting fertility, sexual function, and general health. Here’s an overview of common reproductive health issues and disorders:
Common Disorders in Males
Erectile Dysfunction (ED):
Inability to achieve or maintain an erection suitable for intercourse. Causes include vascular disease, diabetes, psychological issues, and neurological conditions.
Prostatitis:
Inflammation of the prostate gland, often causing painful or difficult urination. Can be caused by bacterial infections or non-specific inflammatory conditions.
Benign Prostatic Hyperplasia (BPH):
Enlargement of the prostate gland that can interfere with urinary flow. Common in older men.
Prostate Cancer:
One of the most common cancers in men, which may grow slowly and is initially confined to the prostate gland, where it may not cause serious harm.
Testicular Disorders:
Includes testicular torsion, varicocele, and testicular cancer. These conditions can affect testicular function and fertility.
Common Disorders in Females
Polycystic Ovary Syndrome (PCOS):
A hormonal disorder causing enlarged ovaries with small cysts on the outer edges. Symptoms include menstrual irregularity, excess hair growth, acne, and obesity.
Endometriosis:
Condition where tissue similar to the lining inside the uterus grows outside it, leading to pain and potential fertility problems.
Uterine Fibroids:
Noncancerous growths in the uterus that can cause heavy menstrual bleeding, pain, and, in some cases, infertility.
Ovarian Cysts:
Fluid-filled sacs in or on the ovary. Most cysts are harmless and resolve without treatment.
Breast Cancer:
Cancer that forms in the cells of the breasts, one of the most common cancers diagnosed in women.
Examples
Example 1: Hormonal Control of the Menstrual Cycle
Scenario: Normal menstrual cycle regulation.
Process: The menstrual cycle is regulated by hormones such as FSH and LH from the pituitary gland and estrogen and progesterone from the ovaries. FSH stimulates follicle growth; LH triggers ovulation. Estrogen prepares the endometrium for possible pregnancy, and progesterone maintains it post-ovulation. If fertilization doesn’t occur, hormone levels drop, leading to menstruation.
Example 2: Spermatogenesis
Scenario: Sperm production in the testes.
Process: Spermatogenesis occurs in the seminiferous tubules of the testes, where spermatogonia divide and differentiate into mature spermatozoa. This process is stimulated by testosterone and regulated by FSH and LH, involving stages of meiosis and spermiogenesis, culminating in the formation of sperm cells.
Example 3: Polycystic Ovary Syndrome (PCOS)
Scenario: A common endocrine disorder in women.
Process: PCOS is characterized by hormonal imbalance, including elevated levels of androgens, which can disrupt the menstrual cycle and ovulation. Symptoms include irregular menstrual periods, excessive hair growth, acne, and obesity. PCOS is also a common cause of infertility due to the lack of ovulation.
Example 4: Erectile Dysfunction
Scenario: Impaired ability to maintain an erection suitable for sexual intercourse.
Process: Erectile dysfunction can result from both psychological factors, such as anxiety or stress, and physiological factors, such as impaired blood flow to the penis or neurological issues. Treatment may involve medications that enhance blood flow, hormone therapy, or counseling.
Example 5: Assisted Reproductive Technology (ART)
Scenario: Couples facing infertility seeking medical assistance to conceive.
Process: Techniques such as IVF involve extracting eggs, retrieving a sperm sample, and then manually combining an egg and sperm in a laboratory dish. The embryo is then transferred to the uterus. Other techniques may involve hormone therapies to stimulate the ovaries to produce multiple eggs for retrieval.
Practice Questions
Question 1: Regulation of Menstrual Cycle
Which hormone is primarily responsible for the thickening of the endometrium during the proliferative phase of the menstrual cycle? A) Luteinizing hormone (LH)
B) Progesterone
C) Follicle-stimulating hormone (FSH)
D) Estrogen
Correct Answer: D) Estrogen
Explanation:
Estrogen is the hormone primarily responsible for the thickening of the endometrium during the proliferative phase of the menstrual cycle. It is secreted by the developing follicles in the ovaries and works to regenerate and thicken the endometrial lining in preparation for a potential pregnancy following ovulation.
Question 2: Hormonal Influence in Males
What is the primary function of luteinizing hormone (LH) in males? A) To stimulate sperm production
B) To promote testosterone secretion
C) To inhibit testosterone secretion
D) To increase follicle development
Correct Answer: B) To promote testosterone secretion
Explanation:
In males, luteinizing hormone (LH) primarily stimulates the Leydig cells in the testes to secrete testosterone. Testosterone is crucial for the normal development of male sexual characteristics, the stimulation of sperm production (spermatogenesis), and overall reproductive health.
Question 3: Causes of Infertility
Which condition is a common cause of infertility in women? A) Polycystic ovary syndrome (PCOS)
B) Increased production of estrogen
C) Decreased production of LH
D) Hyperactivity of the endometrium
Correct Answer: A) Polycystic ovary syndrome (PCOS)
Explanation:
Polycystic ovary syndrome (PCOS) is a common endocrine disorder among women of reproductive age and a frequent cause of infertility. It is characterized by hormonal imbalance, which can prevent regular ovulation. Symptoms often include irregular menstrual cycles, excess androgen levels, and polycystic ovaries.