Social structures refer to the organized patterns of relationships and institutions that shape how individuals interact within a society. These structures include family, education, healthcare, religion, and government systems, influencing behavior, access to resources, and societal norms. Understanding social structures is crucial for the MCAT, as it connects social dynamics with healthcare outcomes, such as how stratification affects access to medical care. Mastery of these concepts equips future physicians to address health disparities by recognizing the societal factors influencing patient care and well-being.
Learning Objectives
In studying "Social Structures" for the MCAT, you should understand how societal frameworks, including family, education, healthcare, religion, and government, shape individual behavior and interactions. Analyze how these structures influence access to resources, social mobility, and health outcomes. Evaluate key sociological theories such as functionalism, conflict theory, symbolic interactionism, and social constructionism. Explore the role of social institutions and stratification in perpetuating inequalities. Additionally, apply your knowledge to interpret how social structures affect healthcare delivery and public health outcomes, ensuring that you can analyze these dynamics effectively in MCAT passages and real-world scenarios.
1. Theoretical Approaches to Understanding Social Structures
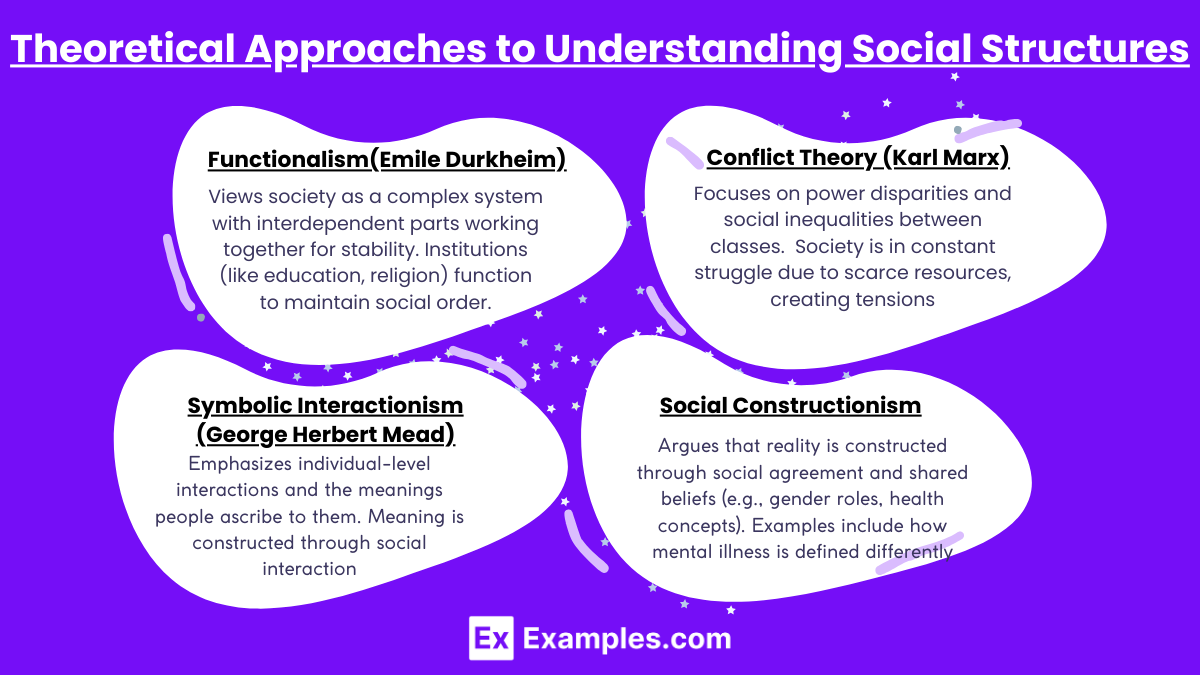
Functionalism (Emile Durkheim):
Views society as a complex system with interdependent parts working together for stability.
Institutions (like education, religion) function to maintain social order.
Manifest and latent functions: Manifest are intended (e.g., education teaches skills), while latent are unintended (e.g., schools provide social networks).
Conflict Theory (Karl Marx):
Focuses on power disparities and social inequalities between classes.
Society is in constant struggle due to scarce resources, creating tensions (e.g., wealth, status, healthcare access).
Highlights issues like healthcare inequality and systemic oppression.
Symbolic Interactionism (George Herbert Mead):
Emphasizes individual-level interactions and the meanings people ascribe to them.
Meaning is constructed through social interaction (e.g., the concept of illness varies across cultures).
Social Constructionism:
Argues that reality is constructed through social agreement and shared beliefs (e.g., gender roles, health concepts).
Examples include how mental illness is defined differently across cultures and historical periods.
2. Social Institutions and Their Impact on Health
Social institutions such as family, education, religion, economy, and government play a crucial role in shaping health outcomes and access to healthcare. These institutions create structures and norms that influence individual behaviors, public policies, healthcare delivery, and the distribution of resources, ultimately impacting the health and well-being of populations.
Family:
Provides emotional and material support but varies in structure (nuclear vs. extended families).
Family structure impacts health outcomes, such as maternal health or child care practices.
Education:
Access to education influences socioeconomic status and healthcare access.
Education-related disparities may lead to differences in health literacy.
Religion:
Offers psychological support and community resources but may influence healthcare decisions (e.g., faith healing vs. medical intervention).
Can promote both health behaviors and risky behaviors (e.g., stigma around certain medical treatments).
Government and Economy:
Government policies shape public healthcare systems (e.g., Medicaid, Medicare).
Economic inequality leads to health disparities, particularly in access to quality healthcare.
Healthcare and Medicine:
Institutional healthcare systems influence how medical care is provided.
Social determinants of health (e.g., environment, social status) impact individual outcomes.
3. Social Inequality and Stratification
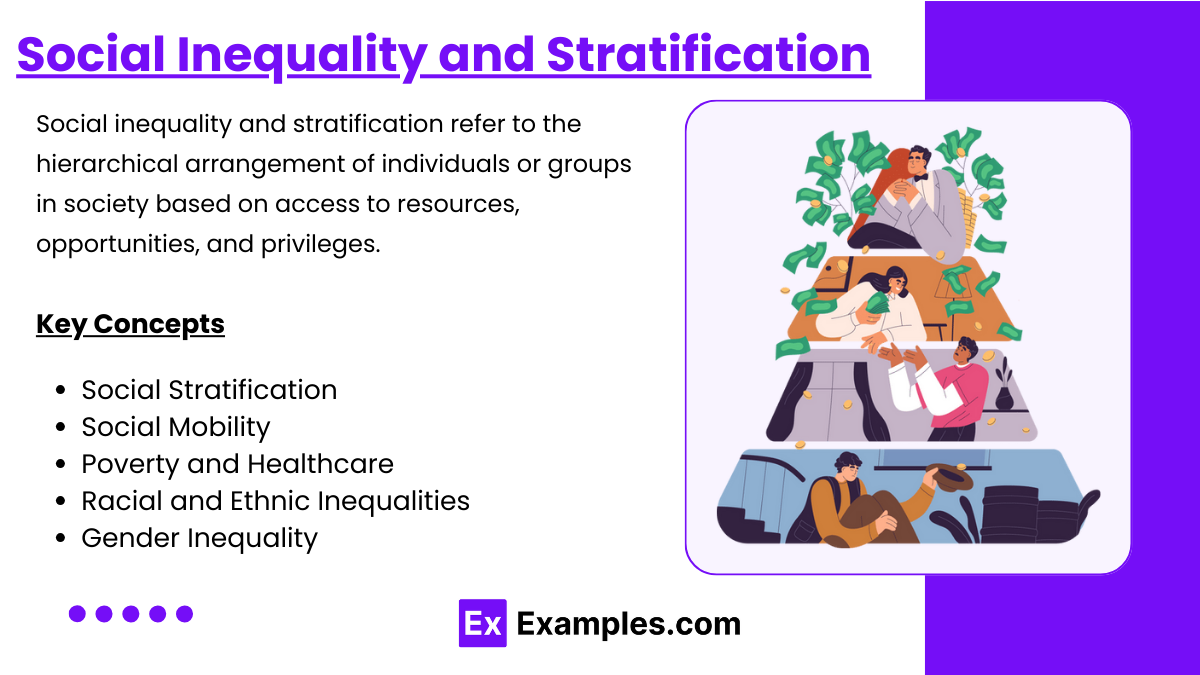
Social inequality and stratification refer to the hierarchical arrangement of individuals or groups in society based on access to resources, opportunities, and privileges. These differences shape life outcomes by affecting wealth, power, and social status. Stratification systems categorize individuals based on criteria such as class, race, gender, and education, perpetuating inequalities across generations.
Social Stratification:
Hierarchical arrangement of individuals into classes based on wealth, power, or status.
Class systems (like upper, middle, and lower class) determine access to resources.
Social Mobility:
Ability to move up or down the social hierarchy.
Limited mobility leads to persistent health disparities.
Poverty and Healthcare:
Poverty restricts access to healthcare services and nutritious food.
Low-income individuals are more likely to experience chronic health conditions.
Racial and Ethnic Inequalities:
Racial and ethnic minorities face systemic barriers in healthcare.
Disparities exist in treatment options, preventive care, and outcomes.
Gender Inequality:
Gender roles affect healthcare access and decision-making.
Women and LGBTQ+ populations may experience healthcare discrimination.
4. Demographics and Social Change
Population Dynamics:
Birth rates, death rates, and migration influence the size and structure of populations.
Fertility rates: Higher in developing countries; affect healthcare infrastructure needs.
Demographic Transition Theory:
Describes changes in birth and death rates as a country develops.
Healthcare systems must adapt to aging populations in developed nations.
Age and Aging:
Aging populations strain healthcare systems due to increased chronic diseases.
Elderly individuals face unique challenges like ageism and healthcare access barriers.
Urbanization:
Movement from rural to urban areas impacts health (e.g., more access to hospitals but higher pollution levels).
5. Health Disparities and Social Determinants of Health
Social Determinants of Health:
Factors outside of healthcare affecting health, such as education, income, and environment.
Health Disparities:
Differences in health outcomes due to socioeconomic, racial, or gender inequality.
Addressing these disparities requires public health initiatives and policy changes.
Global Inequality and Health:
Low-income countries often face higher rates of infectious diseases and lower life expectancy.
Healthcare access is uneven across and within countries, exacerbating inequality.
Examples
Example 1: Family Structure
Families play a foundational role in shaping individual behavior and providing emotional, financial, and social support. Family structures vary across cultures, ranging from nuclear families (parents and children) to extended families (including grandparents and other relatives). In healthcare, family roles can influence medical decision-making, such as who consents for a child's treatment or supports elderly care. MCAT questions may assess how family dynamics affect health outcomes, such as parental involvement in child development or caregiving for the elderly.
Example 2: Educational Institutions
Schools and universities serve as formal social structures that transmit knowledge, develop skills, and shape social behavior. They also promote social mobility by providing individuals with qualifications needed for better job opportunities. However, disparities in access to education can create health inequities, as less-educated individuals may struggle with health literacy and accessing care. The MCAT may focus on the role of education in social stratification and its impact on public health, such as differences in vaccination rates between populations with varying levels of education.
Example 3: Healthcare System
Healthcare institutions represent formal social structures responsible for maintaining and improving public health. These systems are composed of hospitals, clinics, healthcare professionals, and public health agencies. The structure of healthcare delivery impacts patient outcomes, with access to care varying by location, insurance coverage, and socioeconomic status. The MCAT may ask about healthcare inequalities, such as how the lack of access to preventive care leads to chronic health problems in marginalized populations.
Example 4: Religious Institutions
Religion influences individual behavior, social cohesion, and values, and religious institutions act as social structures within communities. These institutions often provide moral guidance, social support, and charitable services, such as free health clinics or food assistance. However, religious beliefs can also impact healthcare decisions, such as opposition to certain medical treatments (e.g., blood transfusions). MCAT questions may explore the intersection between religious beliefs and healthcare practices, highlighting potential conflicts or areas of collaboration.
Example 5: Government and Legal Systems
Governments create and enforce laws that regulate behavior and maintain social order. They play a critical role in shaping public health policies, such as vaccination programs, food safety regulations, and access to healthcare. Legal systems also influence individual rights and the allocation of resources, such as disability benefits or healthcare subsidies. The MCAT may assess how public policy decisions affect health outcomes, such as the impact of healthcare reform laws on uninsured populations or the role of social services in addressing public health crises.
Practice Questions
Question 1
Which of the following is an example of formal social structures?
A) Family relationships
B) Friend groups
C) Educational institutions
D) Personal values
Recommended Answer: C) Educational institutions
Explanation:
Educational institutions are a key example of formal social structures. They are systematically organized with defined roles (such as teachers and students), rules, and functions, serving to transmit knowledge and social norms. These institutions play a vital role in shaping individuals' behavior and social mobility.
Family relationships (A) and friend groups (B) are informal structures. While they shape personal behaviors, they lack the same level of formal regulation found in institutions like schools.
Personal values (D) are individual characteristics rather than social structures, although they can be influenced by societal norms.
Question 2
How do healthcare systems function as a social structure?
A) They promote social cohesion through informal networks.
B) They regulate public behavior through formal policies and medical services.
C) They act as platforms for religious expression and spirituality.
D) They focus solely on individual health behaviors without societal impact.
Recommended Answer: B) They regulate public behavior through formal policies and medical services.
Explanation:
Healthcare systems are formal social structures consisting of institutions like hospitals, clinics, and public health organizations. They enforce regulations (such as vaccination policies) that shape public behavior, ensuring collective well-being.
Option A is incorrect because social cohesion is not the primary function of healthcare systems, although they contribute to societal stability.
Option C relates to religious institutions rather than healthcare.
Option D is inaccurate as healthcare systems have both individual and societal impacts, influencing public health outcomes through preventive care and policy initiatives.
Question 3
Which of the following best reflects the impact of social stratification on health outcomes?
A) Equal access to healthcare services across all socioeconomic classes
B) Increased mobility between social classes leading to reduced health disparities
C) Disparities in access to healthcare based on income, race, or education
D) Decreased need for healthcare as people move up the social ladder
Recommended Answer: C) Disparities in access to healthcare based on income, race, or education
Explanation:
Social stratification refers to the hierarchical division of society into different classes based on factors like wealth, status, or education. This hierarchy often results in unequal access to healthcare, with marginalized populations facing greater barriers to quality care.
Option A is incorrect because healthcare access is not equal across all social groups.
Option B describes social mobility, but mobility is often limited, and disparities persist.
Option D is inaccurate because higher social mobility does not eliminate the need for healthcare; rather, access improves with higher socioeconomic status.