The Maternal & Newborn Health: Antepartum period is a critical phase in pregnancy that spans from conception to the onset of labor. For the NCLEX-PN®, understanding antepartum care is essential for promoting maternal and fetal health. This period involves comprehensive care, including prenatal assessments, health education, early detection of complications, and routine screenings. Nurses play a vital role in ensuring a safe pregnancy by monitoring physiological changes, supporting emotional well-being, and educating expectant mothers on lifestyle modifications, nutrition, and recognizing signs of potential complications.
Learning Objectives
In studying "Maternal & Newborn Health: Antepartum" for the NCLEX-PN® Exam, you should learn to understand the principles of antepartum care, focusing on maternal and fetal well-being. Analyze the roles and responsibilities of nurses in prenatal assessment, health education, and complication management. Evaluate factors affecting antepartum care, such as physiological changes, maternal health status, and fetal development. Explore nursing considerations like patient education, risk assessment, and timely intervention for complications like preeclampsia and gestational diabetes. Apply knowledge to ensure comprehensive prenatal care, effective communication, and appropriate monitoring to support maternal health, promote fetal growth, and maintain pregnancy safety and care quality.
1. Antepartum Care and Assessment
Antepartum care focuses on maintaining maternal and fetal health throughout pregnancy. It includes regular assessments, patient education, and timely identification of risks or complications.
1. Initial Prenatal Visit
Comprehensive History Collection: Collect obstetric, gynecologic, medical, and lifestyle history.
Physical Examination: Measure baseline weight, height, BMI, and vital signs.
Nursing Interventions: Identify high-risk factors (e.g., diabetes, hypertension) and provide emotional support.
2. Regular Prenatal Visits
Frequency: Monthly (up to 28 weeks), biweekly (28-36 weeks), and weekly (36 weeks to delivery).
Routine Checkups: Includes weight, blood pressure, fetal heart rate (FHR), and fundal height.
Nursing Interventions: Encourage adherence to appointments and educate on warning signs (e.g., bleeding, severe headaches, preterm labor).
3. Health Promotion and Education
Lifestyle Changes: Stop smoking, avoid alcohol, and reduce stress.
Nutrition and Supplements: Emphasize the importance of folic acid, iron, and calcium in the diet.
Physical Activity: Recommend light exercises such as walking or yoga to promote circulation and reduce edema.
4. Fetal Well-Being Monitoring
Fetal Movement Counting: Instruct the mother to monitor fetal movements (kick counts) starting at 28 weeks.
Fetal Heart Monitoring: FHR is checked during visits using a Doppler to ensure well-being.
2. Physiological Changes During Pregnancy
During pregnancy, the mother’s body undergoes numerous physiological changes to support fetal development. These changes affect major body systems, and nurses must recognize normal adaptations versus signs of complications.
Key Physiological Changes During Pregnancy :
1. Cardiovascular Changes
Increased Blood Volume: Blood volume increases by 30-50% to support fetal oxygenation.
Increased Heart Rate and Cardiac Output: The heart works harder to meet oxygen demands.
Nursing Interventions: Monitor for hypertension (risk for preeclampsia) and ensure the mother rests on her left side to prevent vena cava compression.
2. Respiratory Changes
Diaphragm Displacement: The uterus presses on the diaphragm, reducing lung expansion.
Increased Oxygen Demand: Oxygen consumption increases by 15-20%.
Nursing Interventions: Encourage deep breathing and teach patients how to position themselves to improve lung expansion.
3. Endocrine Changes
Hormonal Shifts: Estrogen, progesterone, and hCG rise, impacting metabolism and mood.
Increased Risk of Gestational Diabetes: Due to insulin resistance.
Nursing Interventions: Teach the patient about signs of hyperglycemia and the need for glucose tolerance testing.
4. Musculoskeletal Changes
Postural Changes: The mother's center of gravity shifts, causing lordosis (spinal curvature).
Joint Relaxation: Due to the release of relaxin, which softens joints and ligaments.
Nursing Interventions: Teach proper posture, use of maternity support belts, and safe exercise routines.
5. Gastrointestinal Changes
Nausea and Vomiting: Occurs due to hormonal changes (common during the first trimester).
Constipation and Heartburn: Slowed GI motility and relaxation of the esophageal sphincter cause acid reflux.
Nursing Interventions: Advise small, frequent meals, hydration, and consumption of a high-fiber diet.
3. Common Complications of Pregnancy
Pregnancy complications can arise at any point in the antepartum period. Early detection and timely nursing interventions are essential to ensure maternal and fetal well-being.
1. Gestational Diabetes Mellitus (GDM)
Cause: Placental hormones interfere with insulin production, leading to high blood sugar.
Symptoms: Excessive thirst, frequent urination, and a large fetus (macrosomia).
Nursing Interventions:
Teach blood sugar monitoring and encourage dietary changes.
Schedule regular glucose tolerance tests.
2. Preeclampsia/Eclampsia
Cause: Abnormal placental development, leading to high blood pressure.
Symptoms: High BP, proteinuria, blurred vision, and severe headaches.
Nursing Interventions:
Monitor BP and urine protein regularly.
Teach mothers to report headaches, swelling, or blurred vision immediately.
Administer magnesium sulfate to prevent seizures.
3. Placenta Previa
Cause: Placenta implants in the lower uterine segment, covering the cervix.
Symptoms: Painless vaginal bleeding in the second or third trimester.
Nursing Interventions:
Instruct mothers to avoid vaginal exams.
Monitor for signs of hemorrhage and prepare for possible C-section delivery.
4. Hyperemesis Gravidarum
Cause: Excessive vomiting due to severe hormonal shifts.
Symptoms: Severe dehydration, weight loss, and electrolyte imbalances.
Nursing Interventions:
Provide IV fluid replacement.
Recommend small, frequent meals and prescribe antiemetics.
5. Preterm Labor
Cause: Uterine infections, trauma, or multiple pregnancies.
Symptoms: Regular contractions before 37 weeks, lower back pain, and discharge.
Nursing Interventions:
Administer tocolytics to stop labor.
Encourage hydration and activity restriction.
Educate on signs of preterm labor (contractions, leakage of amniotic fluid).
4. Diagnostic Tests During Pregnancy
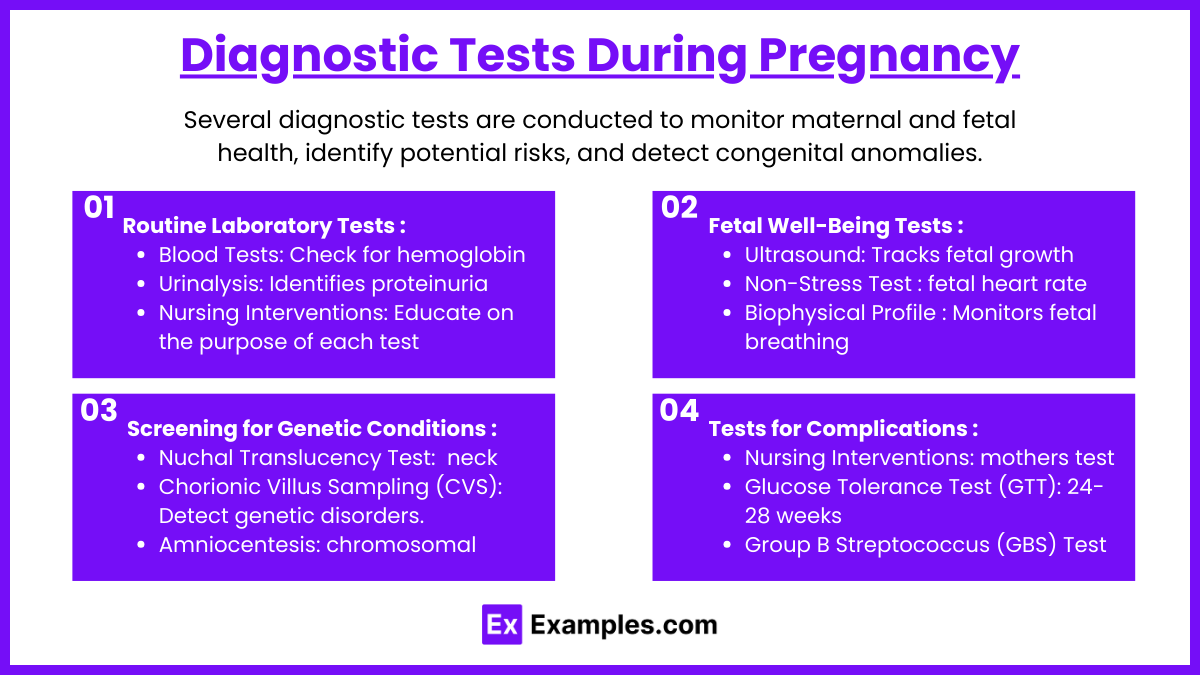
Several diagnostic tests are conducted to monitor maternal and fetal health, identify potential risks, and detect congenital anomalies.
1. Routine Laboratory Tests
Blood Tests: Check for hemoglobin, hematocrit, blood type, Rh factor, and STI screenings.
Urinalysis: Identifies proteinuria, glucose, and infection.
Nursing Interventions: Educate on the purpose of each test and ensure timely follow-ups.
2. Fetal Well-Being Tests
Ultrasound: Tracks fetal growth, identifies abnormalities, and assesses amniotic fluid.
Non-Stress Test (NST): Measures fetal heart rate during fetal movement.
Biophysical Profile (BPP): Monitors fetal breathing, movement, and amniotic fluid.
Nursing Interventions: Ensure the mother is hydrated before tests, as this helps visualize the fetus on ultrasounds.
3. Screening for Genetic Conditions
Nuchal Translucency Test: Measures fluid at the back of the fetus’s neck (linked to Down syndrome risk).
Chorionic Villus Sampling (CVS): Performed at 10-12 weeks to detect genetic disorders.
Amniocentesis: Withdraws amniotic fluid to test for chromosomal abnormalities.
Nursing Interventions: Support the patient through the process and monitor for complications (bleeding, cramping) post-test.
4. Tests for Complications
Nursing Interventions: Encourage mothers to undergo necessary tests and explain the significance of each test.
Glucose Tolerance Test (GTT): Performed at 24-28 weeks to screen for gestational diabetes.
Group B Streptococcus (GBS) Test: Performed at 36-37 weeks to detect GBS bacteria.
Examples
Example 1: Regular Prenatal Checkups
During the antepartum period, pregnant women attend regular prenatal checkups where nurses and healthcare providers monitor vital signs, measure fundal height, and assess fetal heart rate. These visits aim to detect complications like gestational diabetes or preeclampsia early to ensure maternal and fetal well-being.
Example 2: Fetal Ultrasound Scans
Ultrasound scans are essential during the antepartum period to monitor fetal development, detect congenital abnormalities, and assess the position of the placenta. This diagnostic test provides valuable information on fetal growth and identifies potential complications like placenta previa.
Example 3: Screening for Gestational Diabetes
Pregnant women undergo glucose tolerance testing between 24 and 28 weeks to check for gestational diabetes. Early detection allows for timely interventions, such as dietary changes and blood sugar monitoring, to prevent complications for both mother and baby.
Example 4: Nutritional Counseling
Nutritional guidance is an integral part of antepartum care. Pregnant women receive dietary advice, including the importance of folic acid, iron, and calcium intake, to support fetal growth and prevent birth defects. Nurses educate mothers about healthy food choices and the risks of nutrient deficiencies.
Example 5: Monitoring for Preterm Labor
Nurses educate pregnant women on recognizing early signs of preterm labor, such as cramping, backache, and contractions before 37 weeks. Early identification allows healthcare providers to administer tocolytic medications to stop labor, thereby promoting a full-term pregnancy and reducing neonatal complications.
Practice Questions
Question 1
A nurse is assessing a pregnant client during her 28-week prenatal visit. Which of the following findings should the nurse report to the healthcare provider as an abnormal sign?
A) Blood pressure of 150/95 mmHg
B) Fundal height measuring 28 cm
C) Fetal heart rate of 140 beats per minute
D) Report of occasional leg cramps
Answer: A) Blood pressure of 150/95 mmHg
Explanation: A is Correct: A blood pressure reading of 150/95 mmHg is a red flag, as it indicates potential preeclampsia, a pregnancy complication characterized by high blood pressure, proteinuria, and potential organ damage. The nurse should notify the healthcare provider immediately.
Why B is Incorrect: At 28 weeks, the fundal height should be approximately equal to the number of weeks of gestation (±2 cm). Therefore, a fundal height of 28 cm at 28 weeks is normal.
Why C is Incorrect: The normal range for fetal heart rate (FHR) is 110-160 beats per minute, and 140 bpm is well within this range.
Why D is Incorrect: Occasional leg cramps are common in pregnancy due to pressure on nerves and electrolyte imbalances. Proper hydration, stretching, and increasing magnesium intake can relieve leg cramps.
Question 2
A nurse is educating a pregnant client in her first trimester about early pregnancy changes. Which of the following statements indicates that the client requires further teaching?
A) "I may experience nausea and vomiting, especially in the morning."
B) "I should expect to gain about 25-35 pounds throughout the pregnancy."
C) "It’s normal to feel sudden, sharp abdominal pain during the first trimester."
D) "I should take folic acid supplements to reduce the risk of birth defects."
Answer: C) "It’s normal to feel sudden, sharp abdominal pain during the first trimester."
Explanation: C is Correct: Sudden, sharp abdominal pain in the first trimester could be a sign of a serious problem like ectopic pregnancy or miscarriage, and it should be reported immediately. Cramping or mild discomfort is normal, but severe, sharp pain is not.
Why A is Incorrect: Nausea and vomiting (morning sickness) are normal due to increased levels of hCG (human chorionic gonadotropin) during the first trimester.
Why B is Incorrect: Pregnant women are expected to gain 25-35 pounds throughout the pregnancy, depending on their pre-pregnancy BMI.
Why D is Incorrect: Taking folic acid supplements reduces the risk of neural tube defects like spina bifida, making this an essential component of prenatal care.
Question 3
A nurse is teaching a group of pregnant women about the importance of diagnostic testing during pregnancy. Which of the following diagnostic tests is typically performed at 24 to 28 weeks of gestation to screen for gestational diabetes?
A) Group B Streptococcus (GBS) screening
B) Glucose tolerance test (GTT)
C) Amniocentesis
D) Nuchal translucency test
Answer: B) Glucose tolerance test (GTT)
Explanation: B is Correct: The glucose tolerance test (GTT) is done between 24 to 28 weeks of gestation to screen for gestational diabetes mellitus (GDM). It involves drinking a sugary drink followed by blood glucose testing to assess how the body processes glucose.
Why A is Incorrect: Group B Streptococcus (GBS) screening is done at 35-37 weeks, not 24-28 weeks, to detect GBS bacteria and prevent neonatal infection during childbirth.
Why C is Incorrect: Amniocentesis is usually done at 15-20 weeks to check for chromosomal abnormalities, genetic disorders, or neural tube defects. It is not performed at 24-28 weeks.
Why D is Incorrect: The nuchal translucency test is a screening done in the first trimester (11-14 weeks) to detect chromosomal abnormalities such as Down syndrome. It is not a test for gestational diabetes.