Assignment and delegation are fundamental components of leadership and management in nursing. These processes ensure the efficient allocation of tasks, promote teamwork, and support safe, high-quality patient care. While assignment involves allocating routine tasks to qualified personnel, delegation requires the transfer of authority for specific tasks while maintaining accountability. For the NCLEX-PN® exam, understanding the principles of assignment and delegation, including the Five Rights of Delegation, is essential for answering scenario-based questions that assess prioritization, responsibility, and patient safety.
Learning Objectives
In studying “Leadership & Management: Assignment/Delegation” for the NCLEX-PN® Exam, you should learn to understand the principles of assignment and delegation, focusing on the Five Rights of Delegation. Analyze the roles and responsibilities of RNs, LPNs, and UAPs in task delegation. Evaluate factors affecting delegation, such as patient condition, task complexity, and team member competence. Explore nursing considerations like accountability, supervision, and prioritization of care. Apply knowledge to ensure safe delegation, effective communication, and proper supervision to maintain patient safety and care quality.
1. Understanding the Concept of Assignment and Delegation
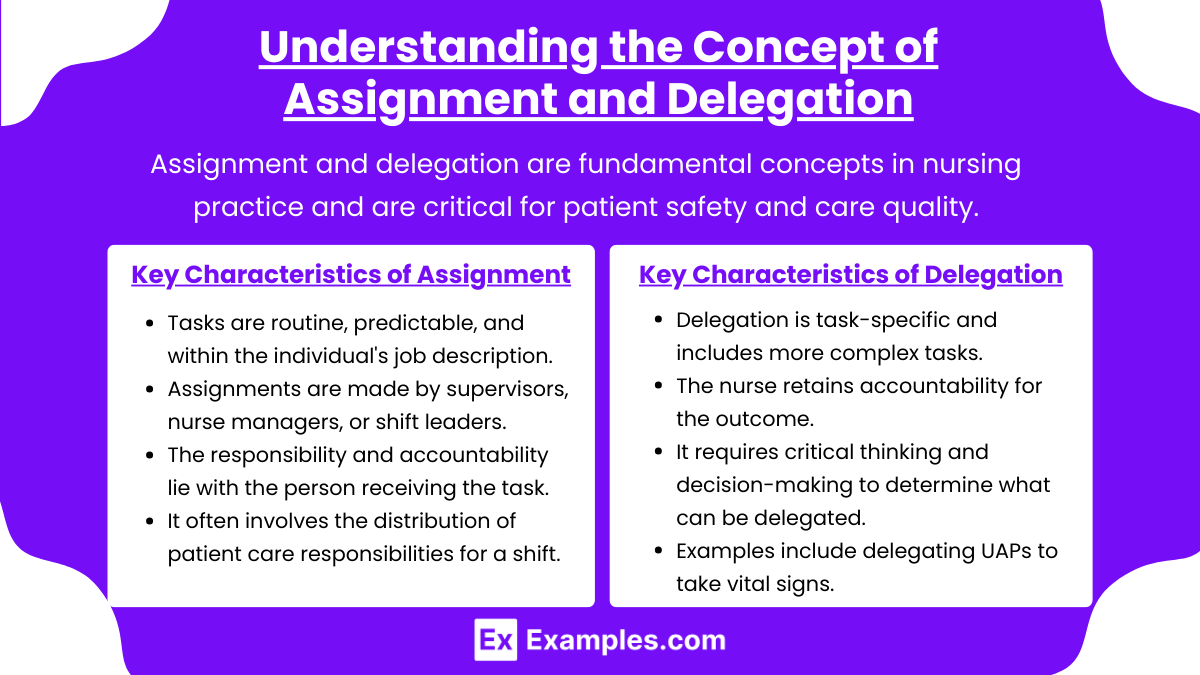
Assignment and delegation are fundamental concepts in nursing practice and are critical for patient safety and care quality. For the NCLEX-PN®, understanding the differences between these two concepts is essential for making sound decisions on task allocation.
- Assignment refers to the process of distributing work or specific tasks to qualified team members. Assignments are direct instructions given to individuals (like LPNs, RNs, or UAPs) regarding the specific duties they need to complete. For example, a nurse manager may assign a UAP to collect vital signs on specific patients.
- Delegation, on the other hand, occurs when a nurse transfers the authority to perform a task to another competent individual. While the task is performed by the delegate (like an LPN or UAP), the nurse remains responsible for ensuring the task is completed properly. Delegation requires clear instructions and follow-up.
Key Characteristics of Assignment
- Tasks are routine, predictable, and within the individual’s job description.
- Assignments are made by supervisors, nurse managers, or shift leaders.
- The responsibility and accountability lie with the person receiving the task.
- It often involves the distribution of patient care responsibilities for a shift (e.g., “LPN A will care for patients 1, 2, and 3”).
Key Characteristics of Delegation
- Delegation is task-specific and includes more complex tasks.
- The nurse retains accountability for the outcome.
- It requires critical thinking and decision-making to determine what can be delegated.
- Examples include delegating UAPs to take vital signs or assist with ADLs.
2. Differences Between Assignment and Delegation
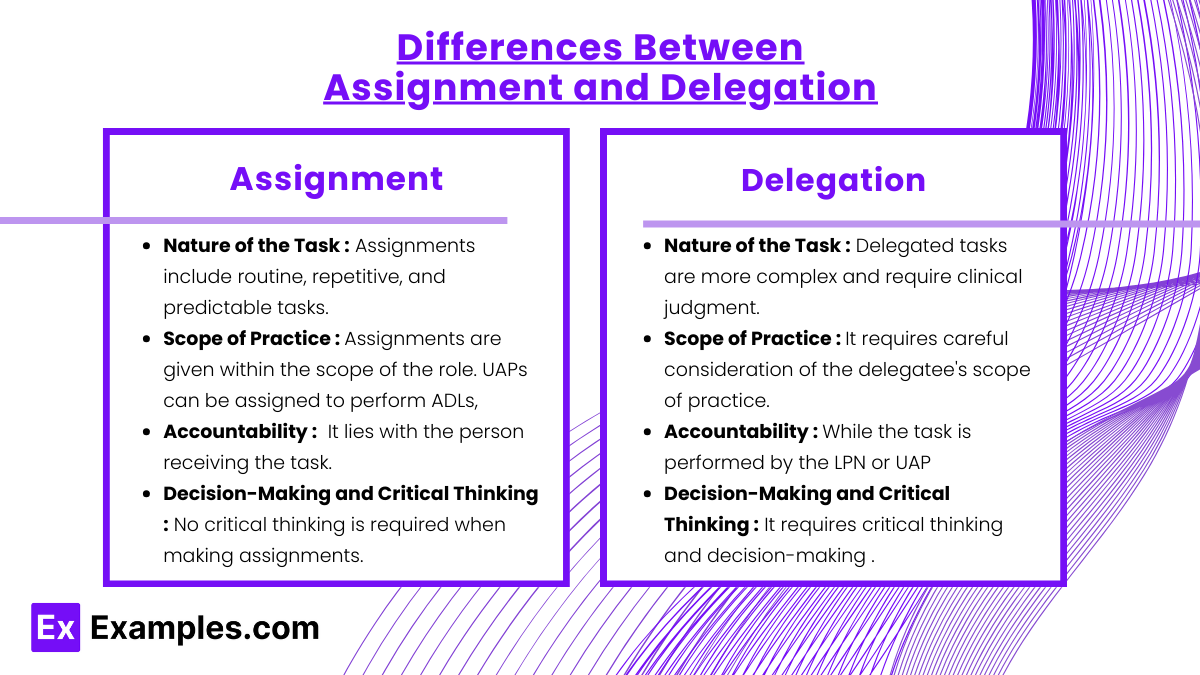
While assignment and delegation are both ways to distribute tasks, their differences lie in responsibility, accountability, and the complexity of the task. Here’s a breakdown of how they differ:
1. Nature of the Task
- Assignment: Assignments include routine, repetitive, and predictable tasks that do not require nursing judgment. Tasks like collecting vital signs, assisting with ADLs (bathing, feeding, etc.), and cleaning a patient’s room can be assigned to a UAP or LPN.
- Delegation: Delegated tasks are more complex and require clinical judgment. Delegation typically involves tasks like blood glucose monitoring, documenting input and output, and administering certain medications (if within the LPN’s scope).
2. Scope of Practice
- Assignment: Assignments are given within the scope of the role. For example, UAPs can be assigned to perform ADLs, but they cannot be assigned to administer medications or perform patient education.
- Delegation: Delegation requires careful consideration of the delegatee’s scope of practice and competence. LPNs can be delegated to change dressings or monitor glucose levels, but they cannot be delegated tasks like initial assessments, IV medication administration, or care planning, as those are reserved for RNs.
3. Accountability
- Assignment: Accountability lies with the person receiving the task. If a UAP is assigned to take vital signs, the UAP is responsible for completing the task correctly.
- Delegation: While the task is performed by the LPN or UAP, the nurse retains full accountability. This means the LPN or RN who delegates the task is still responsible for ensuring that it is completed correctly and safely.
4. Decision-Making and Critical Thinking
- Assignment: No critical thinking is required when making assignments. Assignments are based on workload distribution. For example, assigning a UAP to feed Patient A and bathe Patient B requires no critical thinking.
- Delegation: Delegation requires critical thinking and decision-making to identify which tasks can be safely delegated based on the patient’s condition, the delegatee’s skills, and the nature of the task. The nurse must ensure that the UAP or LPN understands the task and the expected outcome.
3. Principles of Assignment and Delegation
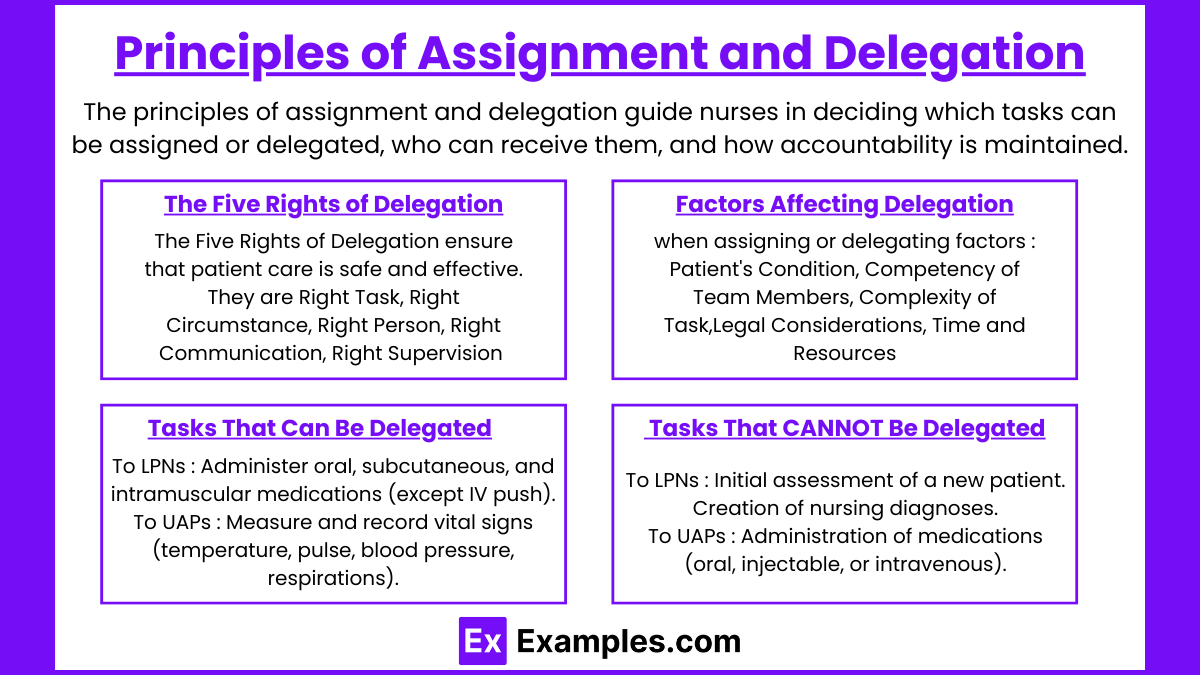
The principles of assignment and delegation guide nurses in deciding which tasks can be assigned or delegated, who can receive them, and how accountability is maintained. For NCLEX-PN® questions, it’s essential to know the following core principles.
1. The Five Rights of Delegation
The Five Rights of Delegation ensure that patient care is safe and effective. They are:
- Right Task: The task must be appropriate for delegation. Routine, repetitive, and predictable tasks are suitable for delegation (e.g., taking vital signs, assisting with ADLs).
- Right Circumstance: The patient’s condition must be stable, and the work environment must support task completion. A UAP cannot be assigned to take vitals on an unstable patient.
- Right Person: The person assigned to the task must be competent and within their scope of practice. Tasks assigned to a UAP differ from those assigned to an LPN.
- Right Communication/Direction: The nurse must provide clear, specific instructions on what needs to be done, how to do it, and when to report back.
- Right Supervision/Evaluation: The nurse must monitor task progress and provide guidance when needed. After completion, the nurse must evaluate the quality of work.
2. Factors Affecting Delegation and Assignment
When assigning or delegating, consider the following factors:
- Patient’s Condition: Unstable or critical patients should only be handled by licensed nurses (RN or LPN), not UAPs.
- Competency of Team Members: Evaluate the delegatee’s skills, knowledge, and abilities before delegating.
- Complexity of Task: Simple tasks like bathing or feeding can be assigned to UAPs, but complex tasks like administering medications must be performed by LPNs or RNs.
- Legal Considerations: Delegation must comply with state Nurse Practice Acts, which define the scope of practice for LPNs and UAPs.
- Time and Resources: Consider if there is enough time to supervise, monitor, and evaluate the performance of the delegate.
3. Tasks That Can Be Delegated
- To LPNs:
- Administer oral, subcutaneous, and intramuscular medications (except IV push).
- Perform wound care, dressing changes, and catheterizations.
- Reinforce patient education after initial teaching by an RN.
- Monitor and report changes in patient conditions.
- Administer enteral feedings (depending on facility policy).
- To UAPs:
- Measure and record vital signs (temperature, pulse, blood pressure, respirations).
- Assist with Activities of Daily Living (ADLs) such as bathing, feeding, and toileting.
- Reposition and transfer patients.
- Clean and maintain patient areas (change linens, empty catheter bags).
4. Tasks That CANNOT Be Delegated
- To LPNs:
- Initial assessment of a new patient.
- Creation of nursing diagnoses.
- IV push medications or blood transfusions.
- Development or modification of the care plan.
- To UAPs:
- Initial patient assessment or evaluation.
- Administration of medications (oral, injectable, or intravenous).
- Patient education (initial education must be done by an RN).
- Wound care requiring sterile technique.
Examples
Example 1: Assigning a UAP to Measure Vital Signs for a Group of Stable Patients
The nurse assigns the Unlicensed Assistive Personnel (UAP) to take and document the vital signs (blood pressure, temperature, heart rate, and respiratory rate) of stable patients on the unit. Since vital signs are a routine, repetitive task that does not require clinical judgment, it qualifies as an assignment. The UAP is responsible for completing the task correctly, but the nurse maintains the responsibility for reviewing the documented results to identify any abnormalities.
Example 2: Delegating an LPN to Perform Wound Care for a Patient with a Pressure Ulcer
A nurse delegates a Licensed Practical Nurse (LPN) to perform wound care, including cleaning, dressing, and applying topical medications to a patient with a stage 2 pressure ulcer. Since wound care requires technical skills and nursing judgment (for example, noticing signs of infection), this task is delegated rather than assigned. The nurse is still accountable for ensuring that the task is completed properly, and the LPN is responsible for carrying out the task according to facility policies and procedures.
Example 3: Assigning a UAP to Assist a Patient with Bathing and Personal Hygiene
The nurse assigns a UAP to assist a patient with bathing, oral hygiene, and grooming. This task does not require nursing judgment, critical thinking, or decision-making, so it is an assignment. The UAP is responsible for ensuring the patient’s hygiene is completed appropriately. The nurse does not need to supervise the task actively but should confirm that the patient’s hygiene needs were met during follow-up care.
Example 4: Delegating an LPN to Administer Oral Medications to a Group of Patients
A nurse delegates an LPN to administer oral medications to a group of patients. Since medication administration requires a level of nursing judgment (confirming the “Five Rights” of medication administration), this is considered delegation, not an assignment. The nurse retains accountability for the overall medication administration process, but the LPN is responsible for administering the medication safely and reporting any issues (like side effects or refusals) to the nurse.
Example 5: Assigning a UAP to Transport a Patient from the Room to the Radiology Department
The nurse assigns a UAP to transport a stable patient to the radiology department for an x-ray. This task is routine, non-complex, and requires no nursing judgment, so it qualifies as an assignment. The nurse does not need to provide ongoing supervision, and the UAP is responsible for ensuring the safe transport of the patient. The nurse, however, is still responsible for verifying that the task was completed and the patient returned safely to the unit.
Practice Questions
Question 1
The LPN is caring for a group of patients. Which task is most appropriate for the LPN to delegate to a UAP?
A) Administer subcutaneous insulin to a diabetic patient.
B) Measure and record the intake and output for a postoperative patient.
C) Teach a patient with asthma how to use a metered-dose inhaler.
D) Monitor for changes in a patient’s neurological status.
Answer: B) Measure and record the intake and output for a postoperative patient.
Explanation: Option B: Correct — Measuring and recording intake and output (I&O) is a routine, non-complex task that is within the scope of a UAP’s role. It does not require nursing judgment or assessment.
- Option A: Incorrect — UAPs cannot administer medications, including subcutaneous injections. This task must be performed by an LPN or RN.
- Option C: Incorrect — Teaching a patient requires critical thinking, assessment, and evaluation, which is within the scope of an RN, not a UAP or LPN.
- Option D: Incorrect — Monitoring for changes in a patient’s neurological status requires critical thinking, ongoing assessment, and evaluation. This task is the responsibility of a licensed nurse (LPN or RN).
Question 2
The LPN is working with a UAP on a medical-surgical floor. Which of the following tasks should the LPN NOT delegate to the UAP?
A) Repositioning a patient every two hours to prevent pressure ulcers.
B) Feeding a patient with stable dysphagia who requires aspiration precautions.
C) Performing a sterile dressing change on a patient’s abdominal surgical wound.
D) Assisting a patient with ambulation using a walker after a total knee replacement.
Answer: C) Performing a sterile dressing change on a patient’s abdominal surgical wound.
Explanation: Option C: Correct — A sterile dressing change requires sterile technique, clinical judgment, and the ability to recognize signs of infection or complications. This task is beyond the scope of a UAP and should be performed by an LPN or RN.
- Option A: Incorrect — Repositioning a patient is a basic activity of daily living (ADL) that can be safely assigned to a UAP.
- Option B: Incorrect — Feeding a patient with stable dysphagia can be assigned to a UAP as long as aspiration precautions are clearly communicated. However, initial feeding following a new diagnosis of dysphagia requires assessment and monitoring by an LPN or RN.
- Option D: Incorrect — Assisting with ambulation is a basic task that does not require clinical judgment. It can be assigned to a UAP as long as proper instructions are provided.
Question 3
The LPN on a medical-surgical unit is caring for four patients. Which task should the LPN complete first based on priority?
A) Administer oral pain medication to a patient who rates their pain 6/10.
B) Delegate the UAP to take vital signs for a patient scheduled for discharge.
C) Respond to a patient who is short of breath and has oxygen saturation of 88%.
D) Perform a dressing change on a stable postoperative patient.
Answer: C) Respond to a patient who is short of breath and has oxygen saturation of 88%.
Explanation: This question requires you to prioritize tasks using the ABC (Airway, Breathing, Circulation) framework. Option C: Correct — Shortness of breath and an oxygen saturation of 88% is a breathing issue, which requires immediate attention. According to the ABC prioritization rule, breathing-related problems take precedence. Immediate intervention is required to prevent further oxygen deprivation. Let’s analyze each option:
- Option A: Incorrect — Administering pain medication is important, but pain is not life-threatening. Breathing takes priority over pain.
- Option B: Incorrect — Delegating vital signs to a UAP is not urgent. It can be done after the LPN addresses more critical patient needs.
- Option D: Incorrect — A dressing change is routine and does not address a life-threatening issue. This task can be delayed.