Preparing for the NCLEX PN® Exam requires a thorough understanding of Basic Care & Comfort in Fundamentals, a key component of nursing practice. Mastery of skills such as nutrition, hydration, hygiene, mobility, and comfort measures is essential. This knowledge supports effective patient care, promoting recovery, comfort, and overall well-being.
Learning Objective
In studying “Basic Care & Comfort in Fundamentals” for the NCLEX PN® Exam, you should aim to understand and apply the fundamental principles of patient care that ensure comfort and facilitate recovery. Learn to assess and manage patients’ needs related to personal hygiene, nutrition, mobility, and sleep. Evaluate different pain management techniques and the use of assistive devices in promoting patient independence and comfort. Additionally, explore the psychological aspects of care, including patient education and emotional support. Apply this knowledge to develop comprehensive nursing care plans that address both the physical and emotional needs of patients, improving their overall well-being and recovery process.
Fundamentals of Nursing Care
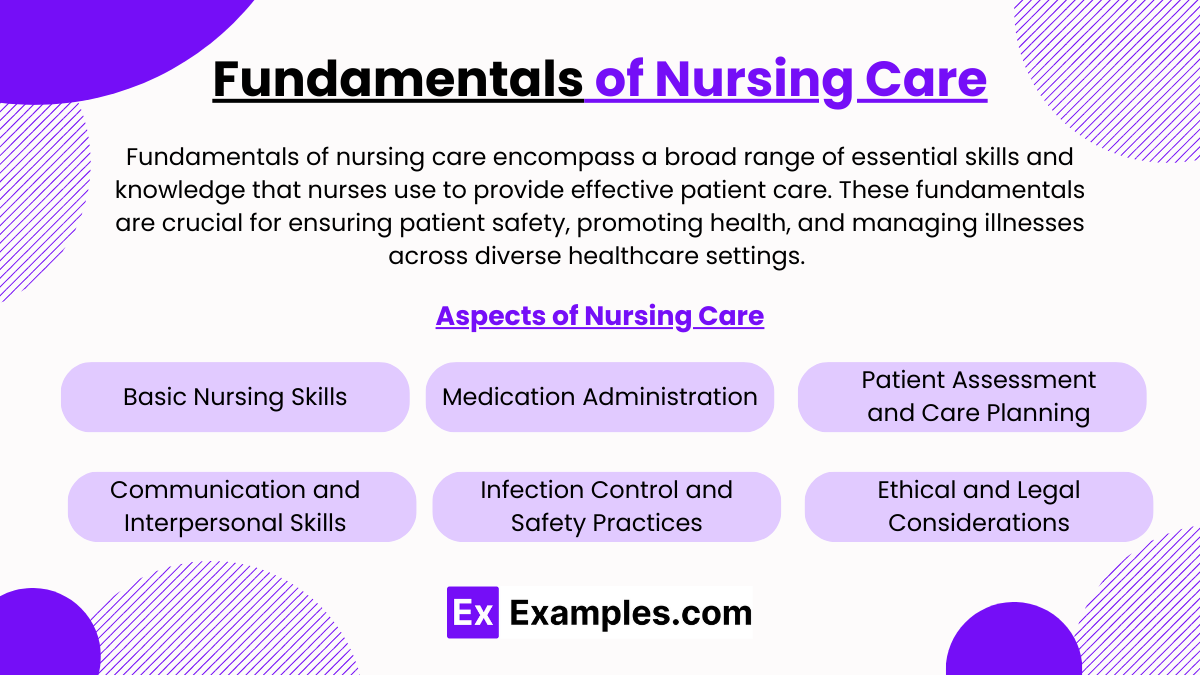
Fundamentals of nursing care encompass a broad range of essential skills and knowledge that nurses use to provide effective patient care. These fundamentals are crucial for ensuring patient safety, promoting health, and managing illnesses across diverse healthcare settings. Here’s an overview of the core aspects of nursing care:
1. Basic Nursing Skills
- Vital Signs Monitoring: Assessing temperature, pulse, respiration, blood pressure, and often oxygen saturation to monitor a patient’s clinical status.
- Hygiene Care: Assisting patients with daily activities such as bathing, oral care, grooming, and dressing, which are essential for comfort and preventing infection.
- Nutrition and Hydration: Managing dietary needs, including feeding patients or setting up nutritional plans with dietitians, ensuring proper hydration and nutrition.
- Mobility Assistance: Helping patients move, turn in bed, and ambulate as needed to maintain physical function and prevent complications like pressure ulcers or deep vein thrombosis.
2. Medication Administration
- Accuracy and Safety: Ensuring correct dosages, medication reconciliation, and monitoring for adverse reactions.
- Routes of Administration: Managing oral, topical, intravenous, and other routes of medication administration.
- Patient Education: Teaching patients about their medications, including how to take them, possible side effects, and interactions.
3. Patient Assessment and Care Planning
- Initial and Ongoing Assessment: Conducting comprehensive assessments of physical, emotional, and social needs.
- Developing Care Plans: Creating individualized care plans based on assessment data, including short-term and long-term goals.
- Documentation: Accurate and detailed recording of patient data, interventions, and outcomes.
4. Communication and Interpersonal Skills
- Patient Interactions: Establishing rapport and trust with patients and their families.
- Interdisciplinary Team Coordination: Collaborating with other healthcare professionals to provide coordinated and comprehensive care.
- Patient and Family Education: Teaching about health conditions, treatment plans, and preventive health practices.
5. Infection Control and Safety Practices
- Hand Hygiene: Regular and thorough handwashing to prevent the spread of infection.
- Use of Personal Protective Equipment (PPE): Proper use of gloves, gowns, masks, and other protective items.
- Aseptic Techniques: Using methods to reduce the risk of infection, particularly in procedures such as wound care or catheter insertion.
6. Ethical and Legal Considerations
- Confidentiality: Maintaining patient privacy and confidentiality in line with legal requirements.
- Consent: Ensuring informed consent is obtained before performing procedures or treatments.
- Ethical Decision Making: Navigating complex ethical issues in patient care, such as end-of-life decisions or conflicts over treatment choices.
Comfort Measures
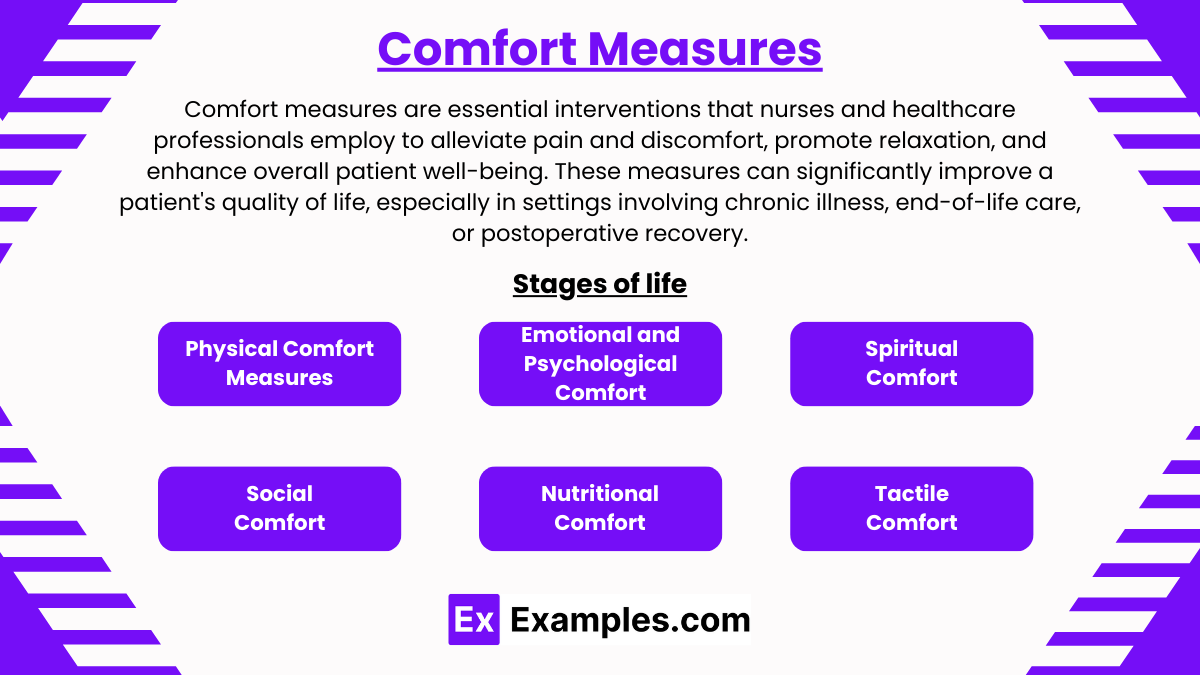
Comfort measures are essential interventions that nurses and healthcare professionals employ to alleviate pain and discomfort, promote relaxation, and enhance overall patient well-being. These measures can significantly improve a patient’s quality of life, especially in settings involving chronic illness, end-of-life care, or postoperative recovery. Here’s an overview of various types of comfort measures commonly used in healthcare:
1. Physical Comfort Measures
- Pain Management: Administering pain medications as prescribed and using non-pharmacological methods such as heat or cold therapy, massage, and relaxation techniques.
- Positioning: Adjusting the patient’s position regularly to prevent pressure ulcers and enhance comfort. Special pillows and supports can help relieve pressure and align the body properly.
- Environment: Adjusting lighting, temperature, and noise levels in the patient’s room to create a soothing environment. Personal items from home can also make a space feel more comforting and familiar.
2. Emotional and Psychological Comfort
- Active Listening and Empathy: Offering a compassionate presence, listening actively to patients’ concerns, and validating their feelings.
- Providing Information and Reassurance: Keeping patients informed about their care and progress can alleviate anxiety. Reassuring patients about what to expect during treatments or procedures can also help reduce fear and anxiety.
- Distraction Techniques: Engaging patients in activities such as reading, music, movies, or simple conversation to divert their attention from pain or discomfort.
3. Spiritual Comfort
- Spiritual Care: Respecting and supporting the patient’s spiritual beliefs and needs. This might involve arranging visits from spiritual care providers, facilitating prayer or meditation, or providing resources like religious texts.
- Existential Support: Helping patients find meaning and peace in their experiences, especially during critical illness or near the end of life.
4. Social Comfort
- Family Involvement: Encouraging visits from family and friends to maintain social connections and provide emotional support. Facilitating virtual communication if in-person visits are not possible.
- Support Groups and Community Resources: Connecting patients with support groups where they can share experiences and receive support from others with similar conditions.
5. Nutritional Comfort
- Dietary Adjustments: Providing meals that are not only nutritionally balanced but also cater to patients’ tastes and dietary preferences. Managing symptoms like nausea or dry mouth with appropriate food choices and hydration strategies.
- Pleasant Meal Environment: Creating a pleasant dining environment can help improve appetite and enjoyment of food, such as providing a well-set table or companionship during meals.
6. Tactile Comfort
- Therapeutic Touch and Massage: Utilizing gentle touch and massage to reduce stress, ease pain, and provide a sense of connection and comfort.
- Personal Care and Grooming: Assisting with grooming and hygiene to help patients feel refreshed and dignified.
Safety and Infection Control

Safety and infection control are critical components of healthcare that protect both patients and healthcare workers from injury and illness. These practices are designed to minimize the risk of infection, prevent accidents, and ensure a safe environment. Here’s an overview of the key elements of safety and infection control in a healthcare setting:
1. Hand Hygiene
- Fundamental Practice: Regular and thorough hand washing with soap and water, or using an alcohol-based hand sanitizer, is the most effective way to prevent the spread of infections.
- Guidelines: Healthcare providers must perform hand hygiene before and after every patient contact, after touching potentially contaminated surfaces, and before performing sterile procedures.
2. Use of Personal Protective Equipment (PPE)
- Components: PPE includes gloves, gowns, masks, face shields, and eye protection.
- Application: Proper use of PPE depends on the risk of exposure and the type of patient interaction. PPE must be donned and doffed correctly to prevent contamination.
3. Safe Injection Practices
- Single-Use Policy: Needles and syringes are used for one patient only and then disposed of safely.
- Medication Preparation: Aseptic technique must be used when preparing and administering medications to prevent contamination.
4. Environmental Cleaning and Disinfection
- Regular Cleaning: Surfaces and medical equipment in patient rooms and treatment areas must be cleaned and disinfected regularly using appropriate cleaning agents.
- Spill Management: Bodily fluids and blood spills must be promptly and safely cleaned according to established protocols.
5. Sterilization of Instruments
- Critical Tools: Instruments used in surgery and other invasive procedures must be properly sterilized to eliminate all microorganisms.
- Monitoring: Sterilization processes are regularly monitored with biological indicators to ensure effectiveness.
6. Respiratory Hygiene/Cough Etiquette
- Implementation: Patients with signs of respiratory infection are instructed to cover their mouths/noses when coughing or sneezing and to use and dispose of tissues.
- Masks and Separation: Patients showing respiratory symptoms should wear a surgical mask and be separated from others in common areas.
7. Safe Handling of Sharps
- Disposal: All sharps (needles, scalpels, etc.) must be immediately disposed of in designated sharps containers.
- No Recapping: Needles should not be recapped to avoid needlestick injuries.
8. Patient Safety Practices
- Identification: Correct patient identification must be verified before administering medications, collecting samples, or performing treatments.
- Fall Prevention: Implement strategies to reduce falls, including non-slip footwear, adequate lighting, and necessary adjustments in patient rooms.
9. Education and Training
- Continuous Training: Healthcare workers receive ongoing training in the latest safety and infection control practices.
- Awareness Campaigns: Regular updates and reminders about infection control protocols are provided to staff.
10. Surveillance and Reporting
- Infection Tracking: Infections acquired within the facility are tracked and investigated to determine the source and prevent recurrence.
- Improvement Strategies: Data collected is used to improve safety protocols and infection control measures.
Examples
Example 1: Hygiene Care for an Immobilized Patient
- A nurse assists an immobilized patient with daily bathing and skin care routines to prevent skin breakdown and infection. The nurse uses gentle cleansing, moisturizes dry areas, and inspects the skin for pressure ulcers, implementing necessary changes in position and bedding to enhance comfort and skin integrity.
Example 2: Nutritional Support for a Patient with Dysphagia
- A patient recovering from a stroke exhibits signs of dysphagia. The nurse collaborates with a dietitian to provide meals that are easy to swallow and meet the patient’s nutritional requirements. The nurse also monitors the patient during meals to prevent choking and ensure adequate intake.
Example 3: Mobility Training with Assistive Devices
- A nurse trains a patient recovering from hip replacement surgery on how to use a walker. The nurse demonstrates proper techniques to ensure safety and encourage mobility, setting gradual goals to increase the patient’s confidence and independence.
Example 4: Pain Management for a Postoperative Patient
- Following abdominal surgery, a patient reports significant pain. The nurse administers prescribed analgesics and employs non-pharmacological methods such as guided imagery and relaxation breathing to enhance the patient’s comfort and facilitate recovery.
Example 5: Teaching a Diabetic Patient About Foot Care
- A nurse educates a diabetic patient on the importance of daily foot inspections to prevent complications like ulcers or infections. The nurse demonstrates how to properly inspect the feet, identifies appropriate footwear, and discusses signs of potential problems that should prompt immediate medical attention.
Practice Questions
Question 1
Which intervention is most effective for preventing pressure ulcers in a bedridden patient?
A. Reposition the patient every two hours
B. Apply a high-potency topical steroid
C. Increase fluid intake to hydrate the skin
D. Use a low-density foam mattress
Answer:
A. Reposition the patient every two hours
Explanation:
Repositioning the patient every two hours is a critical intervention for preventing pressure ulcers, as it helps distribute pressure and enhances blood flow to tissues that might otherwise be compressed by continuous pressure. While increasing fluid intake (option C) is beneficial for overall skin health, it does not directly prevent pressure ulcers. High-potency topical steroids (option B) are not indicated for prevention and may cause skin thinning. Using specialized mattresses (option D) can help, but regular repositioning is universally recognized as a key preventive measure.
Question 2
What is the primary purpose of providing oral care to unconscious patients?
A. To enhance their sense of taste
B. To prevent pneumonia
C. To avoid disturbing the patient
D. To prepare them for meal times
Answer:
B. To prevent pneumonia
Explanation:
Oral care in unconscious patients is crucial for preventing pneumonia, particularly aspiration pneumonia. It helps keep the mouth clean, reduces the bacterial load, and prevents the aspiration of harmful pathogens into the lungs. This intervention is essential as unconscious patients cannot perform oral hygiene themselves, increasing their risk for infections. Enhancing taste (option A) and preparing for meals (option D) are not relevant for unconscious patients, and avoiding disturbance (option C) is not a reason to withhold necessary care.
Question 3
Which technique is most appropriate for a nurse to use when moving a patient from a bed to a wheelchair?
A. The log roll technique
B. The two-person lift
C. The mechanical lift
D. The solo lift
Answer:
C. The mechanical lift
Explanation:
Using a mechanical lift is the most appropriate and safest technique when moving a patient from a bed to a wheelchair, especially if the patient is unable to assist with the transfer. This method minimizes the risk of injury to both the patient and the nurse by providing stable and supported movement. The log roll technique (option A) is more appropriate for turning patients in bed, while the two-person lift (option B) and solo lift (option D) are generally less safe and could risk physical strain or injury.