Preparing for the NCLEX PN® Exam requires a solid understanding of the cardiovascular system, a vital component of Adult Health. Mastery of cardiac anatomy, physiology, and common disorders is essential. This knowledge provides insights into patient care, including managing heart diseases, monitoring circulatory health, and understanding interventions, critical for nursing practice success
Learning Objective
In studying the “Cardiovascular System” for the NCLEX PN® Exam, you should focus on understanding the structure and function of the heart and blood vessels, including the cardiac cycle, conduction system, and blood flow dynamics. Recognize common cardiovascular conditions such as hypertension, heart failure, and arrhythmias, and the nursing interventions required for their management. Evaluate the principles of pharmacological treatments, including anticoagulants, antihypertensives, and diuretics, and their effects on cardiovascular health. Develop skills to interpret vital signs, ECG results, and symptoms related to cardiovascular disorders. Apply this knowledge to clinical scenarios and prioritize care in cardiovascular emergencies effectively.
Anatomy and Physiology of the Cardiovascular System
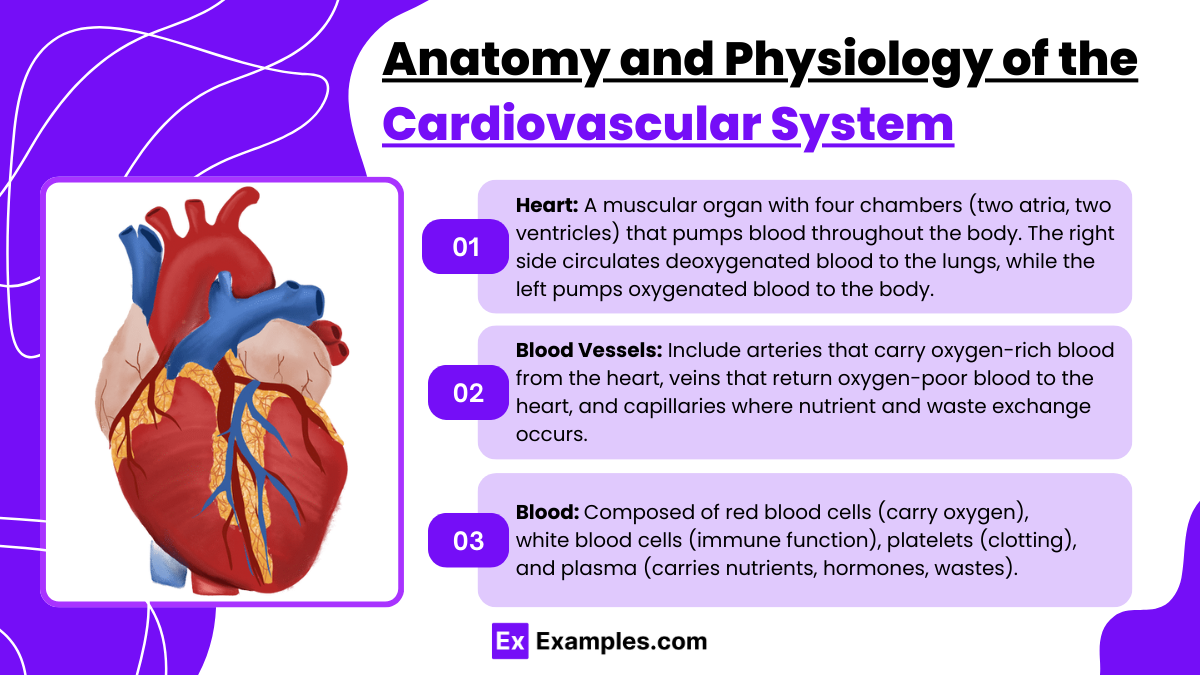
The cardiovascular system, also known as the circulatory system, is essential for sustaining life by transporting blood throughout the body. This system is composed of the heart, blood vessels, and blood itself. Here’s a breakdown of its main components and functions:
- Heart: The heart is a muscular organ located in the chest cavity, slightly to the left of the center. It functions as a pump to circulate blood throughout the body. The heart has four chambers: two upper chambers called atria and two lower chambers called ventricles. The right side of the heart receives deoxygenated blood from the body and pumps it to the lungs for oxygenation. The left side receives oxygenated blood from the lungs and pumps it to the rest of the body.
- Blood Vessels: These are the channels through which blood flows. There are three major types of blood vessels:
- Arteries: These carry oxygen-rich blood away from the heart to all parts of the body. The largest artery is the aorta.
- Veins: These carry oxygen-poor blood back to the heart. The largest veins are the superior and inferior vena cava.
- Capillaries: These are small, thin blood vessels that connect arteries and veins. Capillaries are sites of nutrient and waste exchange between blood and tissues.
- Blood: Blood is composed of red blood cells, white blood cells, platelets, and plasma. Red blood cells contain hemoglobin, which binds oxygen and delivers it to tissues. White blood cells are involved in immune response. Platelets help in blood clotting, and plasma is the liquid component that transports nutrients, hormones, and waste products.
The cardiovascular system is crucial for maintaining homeostasis. It delivers nutrients and oxygen to cells, removes waste products like carbon dioxide, helps regulate body temperature, and distributes hormones. This system also plays a critical role in immune response and wound healing.
Cardiac Cycle and Hemodynamics
The cardiac cycle and hemodynamics are fundamental aspects of how the heart functions and how blood flows through the cardiovascular system. Here’s a detailed explanation of these processes:
Cardiac Cycle
The cardiac cycle refers to the sequence of events that occur as the heart beats, involving the contraction and relaxation of the atria and ventricles to pump blood throughout the body. The cycle is divided into several phases:
- Diastole (Relaxation Phase):
- Ventricular Diastole: Ventricles relax, AV valves open, allowing blood to flow from atria to ventricles.
- Atrial Systole: Atria contract to complete ventricular filling.
- Systole (Contraction Phase):
- Isovolumetric Contraction: Ventricles contract with all valves closed, increasing pressure.
- Ventricular Ejection: Pressure forces semilunar valves open, ejecting blood into aorta and pulmonary artery.
Hemodynamics
Hemodynamics refers to the dynamics of blood flow within the cardiovascular system, primarily influenced by heart action, blood volume, resistance to flow, and blood pressure. Key aspects include:
- Blood Pressure: Force exerted by blood against vessel walls, influenced by cardiac output, blood volume, and resistance.
- Cardiac Output (CO): Volume of blood the heart pumps per minute, calculated as stroke volume x heart rate.
- Vascular Resistance: Resistance to blood flow within vessels, mainly affected by vessel diameter.
- Venous Return: Flow of blood back to the heart, critical for maintaining cardiac output.
- Regulation of Blood Flow: Adjusted by vasodilation and vasoconstriction in response to tissue demands.
Pharmacological Management of Cardiovascular Conditions
Pharmacological management of cardiovascular conditions involves various medications tailored to treat specific aspects of heart disease and its risk factors. Here’s an overview of the main categories of cardiovascular medications and their purposes:
1. Antihypertensives
These drugs are used to lower high blood pressure, reducing the risk of heart attack, stroke, and kidney disease. Major classes include:
- ACE Inhibitors (e.g., lisinopril, enalapril): Block the conversion of angiotensin I to angiotensin II, lowering blood pressure and reducing workload on the heart.
- Beta-Blockers (e.g., metoprolol, atenolol): Reduce heart rate and cardiac output, lowering blood pressure and heart muscle oxygen demand.
- Calcium Channel Blockers (e.g., amlodipine, verapamil): Prevent calcium from entering cells of the heart and blood vessel walls, leading to lower blood pressure.
- Diuretics (e.g., hydrochlorothiazide, furosemide): Increase urine output to reduce blood volume, thereby lowering blood pressure.
2. Antiarrhythmics
These drugs help manage abnormal heart rhythms and include:
- Sodium Channel Blockers (e.g., lidocaine, procainamide): Reduce the ability of the myocardial cells to conduct electricity, stabilizing the heart rhythm.
- Potassium Channel Blockers (e.g., amiodarone, sotalol): Prolong repolarization and prevent recurrent arrhythmias.
- Beta-Blockers: Also used to slow the heart rate in conditions like atrial fibrillation.
3. Antianginals
Used to manage angina pectoris (chest pain):
- Nitrates (e.g., nitroglycerin, isosorbide mononitrate): Dilate blood vessels, increasing blood flow to the heart muscle and decreasing its oxygen demand.
- Beta-Blockers and Calcium Channel Blockers: Reduce myocardial oxygen consumption by lowering heart rate and contractility.
4. Anticoagulants and Antiplatelets
These are crucial in preventing blood clot formation:
- Anticoagulants (e.g., warfarin, heparin, direct oral anticoagulants like apixaban): Inhibit the clotting factors to prevent clot formation.
- Antiplatelets (e.g., aspirin, clopidogrel): Prevent platelets from clumping together to form clots.
5. Lipid-lowering Drugs
These medications reduce cholesterol levels and include:
- Statins (e.g., atorvastatin, simvastatin): Inhibit the enzyme involved in cholesterol synthesis, lowering LDL cholesterol.
- Fibrates (e.g., fenofibrate): Mainly lower triglycerides and slightly increase HDL cholesterol.
6. Heart Failure Medications
These help manage symptoms and improve survival in heart failure patients:
- ACE Inhibitors and Beta-Blockers: Improve survival rates.
- Diuretics: Reduce fluid overload.
- Aldosterone Antagonists (e.g., spironolactone): Block aldosterone, reducing fluid retention and fibrosis.
Diagnostic and Monitoring Tools
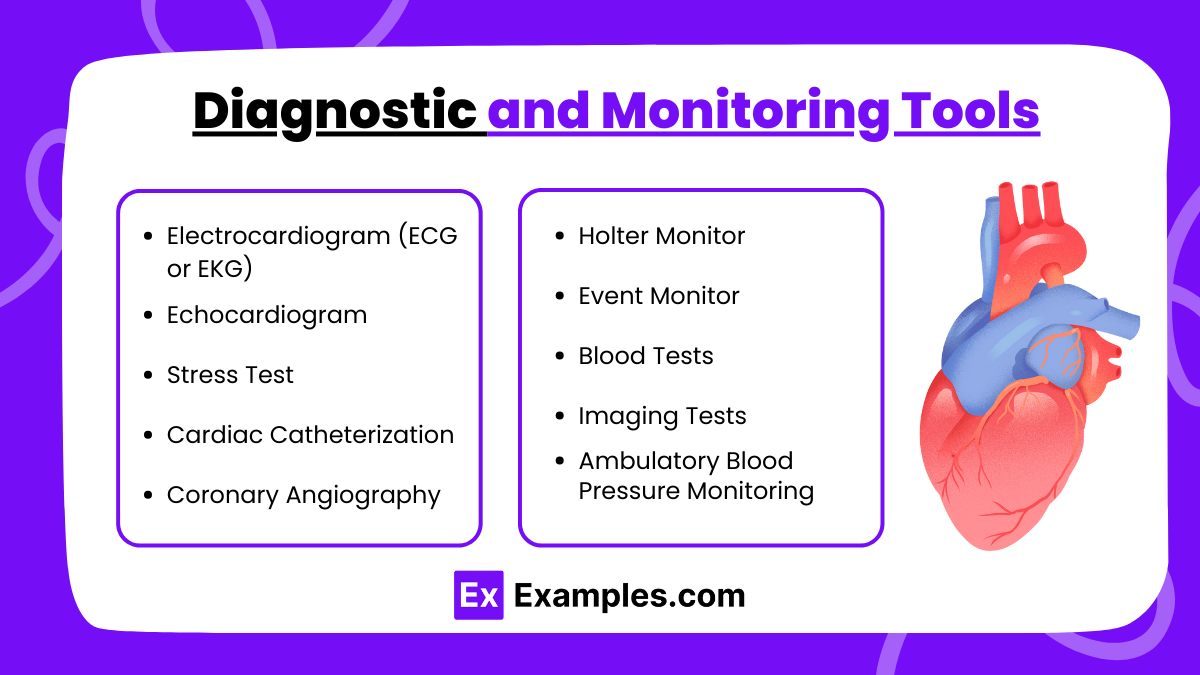
The diagnosis and monitoring of cardiovascular diseases involve various tools and technologies that help in assessing heart function, detecting abnormalities, and guiding treatment. Here’s a breakdown of the key diagnostic and monitoring tools used in cardiology:
1. Electrocardiogram (ECG or EKG)
- Purpose: Records the electrical activity of the heart.
- Uses: Diagnoses arrhythmias, heart attacks, and other heart conditions.
2. Echocardiogram
- Purpose: Uses ultrasound waves to produce images of the heart’s structure and function.
- Uses: Assesses cardiac output, detects structural abnormalities, and evaluates the heart’s pumping efficiency.
3. Stress Test
- Purpose: Measures the heart’s performance and capacity under physical stress.
- Uses: Diagnoses coronary artery disease and assesses the severity of heart conditions.
4. Cardiac Catheterization
- Purpose: Involves inserting a catheter into the heart’s blood vessels.
- Uses: Measures pressures within the heart, collects blood samples, and conducts tissue biopsies.
5. Coronary Angiography
- Purpose: Uses X-ray imaging to view the heart’s blood vessels.
- Uses: Identifies blockages or narrowing in the coronary arteries.
6. Holter Monitor
- Purpose: A portable device worn by a patient to continuously record the heart’s rhythms over 24-48 hours.
- Uses: Detects intermittent cardiac arrhythmias not captured during a standard ECG.
7. Event Monitor
- Purpose: Similar to a Holter monitor but used for longer periods.
- Uses: Patients activate it when they experience symptoms of a heart problem.
8. Blood Tests
- Purpose: Analyze various substances in the blood.
- Uses: Detects markers of heart damage like troponin or conditions affecting the heart such as anemia or thyroid disease.
9. Imaging Tests
- Purpose: Includes CT scans, MRI scans, and nuclear imaging.
- Uses: Visualizes the heart structure, assesses metabolic activity, and detects inflammation or scarring.
10. Ambulatory Blood Pressure Monitoring
- Purpose: Records blood pressure at regular intervals over 24 hours.
- Uses: Provides a detailed profile of blood pressure changes throughout the day and night.
These tools are crucial for providing comprehensive information about the heart’s structure, function, and the presence of any cardiovascular disease, guiding both diagnosis and management strategies effectively.
Examples
Examples 1: Heart Failure Case Study
A patient presents with shortness of breath, fatigue, and swollen ankles. Their medical history includes hypertension and type 2 diabetes. An echocardiogram shows decreased ejection fraction. Nursing interventions include monitoring fluid status, administering prescribed diuretics, and educating the patient about sodium restriction and fluid intake limits.
Examples 2: Management of Acute Myocardial Infarction (AMI)
A patient arrives in the emergency department with chest pain radiating to the left arm, sweating, and nausea. ECG shows ST elevation. Immediate nursing actions include administering oxygen, aspirin, and nitroglycerin as ordered, preparing for thrombolytic therapy, and continuous monitoring of vital signs and cardiac rhythm.
Examples 3: Hypertension Monitoring and Education
A newly diagnosed hypertensive patient needs education on medication adherence, lifestyle changes, and self-monitoring of blood pressure. The nurse demonstrates how to use a home blood pressure monitor and discusses the importance of dietary changes such as reducing salt intake and increasing physical activity.
Examples 4: Atrial Fibrillation Management
A patient with a history of atrial fibrillation presents with palpitations and dizziness. The nurse must check the heart rate and rhythm, ensure anticoagulation therapy is administered as prescribed to prevent stroke, and educate the patient about recognizing symptoms that require immediate medical attention.
Examples 5: Post-Cardiac Catheterization Care
After a cardiac catheterization procedure to assess for coronary artery disease, the patient requires monitoring for signs of bleeding from the catheter insertion site, signs of limb ischemia, and arrhythmias. Nurses provide instructions on activity restrictions and wound care and ensure the patient understands follow-up appointments and medication adjustments.
Practice Questions
Question 1
A patient is admitted with a diagnosis of left-sided heart failure. Which of the following clinical manifestations is most likely to be observed?
A. Peripheral edema
B. Pulmonary congestion
C. Jugular vein distention
D. Hepatomegaly
Answer
B. Pulmonary congestion
Explanation
Left-sided heart failure leads to blood backing up into the lungs because the left ventricle is unable to pump blood effectively. This results in pulmonary congestion, which manifests as dyspnea, crackles on auscultation, and orthopnea.
- A. Peripheral edema: More commonly associated with right-sided heart failure.
- C. Jugular vein distention: A sign of right-sided heart failure.
- D. Hepatomegaly: Another sign of right-sided heart failure caused by congestion in systemic circulation.
Question 2
Which of the following ECG findings is most indicative of a myocardial infarction (MI)?
A. Prolonged PR interval
B. ST-segment elevation
C. T-wave inversion
D. Atrial fibrillation
Answer
B. ST-segment elevation
Explanation
ST-segment elevation is a hallmark finding in an acute myocardial infarction (MI), indicating injury to the heart muscle. Immediate medical intervention is required to prevent further damage.
- A. Prolonged PR interval: Suggests first-degree heart block, not MI.
- C. T-wave inversion: May indicate ischemia, but not as specific to MI as ST-segment elevation.
- D. Atrial fibrillation: An arrhythmia that may coexist with MI but is not a defining feature.
Question 3
A nurse is administering furosemide (Lasix) to a patient with heart failure. Which lab value should the nurse monitor most closely?
A. Serum calcium
B. Serum potassium
C. Blood urea nitrogen (BUN)
D. Serum sodium
Answer
B. Serum potassium
Explanation
Furosemide is a loop diuretic that can cause significant potassium loss through urine, leading to hypokalemia. Monitoring serum potassium levels is critical to prevent complications such as arrhythmias.
- A. Serum calcium: Not directly impacted by furosemide.
- C. BUN: May be elevated with dehydration, but potassium is a more critical concern.
- D. Serum sodium: Can be affected, but potassium monitoring takes priority in this case.