Preparing for the NCLEX PN® Exam necessitates a thorough understanding of the endocrine system, a fundamental component of Adult Health. Mastery of glandular functions, hormone regulation, and metabolic processes is essential. This knowledge provides insights into patient care management, including disorders like diabetes and thyroid dysfunction, critical for effective nursing practice.
Learning Objective
In studying the “Endocrine System” for the NCLEX PN® Exam, you should aim to understand the functions and disorders of various endocrine glands, including the thyroid, pancreas, adrenal, and pituitary glands. Learn to identify hormonal imbalances and their clinical manifestations, such as diabetes, hyperthyroidism, and Addison’s disease. Evaluate the principles of diagnostic tests and therapeutic interventions, including hormone replacement and pharmacological management. Additionally, explore how hormonal feedback mechanisms regulate body processes and apply this knowledge to patient care scenarios, focusing on maintaining homeostasis and managing chronic conditions related to endocrine dysfunctions in your nursing practice.
Overview of the Endocrine System
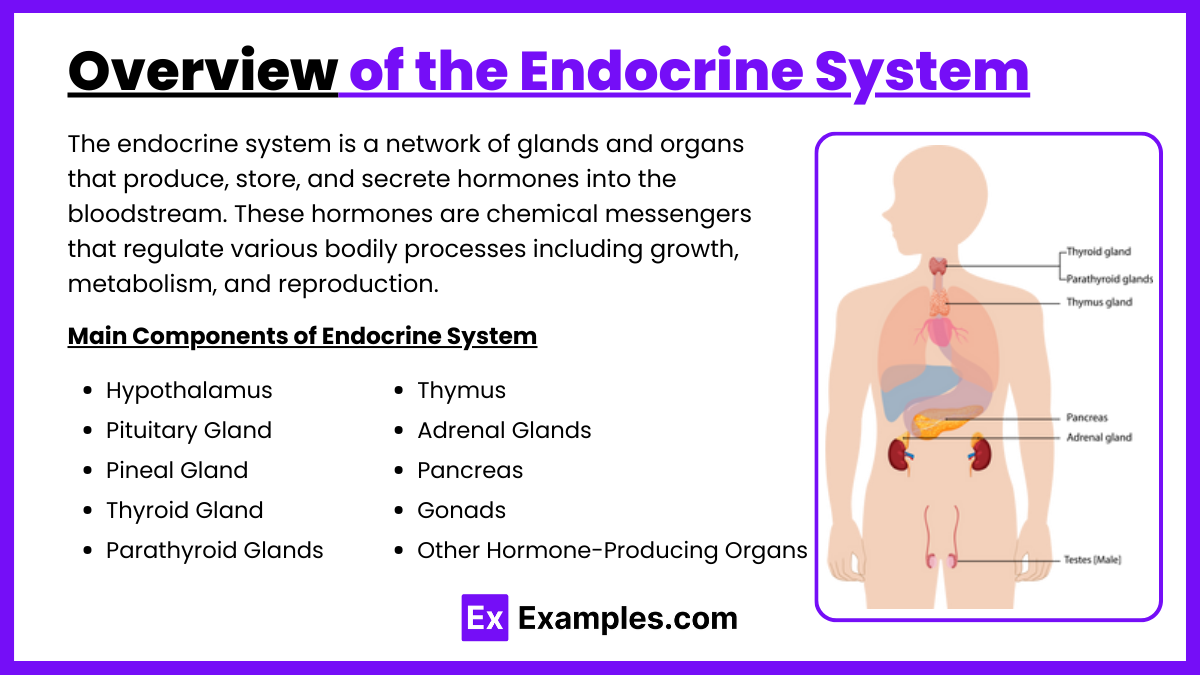
The endocrine system is a network of glands and organs that produce, store, and secrete hormones into the bloodstream. These hormones are chemical messengers that regulate various bodily processes including growth, metabolism, and reproduction. Here’s a detailed overview of the main components and functions of the endocrine system:
1. Hypothalamus
- Location: Part of the brain.
- Function: Regulates the pituitary gland and maintains homeostasis by controlling body temperature, hunger, thirst, and sleep cycles. It produces hormones that can either stimulate or inhibit hormone release from the pituitary.
2. Pituitary Gland
- Location: Base of the brain.
- Function: Often called the “master gland,” it controls other endocrine glands and regulates critical body functions. It releases hormones that influence growth, metabolism, and fertility.
3. Pineal Gland
- Location: Center of the brain.
- Function: Produces melatonin, which regulates sleep-wake cycles.
4. Thyroid Gland
- Location: Front of the neck.
- Function: Produces thyroid hormones that regulate metabolism, energy generation, and body temperature.
5. Parathyroid Glands
- Location: Behind the thyroid gland.
- Function: Produce parathyroid hormone which regulates calcium levels in the blood.
6. Thymus
- Location: Upper chest, beneath the sternum.
- Function: Produces hormones important for the development of the immune system in early life.
7. Adrenal Glands
- Location: Top of each kidney.
- Function: Produce hormones that help regulate metabolism, immune system, blood pressure, and response to stress. These include cortisol and adrenaline.
8. Pancreas
- Location: Behind the stomach.
- Function: Produces insulin and glucagon, which regulate blood sugar levels.
9. Gonads
- Ovaries (in females) and Testes (in males)
- Function: Produce hormones that regulate sexual development, reproduction, and secondary sexual characteristics such as breast development and facial hair.
10. Other Hormone-Producing Organs
- Including: Kidneys (produce erythropoietin which influences red blood cell production), Liver (produces angiotensinogen which affects blood pressure), and Fat cells (produce leptin which influences appetite and fat storage).
Diagnostic and Therapeutic Interventions
Diagnostic and therapeutic interventions are essential components of medical practice, aiding in the identification of diseases and conditions and providing effective treatments to manage or cure them. Here’s an overview of key diagnostic and therapeutic interventions used in various medical fields:
Diagnostic Interventions
- Imaging Techniques
- X-rays: Detect abnormalities in bones and certain body tissues.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues, organs, and the nervous system.
- CT Scans (Computed Tomography): Offers cross-sectional images of the body to detect tumors, fractures, and internal bleeding.
- Ultrasound: Uses sound waves to create images of internal organs, commonly used in prenatal care and diagnosing gallbladder disease.
- Lab Tests
- Blood Tests: Assess various blood components to detect conditions like diabetes, anemia, and infection.
- Urine Tests: Detect kidney disease, diabetes, and urinary tract infections.
- Biopsies: Involve extracting tissue samples to diagnose cancer and other diseases.
- Endoscopy
- Gastroscopy and Colonoscopy: Inspect the gastrointestinal tract for abnormalities such as ulcers, polyps, and cancers.
- Genetic Testing
- Screen for genetic disorders: Such as cystic fibrosis, sickle cell disease, and hereditary cancers.
Therapeutic Interventions
- Surgical Procedures
- Laparoscopy: Minimally invasive surgery used for operations in the abdomen.
- Open Surgery: Traditional method requiring larger incisions, used for complex procedures.
- Robotic Surgery: Enhances precision, flexibility, and control during the operation, minimizing recovery time.
- Pharmacotherapy
- Antibiotics: Treat bacterial infections.
- Chemotherapy: Treats cancer by killing or slowing the growth of cancer cells.
- Antivirals: Treat viral infections like influenza and HIV.
- Radiation Therapy
- Used to treat cancer: By targeting malignant cells with ionizing radiation to destroy cancerous tissue.
- Physical Therapy and Rehabilitation
- Aids in recovery: After injuries or surgeries, improving mobility and reducing pain.
- Psychotherapy
- Treats mental health issues: Such as depression, anxiety, and PTSD through various therapeutic techniques.
Pathophysiology and Clinical Management
Pathophysiology and clinical management are core aspects of medical practice, providing a deep understanding of the mechanisms of disease and guiding effective treatment strategies. Here’s a concise overview of each component:
Pathophysiology
Pathophysiology refers to the study of the functional changes that occur in the body as a result of a disease or medical condition. It bridges the gap between basic science and clinical practice by explaining the processes within the body that result in the signs and symptoms of a disease. Understanding pathophysiology involves:
- Identifying Abnormal Processes: Recognizing how normal physiological processes are altered by disease or injury.
- Disease Mechanisms: Exploring how diseases develop from genetic, biochemical, or immunological abnormalities affecting cellular function.
- Progression of Disease: Observing how diseases evolve over time, potentially worsening or responding to treatment.
- Impact on Body Systems: Examining how diseases affect different body systems, often leading to multiple symptoms and complex health issues.
Clinical Management
Clinical management involves the application of medical knowledge to diagnose, treat, and prevent diseases. Effective clinical management is based on a thorough understanding of pathophysiology and typically includes:
- Diagnosis: Utilizing history taking, physical examination, and diagnostic tests to accurately identify the disease or condition.
- Treatment Planning: Developing a tailored treatment strategy based on the diagnosis, patient’s condition, and current medical guidelines. This might include:
- Medication: Prescribing drugs to treat symptoms or address root causes.
- Surgery: Recommending surgical interventions to remove, repair, or improve the function of diseased organs or structures.
- Therapy: Engaging in physical, occupational, or psychological therapies to restore function or manage conditions.
- Lifestyle Adjustments: Advising on diet, exercise, and other lifestyle changes to improve health and well-being.
- Monitoring and Follow-Up: Regularly assessing the patient’s response to treatment through follow-up appointments, repeated tests, and ongoing assessments.
- Preventive Measures: Implementing strategies to prevent disease progression or occurrence, including vaccinations, screening, and patient education.
Examples
Example 1: Management of Type 1 Diabetes
- A young patient diagnosed with Type 1 diabetes needs comprehensive education on insulin administration, glucose monitoring, and diet management. The nurse demonstrates the use of an insulin pump and explains the importance of regular blood sugar testing, recognizing signs of hypo- and hyperglycemia, and dietary adjustments to manage their condition effectively.
Example 2: Post-Thyroidectomy Care
- A patient who has undergone a thyroidectomy for thyroid cancer requires careful monitoring for signs of hypocalcemia and damage to the parathyroid glands. The nurse monitors calcium levels, administers calcium supplements as prescribed, and educates the patient about the signs of hypocalcemia, such as tingling in the lips and fingers and muscle cramps.
Example 3: Addison’s Disease Management
- A patient with Addison’s disease presents with fatigue, weight loss, and hyperpigmentation. The nurse administers hydrocortisone as ordered, educates the patient on stress management techniques and the importance of wearing a medical alert bracelet, and prepares an emergency steroid kit for use during an adrenal crisis.
Example 4: Treatment of Hyperthyroidism
- A patient with hyperthyroidism exhibits symptoms like rapid heartbeat, weight loss, and anxiety. The nurse administers antithyroid medications, monitors the patient for side effects, and provides education on dietary changes to avoid foods that may exacerbate symptoms, such as excessive iodine.
Example 5: Handling Hypoparathyroidism
- A post-surgical patient with accidental removal of the parathyroid glands during thyroid surgery shows symptoms of hypocalcemia. The nurse ensures prompt calcium and vitamin D administration, monitors serum calcium levels regularly, and educates the patient on recognizing symptoms of calcium deficiency and the importance of follow-up care to adjust supplementation levels.
Practice Questions
Question 1
Which hormone is primarily involved in the regulation of serum calcium levels?
A. Cortisol
B. Insulin
C. Parathyroid hormone (PTH)
D. Thyroxine (T4)
Answer:
C. Parathyroid hormone (PTH)
Explanation:
Parathyroid hormone (PTH) is secreted by the parathyroid glands and plays a critical role in the regulation of serum calcium levels. It increases blood calcium levels by stimulating the release of calcium from bones, increasing calcium absorption in the intestines, and promoting calcium reabsorption in the kidneys. Cortisol (option A) is involved in stress response and metabolism regulation, insulin (option B) regulates blood glucose levels, and thyroxine (T4, option D) regulates metabolism.
Question 2
A patient with untreated diabetes mellitus will most likely exhibit which of the following?
A. Hypoglycemia
B. Hyperglycemia
C. Decreased urine output
D. Low serum potassium levels
Answer:
B. Hyperglycemia
Explanation:
Untreated diabetes mellitus typically leads to hyperglycemia, which is characterized by high blood sugar levels. This occurs due to the body’s inability to produce sufficient insulin (Type 1 diabetes) or use insulin effectively (Type 2 diabetes), resulting in poor glucose uptake into cells. Hypoglycemia (option A) occurs typically due to excessive insulin administration, not untreated diabetes. Decreased urine output (option C) and low serum potassium levels (option D) are not directly associated with untreated diabetes.
Question 3
Which of the following conditions is a common complication of uncontrolled hyperthyroidism?
A. Bradycardia
B. Hypotension
C. Thyroid storm
D. Hypoglycemia
Answer:
C. Thyroid storm
Explanation:
Thyroid storm is a severe and potentially life-threatening complication of uncontrolled hyperthyroidism, characterized by an extreme overproduction of thyroid hormones. It presents with symptoms such as very high fever, tachycardia, hypertension, and delirium. Bradycardia (option A) and hypotension (option B) are typically not associated with hyperthyroidism, which generally causes tachycardia and potential hypertension. Hypoglycemia (option D) is unrelated to thyroid hormone levels.