Preparing for the NCLEX PN® Exam requires a thorough understanding of Ethical/Legal Fundamentals, essential components of nursing practice. Mastery of ethical principles, legal responsibilities, and professional boundaries is crucial. This knowledge aids in making informed decisions, protecting patient rights, and ensuring the delivery of ethical and legally compliant care, pivotal for nursing credibility and trust.
Learning Objective
In studying "Ethical/Legal in Fundamentals" for the NCLEX PN® Exam, you should aim to understand the key ethical principles and legal considerations that govern nursing practice. Learn to identify and apply concepts such as autonomy, justice, beneficence, and non-maleficence in patient care scenarios. Evaluate the impact of legal issues like confidentiality, informed consent, and documentation requirements on nursing responsibilities. Additionally, explore the role of the nurse in advocating for patient rights and ethical standards in healthcare settings. Apply this knowledge to navigate ethical dilemmas and legal challenges effectively, ensuring compassionate, ethical, and legally sound patient care.
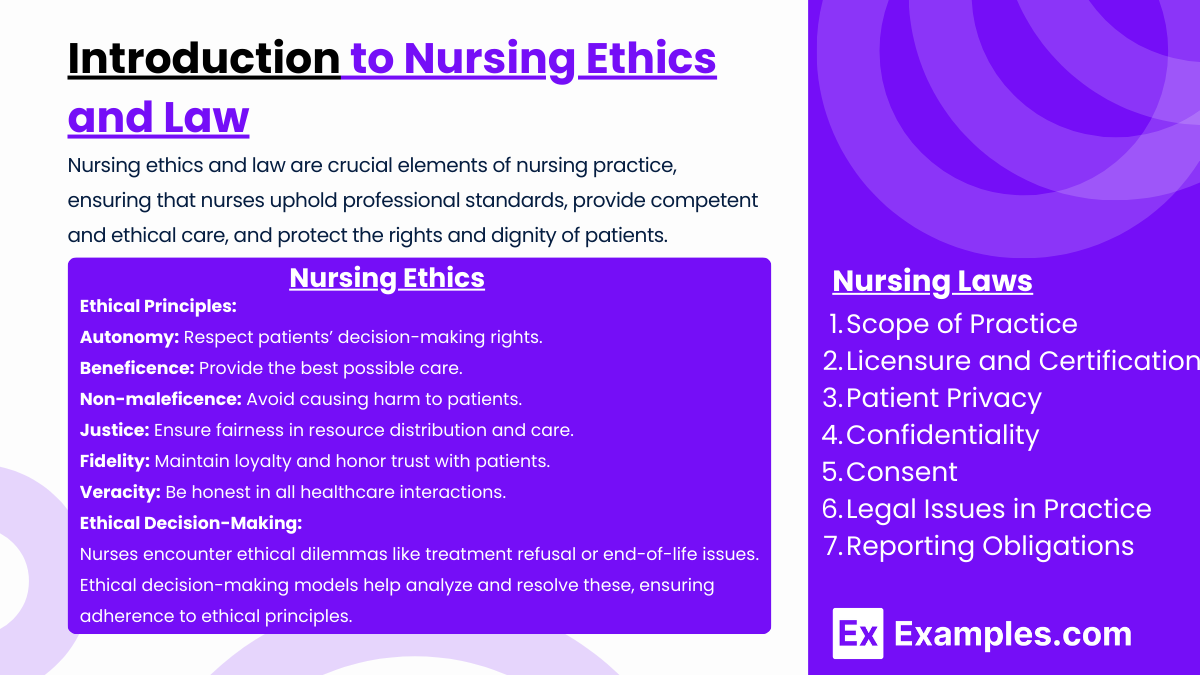
Introduction to Nursing Ethics and Law
Nursing ethics and law are crucial elements of nursing practice, ensuring that nurses uphold professional standards, provide competent and ethical care, and protect the rights and dignity of patients. Here is an introduction to the key concepts and principles in nursing ethics and law:
Nursing Ethics
Ethical Principles:
Autonomy: Respecting patients' rights to make their own decisions about their healthcare.
Beneficence: Acting in the best interest of the patient to do good and provide the best possible care.
Non-maleficence: Avoiding harm to patients. This includes preventing harm and ensuring the risks associated with care do not outweigh the benefits.
Justice: Ensuring fairness in distributing resources and providing care. This includes considerations of equity and fairness in treatment decisions.
Fidelity: Maintaining loyalty and commitment to the patient and honoring the trust placed in the nurse.
Veracity: Committing to truthfulness and honesty in interactions with patients and other healthcare professionals.
Ethical Decision-Making:
Nurses face complex ethical dilemmas in their daily practice. These can range from conflicts over autonomy (such as patients refusing treatment) to issues related to end-of-life care. Utilizing ethical decision-making models can help nurses analyze and resolve these dilemmas effectively, considering all ethical principles involved.
Nursing Law
Scope of Practice:
Defined by each state’s Nurse Practice Act, which outlines what is legally permissible for nurses to perform in their roles. This includes specific actions, duties, and responsibilities that registered nurses (RNs), licensed practical nurses (LPNs), and advanced practice registered nurses (APRNs) are allowed to undertake.
Licensure and Certification:
Nurses must be licensed to practice in their respective states, which involves passing the National Council Licensure Examination (NCLEX) for registered nurses or practical nurses. Continuing education is typically required to maintain licensure.
Patient Privacy and Confidentiality:
Laws such as the Health Insurance Portability and Accountability Act (HIPAA) protect patient information. Nurses must ensure that all patient information remains confidential and is only shared with individuals who have a legal and legitimate need to know.
Consent:
Nurses must ensure that patients give informed consent before any and all medical treatments or procedures. This involves providing patients with clear and comprehensive information about the potential benefits, risks, and alternatives.
Legal Issues in Practice:
Nurses must be aware of legal issues such as malpractice, negligence, and liability in nursing practice. Understanding these areas helps prevent legal actions due to professional misconduct or failures in following the standard of care.
Reporting Obligations:
Nurses have a duty to report certain conditions, such as infectious diseases, or suspicions of abuse or neglect, according to state laws.
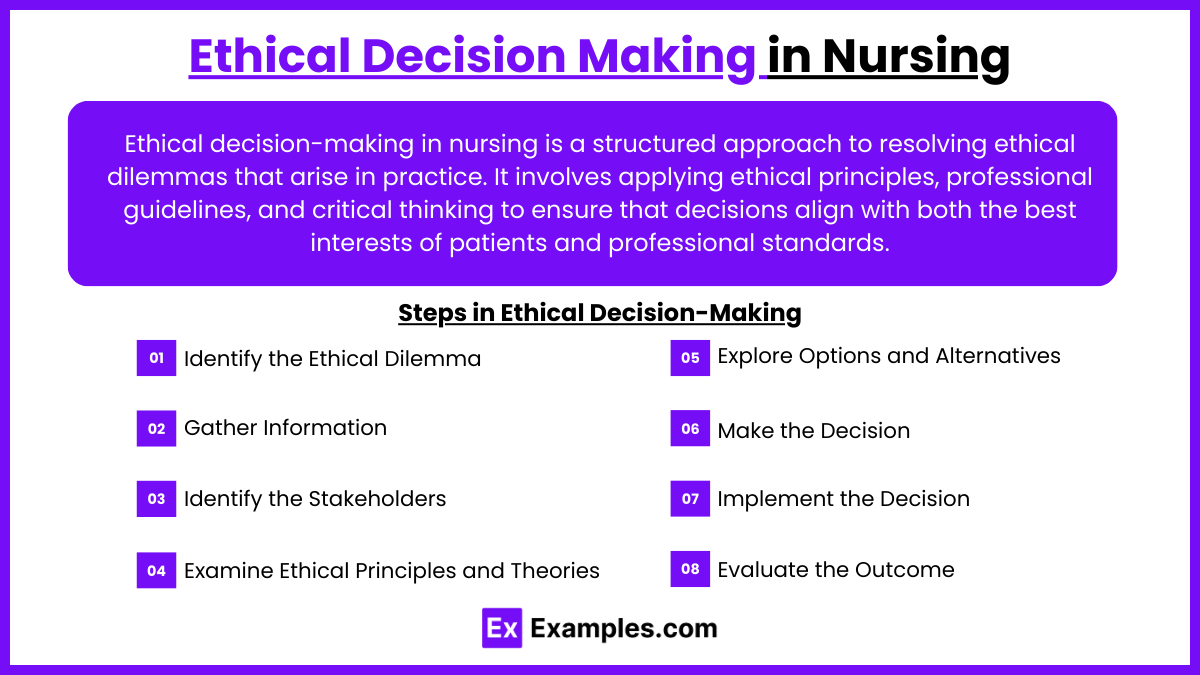
Ethical Decision Making in Nursing
Ethical decision-making in nursing is a structured approach to resolving ethical dilemmas that arise in practice. It involves applying ethical principles, professional guidelines, and critical thinking to ensure that decisions align with both the best interests of patients and professional standards. Here’s an overview of ethical decision-making in nursing:
Steps in Ethical Decision-Making
Identify the Ethical Dilemma:
Recognize the situation as an ethical issue that involves conflicting values, principles, or responsibilities.
Example: A patient refuses life-saving treatment, conflicting with the nurse's duty to preserve life.
Gather Information:
Collect all relevant medical, personal, social, and legal facts.
Consider patient preferences, cultural values, family involvement, and institutional policies.
Identify the Stakeholders:
Determine who is affected by the decision, such as the patient, family, healthcare team, and the institution.
Examine Ethical Principles and Theories:
Apply core ethical principles such as:
Autonomy: Respect for the patient’s right to make informed choices.
Beneficence: Promoting the patient’s well-being.
Non-maleficence: Avoiding harm.
Justice: Ensuring fairness and equality in care delivery.
Consider ethical theories like utilitarianism (greatest good for the greatest number) or deontology (duty-based ethics).
Explore Options and Alternatives:
Identify all possible courses of action and evaluate their potential outcomes.
Collaborate with the healthcare team, patient, and family to discuss viable solutions.
Make the Decision:
Choose the option that aligns best with ethical principles, patient preferences, and professional guidelines.
Document the rationale for the decision.
Implement the Decision:
Take action while maintaining clear communication with the patient, family, and healthcare team.
Ensure that the chosen course of action is carried out effectively and ethically.
Evaluate the Outcome:
Assess the impact of the decision on the patient, family, and healthcare team.
Reflect on whether the decision achieved the desired ethical and clinical outcomes.
Legal Responsibilities of Nurses
The legal responsibilities of nurses are crucial for maintaining safe, ethical, and professional healthcare practices. These responsibilities are governed by laws, regulations, and standards that ensure patient safety, uphold nursing practice integrity, and protect nurses from legal liability. Below is an overview of the key legal responsibilities of nurses:
1. Adherence to Scope of Practice
Defined by Nurse Practice Acts (NPAs): State-specific laws outline the roles, duties, and activities nurses are legally permitted to perform.
Understanding Limitations: Nurses must only perform tasks they are trained, licensed, and competent to carry out, avoiding actions that fall outside their scope.
2. Duty of Care
Standard of Care: Nurses are legally obligated to provide care that meets accepted standards, ensuring safety, competence, and professionalism.
Negligence and Malpractice:
Negligence: Failing to provide the expected standard of care, resulting in harm.
Malpractice: A form of professional negligence where improper or unethical conduct leads to patient injury.
3. Maintaining Patient Confidentiality
HIPAA Compliance: Nurses must protect patient information as mandated by the Health Insurance Portability and Accountability Act (HIPAA). This includes ensuring that electronic, verbal, and written data are securely handled.
Exceptions: Confidentiality can only be breached in cases of mandatory reporting (e.g., abuse, public health concerns).
4. Informed Consent
Ensuring Understanding: Nurses must verify that patients fully understand the benefits, risks, and alternatives of procedures or treatments before giving consent.
Witnessing Consent: Nurses often act as witnesses to the patient’s signature on consent forms, confirming the process has been followed appropriately.
5. Documentation and Record-Keeping
Accurate and Timely Entries: Nurses are responsible for maintaining precise, detailed, and timely patient records to reflect the care provided.
Legal Evidence: Documentation serves as legal evidence in the event of disputes or investigations. Incomplete or inaccurate records can result in legal liability.
6. Medication Administration
Five Rights of Medication Administration:
Right Patient
Right Medication
Right Dose
Right Route
Right Time
Preventing Errors: Nurses are legally accountable for safe medication administration and must report and document any errors immediately.
7. Mandatory Reporting
Abuse and Neglect: Nurses are legally required to report suspected cases of child abuse, elder abuse, or domestic violence.
Public Health Issues: Reporting communicable diseases, certain injuries, and unsafe working conditions is mandated in many jurisdictions.
8. Patient Advocacy
Protecting Patient Rights: Nurses have a legal and ethical obligation to advocate for the patient’s best interests, ensuring they receive appropriate care and treatment.
Acting Against Harm: Reporting unsafe practices, such as medical errors or abuse, is part of this responsibility.
9. Professional Licensure
Maintaining Credentials: Nurses must keep their license current by meeting continuing education requirements and renewing it on time.
Avoiding License Revocation: Actions such as practicing under the influence of drugs or alcohol, violating patient confidentiality, or engaging in unethical behavior can lead to disciplinary action or license revocation.
10. Legal Responsibilities in Delegation
Appropriate Delegation: Nurses must delegate tasks based on the competency of the individual and in compliance with institutional policies and NPAs.
Accountability: While tasks may be delegated, the nurse retains responsibility for patient outcomes.
Examples
Example 1: Ensuring Patient Autonomy
A nurse must ensure a patient's autonomy is respected when they decide against a recommended surgical procedure. The nurse explains the risks and benefits thoroughly and documents the patient's decision, ensuring informed consent is fully supported and recorded.
Example 2: Managing Confidential Information
A nurse handles a situation where a patient's family members ask for details about the patient's condition. The nurse carefully explains the importance of patient confidentiality and ensures that information is only shared with individuals who have a legal right to know, adhering to HIPAA guidelines.
Example 3: Documentation of Care
A nurse meticulously documents the care provided to a patient during their shift, including all medications administered, vital signs monitored, and any patient complaints or incidents. This precise documentation serves as a legal record and can be crucial in the event of a malpractice claim.
Example 4: Dealing with End-of-Life Decisions
In a case where a patient is unable to make decisions due to a terminal illness, a nurse facilitates discussions between the family and healthcare team about advance directives and end-of-life care options, ensuring all parties understand the legal and ethical implications of their decisions.
Example 5: Ethical Dilemma in Patient Care
A nurse encounters an ethical dilemma when a patient with dementia resists taking their medication. The nurse uses ethical decision-making skills to balance the patient's right to refuse treatment with the ethical principle of beneficence, seeking guidance from the healthcare team and the patient's family to find the best solution.
Practice Questions
Question 1
What is the primary purpose of obtaining informed consent before a surgical procedure?
A. To ensure the patient is aware of the financial costs associated with the procedure.
B. To ensure that the patient understands the risks, benefits, and alternatives to the procedure.
C. To protect the hospital from legal action.
D. To ensure that the patient complies with post-operative care.
Answer:
B. To ensure that the patient understands the risks, benefits, and alternatives to the procedure.
Explanation:
Informed consent is a fundamental ethical and legal requirement in healthcare that ensures patients are fully informed about the risks, benefits, and alternatives to a proposed medical procedure or treatment. This empowers the patient to make a knowledgeable decision about their own healthcare, respecting their autonomy. It is not primarily about financial costs (option A), protecting the hospital legally (option C), or ensuring compliance with care post-procedure (option D), though these might also be considerations.
Question 2
A nurse witnesses a coworker taking a patient's prescribed narcotic medication. What is the nurse's best action?
A. Confront the coworker privately.
B. Ignore the incident to avoid conflict.
C. Report the incident to a supervisor immediately.
D. Document the incident in the patient’s chart.
Answer:
C. Report the incident to a supervisor immediately.
Explanation:
The ethical and legal obligation of a nurse is to ensure patient safety and uphold the law. Observing a coworker diverting medication is a serious offense that could harm patients and is illegal. The appropriate action is to report the incident to a supervisor immediately to ensure that proper investigations and actions can be taken. Confronting the coworker (option A) or documenting the incident in the patient's chart (option D) without reporting it does not address the root of the issue, and ignoring it (option B) is unethical and irresponsible.
Question 3
Which scenario is an example of a breach in patient confidentiality?
A. Discussing patient care with another nurse involved in the patient’s treatment.
B. Sharing patient information during a handover meeting in a private setting.
C. Discussing patient details with a friend who works in the same hospital but not in patient care.
D. Consulting with a physician about the patient’s diagnosis in a private office.
Answer:
C. Discussing patient details with a friend who works in the same hospital but not in patient care.
Explanation:
Confidentiality is a legal and ethical obligation that involves keeping a patient's personal and health information private unless consent to share the information is given. Discussing patient details with someone not involved in the patient’s care, even if they work in the same hospital, is a clear breach of confidentiality. The other options involve sharing information with healthcare professionals who are directly involved in the patient's care or in settings where such discussions are appropriate and protected, which are considered acceptable and necessary for effective patient care.