The “Leadership & Management: Ethical/Legal” component of the NCLEX-PN® exam focuses on the ethical principles and legal responsibilities that guide nursing practice. This section assesses a nurse’s ability to uphold patient rights, ensure confidentiality, and make ethical decisions in complex healthcare settings. It also emphasizes the legal aspects of nursing, including scope of practice, informed consent, and patient advocacy. Practical nurses must demonstrate sound judgment, accountability, and leadership skills to manage ethical dilemmas, adhere to laws, and maintain high professional standards.
Learning Objectives
In studying “Leadership & Management: Ethical/Legal” for the NCLEX-PN® Exam, you should learn to understand key ethical principles such as autonomy, beneficence, nonmaleficence, justice, fidelity, and veracity. Analyze the legal responsibilities of practical nurses, focusing on the Nurse Practice Act (NPA), scope of practice, patient rights, and confidentiality under HIPAA. Evaluate how ethical dilemmas and legal issues affect nursing decisions and patient outcomes. Explore nursing considerations like informed consent, delegation, documentation, and reporting. Apply knowledge to ensure ethical decision-making, maintain patient privacy, promote advocacy, and prevent liability issues to safeguard patient safety, enhance care quality, and support professional accountability.
1. Ethical Principles in Nursing Leadership and Management
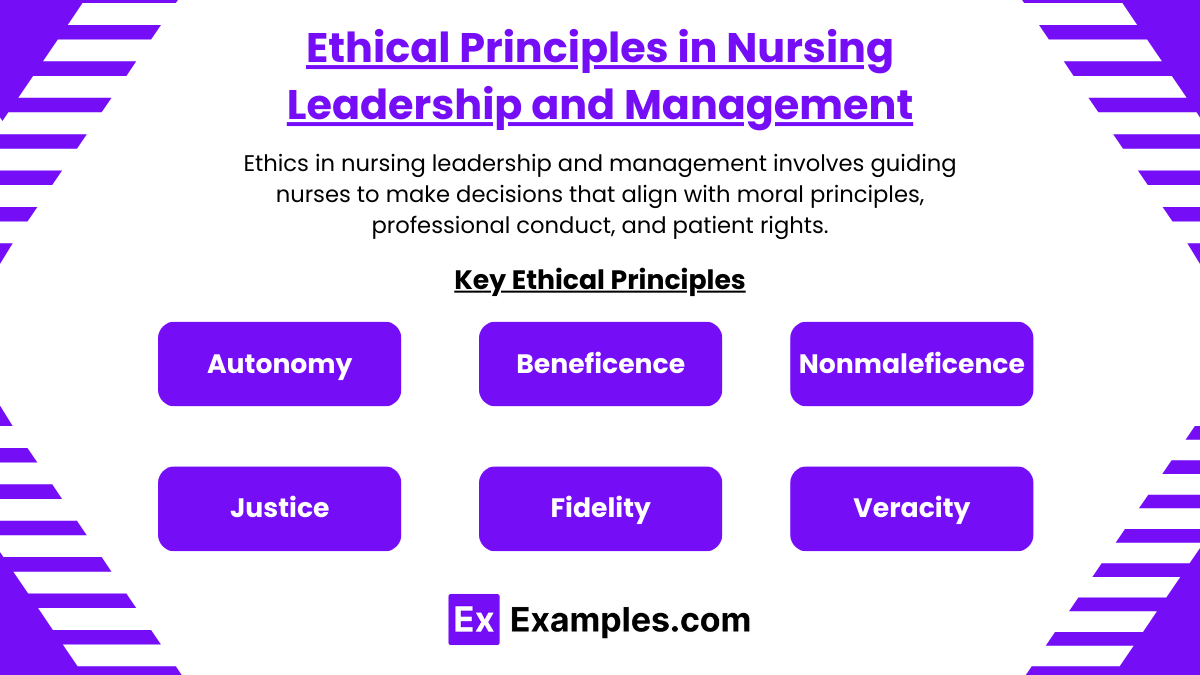
Ethics in nursing leadership and management involves guiding nurses to make decisions that align with moral principles, professional conduct, and patient rights. Ethical leadership ensures fair treatment, patient advocacy, and adherence to core values.
Key Ethical Principles
- Autonomy: Ensuring patients have the right to make their own healthcare decisions. Nurse leaders must respect and support patient autonomy, even when patients make choices different from the nurse’s personal beliefs.
- Beneficence: Acting for the benefit of patients by promoting their health, well-being, and safety. Nurse managers must guide staff to prioritize the best outcomes for patients.
- Nonmaleficence: Avoiding harm to patients. Nurse leaders should identify potential risks and create protocols to reduce errors or adverse outcomes.
- Justice: Ensuring fairness and equity in the distribution of healthcare services. Nurse leaders must avoid bias and ensure all patients receive equal treatment.
- Fidelity: Maintaining loyalty and confidentiality. Nurse leaders must ensure that patient information is secure and only shared when legally or ethically justified.
- Veracity: Promoting honesty and truth-telling in all interactions. Leaders are responsible for fostering a transparent environment where honesty prevails.
2. Legal Responsibilities in Nursing Leadership and Management
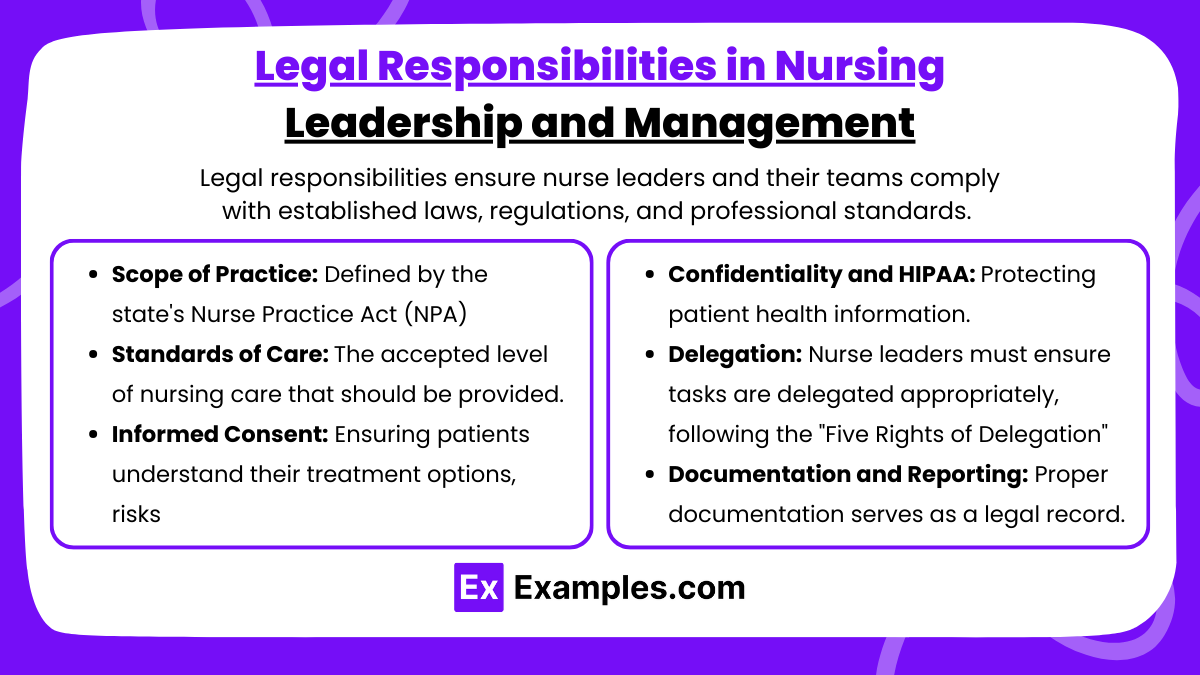
Legal responsibilities ensure nurse leaders and their teams comply with established laws, regulations, and professional standards. Legal principles help avoid negligence, malpractice, and professional liability.
Key Legal Responsibilities
- Scope of Practice: Defined by the state’s Nurse Practice Act (NPA), outlining what tasks PNs can and cannot perform. Nurse managers ensure staff follow the correct scope of practice.
- Standards of Care: The accepted level of nursing care that should be provided. Nurse leaders must ensure that nurses meet these standards to avoid negligence claims.
- Informed Consent: Ensuring patients understand their treatment options, risks, and benefits before giving permission. Nurse leaders ensure informed consent is obtained properly.
- Confidentiality and HIPAA: Protecting patient health information. Nurse leaders must educate staff about the importance of protecting patient privacy to avoid legal penalties.
- Delegation: Nurse leaders must ensure tasks are delegated appropriately, following the “Five Rights of Delegation” (right task, person, communication, circumstance, supervision).
- Documentation and Reporting: Proper documentation serves as a legal record. Leaders ensure nurses accurately document patient care and report issues such as abuse or unsafe practices.
3. Ethical and Legal Issues in Nursing Practice
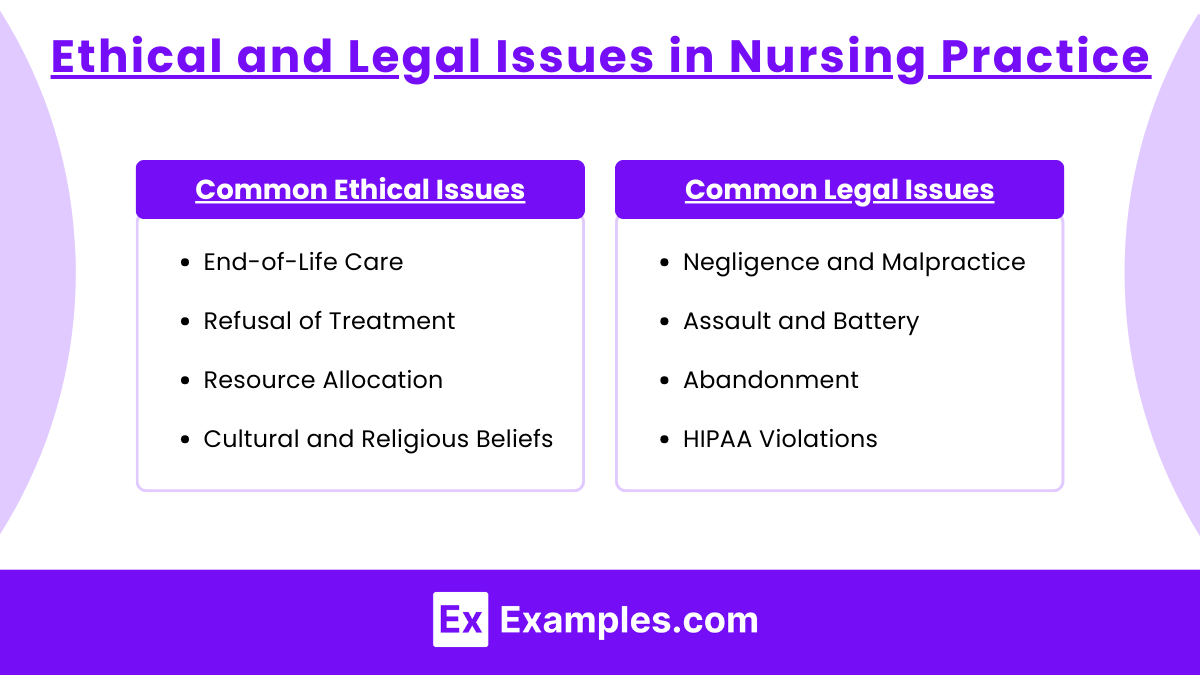
Nurses face ethical and legal challenges daily. Ethical issues focus on moral dilemmas, while legal issues arise from violations of state, federal, or organizational policies.
Common Ethical Issues
- End-of-Life Care: End-of-life care is one of the most complex ethical dilemmas nurses face. Patients may have advanced directives, which outline their preferences for life-sustaining treatment, and nurses must honor them. In addition, nurses encounter DNR (Do Not Resuscitate) orders, requiring them to withhold resuscitation efforts.
- Refusal of Treatment: Patients have the legal and ethical right to refuse treatment, even if it may negatively impact their health or lead to death. Nurses must ensure that patients are fully informed of the risks, benefits, and consequences of refusing care. While patients can refuse treatment, nurses must document their decision and continue providing care and support. Patients have the right to refuse treatment, but nurses must ensure the patient is fully informed.
- Resource Allocation: During emergencies or pandemics, limited healthcare resources (like ventilators, ICU beds, and medications) present an ethical dilemma. Nurse leaders may face the challenge of allocating resources fairly and equitably among patients with different care needs. Resource allocation is closely tied to the ethical principle of justice, which requires fair and equal treatment of all patients. Limited resources, such as ventilators, force nurse leaders to decide who receives care first.
- Cultural and Religious Beliefs: Patients’ cultural and religious beliefs can significantly influence the care they seek and the decisions they make. Ethical issues may arise when cultural or religious practices conflict with standard medical care or treatment protocols. For example, some patients may refuse blood transfusions due to religious beliefs.
Common Legal Issues
- Negligence and Malpractice: Failure to meet standards of care can lead to negligence or malpractice claims. Nurse leaders must ensure staff adhere to safety protocols. Negligence occurs when a nurse fails to provide the standard of care expected in a given situation, while malpractice refers to acts of negligence that result in harm to the patient. These claims arise when nurses fail to perform their duties competently.
- Assault and Battery: Unauthorized touching of a patient may lead to assault/battery claims. Nurse leaders ensure proper procedures for consent and avoid coercive tactics. Assault occurs when a nurse threatens to cause harm to a patient, while battery occurs when physical contact is made without the patient’s consent. Nurses must obtain informed consent before any invasive procedures.
- Abandonment: Leaving patients unattended is a form of patient abandonment. Leaders must ensure proper nurse-patient assignments and prevent staffing shortages. Patient abandonment occurs when a nurse leaves a patient under their care without proper handoff or communication to another provider. This can happen if a nurse walks away from a shift or fails to notify other nurses when leaving their unit.
- HIPAA Violations (Patient Confidentiality): The Health Insurance Portability and Accountability Act (HIPAA) ensures the protection of patient health information. Nurses must keep patient information confidential and avoid sharing it with unauthorized individuals.
Examples
Example 1: Ensuring Patient Autonomy in Care Decisions
A practical nurse (PN) is caring for a terminally ill patient who refuses further treatment. The nurse informs the healthcare team and advocates for the patient’s right to refuse care, even if family members or the healthcare team disagree. This demonstrates the ethical principle of autonomy and legal responsibility to honor the patient’s informed decision.
Example 2: Maintaining Patient Confidentiality (HIPAA Compliance)
A nurse is discussing a patient’s medical condition in a public hallway where others can overhear. The nurse manager intervenes, reminding the nurse of HIPAA privacy rules and providing training on maintaining confidentiality. This scenario highlights the legal obligation to protect patient privacy and the ethical principle of fidelity, which ensures loyalty and confidentiality in patient care.
Example 3: Addressing End-of-Life Ethical Dilemmas
A patient has a DNR (Do Not Resuscitate) order, but a family member insists on performing CPR during a cardiac arrest. The nurse follows the patient’s DNR order, advocating for the patient’s previously expressed wishes. This situation reflects the nurse’s ethical responsibility to uphold the principle of beneficence (acting in the patient’s best interest) and the legal duty to comply with advanced directives.
Example 4: Proper Delegation of Nursing Tasks
A nurse manager assigns a nursing assistant to measure and record a patient’s vital signs. Later, the nurse learns the assistant failed to record the blood pressure. The nurse leader addresses the situation, reminding the team of the Five Rights of Delegation (right task, right circumstance, right person, right direction/communication, and right supervision). This situation reflects the nurse manager’s legal obligation to ensure proper task delegation and accountability for safe care.
Example 5: Handling Workplace Negligence and Malpractice
A nurse forgets to administer a prescribed medication, leading to a patient’s adverse reaction. The nurse manager investigates, files an incident report, and provides corrective education to the nurse. This situation addresses the legal aspect of malpractice (failure to meet standards of care) and highlights the nurse leader’s role in ensuring quality care, risk management, and staff accountability.
Practice Questions
Question 1
A nurse is caring for a terminally ill patient who refuses further treatment. The patient states, “I just want to live my final days in peace without any more hospital visits.” Which ethical principle is the nurse demonstrating by honoring the patient’s request?
A. Beneficence
B. Autonomy
C. Justice
D. Nonmaleficence
Answer: B. Autonomy
Explanation:
- Autonomy refers to respecting the patient’s right to make their own decisions about their care and treatment. By honoring the patient’s request to stop treatment, the nurse supports the patient’s independence and decision-making rights.
- Beneficence (Option A) is about promoting the well-being of the patient, but in this case, beneficence could conflict with the patient’s right to autonomy.
- Justice (Option C) involves fairness and equity in care, which is unrelated to this scenario.
- Nonmaleficence (Option D) means “do no harm,” and while stopping treatment may prevent harm, this situation centers on honoring patient choice, which aligns with autonomy.
Question 2
A practical nurse (PN) is assigned to care for four patients. Which of the following tasks is outside the PN’s scope of practice, according to most Nurse Practice Acts (NPA)?
A. Administering oral and subcutaneous medications
B. Initiating blood transfusion therapy
C. Collecting data for a patient’s care plan
D. Providing patient education on medication side effects
Answer: B. Initiating blood transfusion therapy
Explanation:
- Initiating blood transfusions is generally outside the scope of practice for PNs, as it requires an RN’s supervision and involves assessing for transfusion reactions. While PNs can monitor patients during a transfusion, they typically cannot initiate it.
- Administering medications (Option A), like oral and subcutaneous drugs, is within the PN’s scope of practice.
- Data collection (Option C) is part of a PN’s role in the nursing process, although they do not create or modify care plans.
- Patient education (Option D) on medication side effects is within the PN’s role, as long as it involves reinforcement of information provided by an RN or healthcare provider.
Question 3
A nurse notices that a co-worker is repeatedly failing to document medication administration in patient charts. The nurse reports this to the unit manager. Which ethical and legal obligation is the nurse fulfilling?
A. Advocacy
B. Confidentiality
C. Duty to Report
D. Informed Consent
Answer: C. Duty to Report
Explanation:
- Duty to report means that nurses have a legal obligation to report unsafe, unethical, or illegal practices that jeopardize patient safety. By reporting the co-worker’s failure to document medication administration, the nurse is fulfilling this duty.
- Advocacy (Option A) involves supporting patient rights, but this situation is more focused on the nurse’s responsibility to report unsafe practices.
- Confidentiality (Option B) refers to safeguarding patient information, which is unrelated to reporting a nurse’s failure to document.
- Informed Consent (Option D) pertains to patient permission for procedures and treatment, which is irrelevant in this context.