Preparing for the NCLEX PN® Exam requires a thorough understanding of the gastrointestinal system and nutrition. Mastery of digestive anatomy, nutrient absorption, metabolic pathways, and dietary needs is essential. This knowledge supports effective care planning, management of gastrointestinal disorders, and promotion of patient health, crucial for achieving success on the exam.
Learning Objectives
In studying “Gastrointestinal/Nutrition” for the NCLEX PN® Exam, you should learn to understand the structure and function of the gastrointestinal system, including processes of digestion, absorption, and elimination. Analyze nutritional requirements across the lifespan, recognize the impact of dietary choices on health, and evaluate conditions affecting gastrointestinal function, such as GERD, ulcers, and malabsorption disorders. Explore interventions like enteral and parenteral nutrition, therapeutic diets, and management of feeding tubes. Apply your understanding to assess gastrointestinal health, identify signs of nutritional deficiencies, and interpret diagnostic results to provide safe, effective nursing care in diverse clinical scenarios.
Management of Dehydration, Electrolyte Imbalances, and Malnutrition
1. Dehydration Management
- Assessment: Monitor for signs such as dry mucous membranes, decreased skin turgor, and low urine output.
- Rehydration Therapy: Use oral rehydration solutions (ORS) for mild to moderate cases; initiate intravenous (IV) fluids (e.g., normal saline or Ringer’s lactate) for severe dehydration.
- Monitoring: Track urine output, vital signs, and laboratory values (e.g., blood urea nitrogen, creatinine) to assess hydration status.
- Prevention: Educate on adequate fluid intake, especially during illness, exercise, or high heat exposure.
2. Management of Electrolyte Imbalances
- Assessment: Identify specific imbalances through clinical signs and laboratory results (e.g., sodium, potassium, calcium levels).
- Intervention:
- Hyponatremia: Restrict water intake and administer hypertonic saline if symptomatic.
- Hyperkalemia: Use calcium gluconate, insulin with glucose, or sodium bicarbonate to stabilize cardiac function and shift potassium intracellularly. Consider dialysis if severe.
- Hypokalemia: Administer oral or IV potassium supplements carefully.
- Hypocalcemia: Provide calcium gluconate or calcium carbonate supplements.
- Monitoring: Regularly check electrolyte levels and ECG for cardiac effects.
3. Malnutrition Management
- Assessment: Screen for malnutrition using tools like the Malnutrition Universal Screening Tool (MUST). Measure weight, BMI, and serum albumin levels.
- Nutritional Support:
- Mild Cases: Encourage nutrient-rich, balanced meals and use oral nutritional supplements if needed.
- Moderate to Severe Cases: Implement enteral feeding via nasogastric or gastrostomy tubes. Consider parenteral nutrition if enteral feeding is not feasible.
- Micronutrient Supplementation: Address specific deficiencies (e.g., iron for anemia, vitamin D for bone health).
- Monitoring and Follow-Up: Track weight gain, dietary intake, and improvement in clinical symptoms.
Diagnostic Tests and Their Interpretation
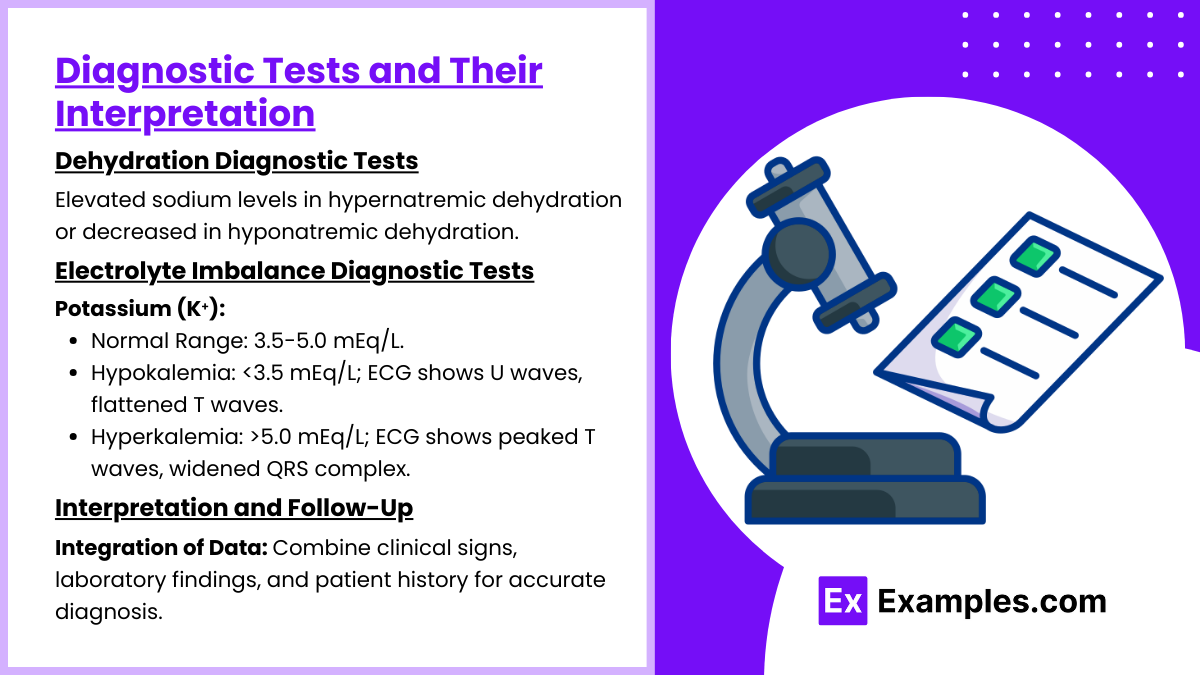
1. Dehydration Diagnostic Tests
- Clinical Assessment:
- Signs: Dry mucous membranes, decreased skin turgor, and oliguria.
- Vital Signs: Hypotension and tachycardia indicating hypovolemia.
- Laboratory Tests:
- Serum Electrolytes: Elevated sodium levels in hypernatremic dehydration or decreased in hyponatremic dehydration.
- Blood Urea Nitrogen (BUN): Elevated BUN-to-creatinine ratio (>20:1) suggests dehydration.
- Urine Specific Gravity: Increased (>1.030) indicates concentrated urine due to fluid deficit.
2. Electrolyte Imbalance Diagnostic Tests
- Sodium (Na⁺):
- Normal Range: 135-145 mEq/L.
- Hyponatremia: <135 mEq/L; symptoms include confusion, seizures, or coma.
- Hypernatremia: >145 mEq/L; symptoms include thirst, weakness, or altered mental status.
- Potassium (K⁺):
- Normal Range: 3.5-5.0 mEq/L.
- Hypokalemia: <3.5 mEq/L; ECG shows U waves, flattened T waves.
- Hyperkalemia: >5.0 mEq/L; ECG shows peaked T waves, widened QRS complex.
- Calcium (Ca²⁺):
- Normal Range: 8.5-10.5 mg/dL.
- Hypocalcemia: <8.5 mg/dL; signs include Chvostek’s and Trousseau’s signs.
- Hypercalcemia: >10.5 mg/dL; symptoms include nausea, vomiting, and confusion.
- Magnesium (Mg²⁺):
- Normal Range: 1.5-2.5 mEq/L.
- Hypomagnesemia: <1.5 mEq/L; signs include muscle cramps and arrhythmias.
- Hypermagnesemia: >2.5 mEq/L; symptoms include lethargy and bradycardia.
3. Interpretation and Follow-Up
- Integration of Data: Combine clinical signs, laboratory findings, and patient history for accurate diagnosis.
- Trend Monitoring: Reassess laboratory values and physical signs post-treatment to evaluate improvement.
- Differentiation: Use patterns of abnormalities to distinguish between conditions (e.g., hypernatremia due to dehydration vs. diabetes insipidus).
Common Gastrointestinal (GI) Disorders
Gastrointestinal (GI) disorders encompass a range of conditions affecting the digestive tract, which includes the esophagus, stomach, intestines, liver, pancreas, and gallbladder. These conditions can vary in severity from mild and self-limiting to chronic and life-threatening.
1. Gastroesophageal Reflux Disease (GERD)
- Description: Chronic condition where stomach acid flows back into the esophagus, causing irritation.
- Symptoms: Heartburn, regurgitation, chest pain, difficulty swallowing.
- Causes: Weakened lower esophageal sphincter (LES), obesity, smoking, certain foods (e.g., caffeine, spicy foods).
- Management:
- Lifestyle Changes: Weight loss, elevating the head of the bed, avoiding trigger foods.
- Medications: Proton pump inhibitors (PPIs), H2 blockers, antacids.
- Surgery: Fundoplication in severe cases.
2. Irritable Bowel Syndrome (IBS)
- Description: Functional GI disorder affecting the large intestine, with no identifiable structural cause.
- Symptoms: Abdominal pain, bloating, diarrhea, constipation, or alternating bowel habits.
- Causes: Stress, diet, gut-brain axis dysfunction, food intolerances.
- Management:
- Dietary Modifications: Low FODMAP diet, fiber supplementation.
- Medications: Antispasmodics, laxatives, antidiarrheals, probiotics.
- Behavioral Therapy: Stress management, cognitive behavioral therapy.
3. Peptic Ulcer Disease (PUD)
- Description: Open sores in the lining of the stomach or duodenum caused by acid erosion.
- Symptoms: Epigastric pain, nausea, bloating, bleeding (evidenced by melena or hematemesis).
- Causes: Helicobacter pylori infection, long-term NSAID use, smoking.
- Management:
- Medications: Antibiotics for H. pylori, PPIs, antacids.
- Lifestyle Changes: Avoid NSAIDs, alcohol, and smoking.
- Surgical Intervention: Rare, for complications like perforation or severe bleeding.
4. Inflammatory Bowel Disease (IBD)
- Description: Chronic inflammation of the GI tract, primarily Crohn’s disease and ulcerative colitis.
- Symptoms: Diarrhea, abdominal pain, weight loss, fatigue, bloody stools (more common in ulcerative colitis).
- Causes: Autoimmune response, genetic predisposition, environmental factors.
- Management:
- Medications: Aminosalicylates, corticosteroids, immunomodulators, biologics.
- Diet: Low-residue diet during flares, nutritional support.
- Surgery: Colectomy for ulcerative colitis; resection for Crohn’s complications.
5. Celiac Disease
- Description: Autoimmune reaction to gluten, damaging the small intestine’s villi.
- Symptoms: Diarrhea, weight loss, abdominal pain, bloating, malabsorption, anemia.
- Causes: Genetic predisposition, exposure to gluten (found in wheat, barley, rye).
- Management:
- Gluten-Free Diet: Avoid all sources of gluten.
- Nutritional Support: Supplement deficiencies (iron, calcium, vitamin D, B12).
- Monitoring: Regular follow-up for symptoms and nutrient levels.
Examples
Example 1: Gastroesophageal Reflux Disease (GERD)
A patient complaining of heartburn after eating spicy food, requiring dietary adjustments and lifestyle modifications.
Example 2: Peptic Ulcer Disease
A patient experiencing epigastric pain relieved by eating or taking antacids, requiring education on avoiding NSAIDs and alcohol.
Example 3: Irritable Bowel Syndrome (IBS)
A patient reporting alternating diarrhea and constipation, needing guidance on high-fiber diets and stress management techniques.
Example 4: Nausea and Vomiting
A post-operative patient experiencing nausea, requiring interventions such as antiemetics and clear liquid diets to manage symptoms.
Example 5: Constipation
A patient with reduced bowel movements due to immobility, requiring increased fluid intake, dietary fiber, and possibly stool softeners.
Practice Questions
Question 1
A client with a history of peptic ulcer disease presents with abdominal pain and dark, tarry stools. Which nursing intervention is the priority?
A. Administer prescribed antacids.
B. Monitor for signs of hypovolemic shock.
C. Encourage the client to increase dietary fiber.
D. Teach the client about smoking cessation.
Answer:
B. Monitor for signs of hypovolemic shock.
Explanation: Dark, tarry stools (melena) indicate upper gastrointestinal bleeding. The nurse’s priority is to assess and monitor for hypovolemic shock caused by blood loss. Administering antacids, increasing dietary fiber, and smoking cessation are important but are not immediate priorities in this situation.
Question 2
A nurse is teaching a client about managing gastroesophageal reflux disease (GERD). Which instruction should the nurse include?
A. “Eat three large meals daily to reduce gastric acid production.”
B. “Elevate the head of your bed by 6–8 inches during sleep.”
C. “Lie down immediately after eating to facilitate digestion.”
D. “Drink citrus juices to neutralize stomach acid.”
Answer:
B. Elevate the head of your bed by 6–8 inches during sleep.
Explanation: Elevating the head of the bed helps reduce reflux by preventing stomach acid from flowing back into the esophagus. The other options are incorrect as they worsen GERD symptoms.
Question 3
A client with cirrhosis is experiencing ascites. Which dietary recommendation should the nurse reinforce?
A. Increase protein intake.
B. Restrict sodium intake.
C. Encourage high-calorie snacks.
D. Restrict fluid intake to 1,000 mL/day.
Answer:
B. Restrict sodium intake.
Explanation: Sodium restriction is essential to reduce fluid retention associated with ascites. Fluid restriction may be needed, but sodium restriction takes precedence. Protein intake may vary based on the presence of hepatic encephalopathy.