Preparing for the NCLEX PN® Exam requires a thorough understanding of hematological and oncological systems, key components of nursing care. Mastery of blood cell functions, cancer pathophysiology, and treatment modalities is essential. This knowledge aids in managing blood disorders and providing oncological care, crucial for patient recovery and quality of life.
Learning Objective
In studying "Hematological/Oncological" for the NCLEX PN® Exam, you should aim to understand the structure and function of the hematological system, including the types and functions of blood cells, and the pathophysiology of common blood disorders. Learn to identify and manage oncological conditions, understanding cancer development, progression, and treatment options. Evaluate diagnostic tests like CBC, bone marrow biopsy, and tumor markers. Additionally, explore the implications of chemotherapy, radiation, and surgical interventions, and apply this knowledge to care planning and symptom management in clinical scenarios, ensuring comprehensive patient care in hematological and oncological settings.
Hematology: Understanding Blood and Blood Disorders
Hematology is the branch of medicine that focuses on the study, diagnosis, treatment, and prevention of diseases related to the blood. It encompasses the understanding of blood components, their functions, and the various disorders that can affect these components. Below is an overview of the key concepts in hematology, including the components of blood and common blood disorders.
Components of Blood
Red Blood Cells (RBCs):
Function: Carry oxygen from the lungs to the body's tissues and return carbon dioxide from the tissues back to the lungs.
Hemoglobin: Protein in RBCs that binds oxygen.
White Blood Cells (WBCs):
Function: Part of the immune system; different types of WBCs (such as neutrophils, lymphocytes, monocytes, eosinophils, and basophils) play roles in protecting the body against infection and disease.
Platelets:
Function: Essential for blood clotting and wound healing. They aggregate at sites of injury, forming a plug to prevent blood loss.
Plasma:
Function: The liquid component of blood in which blood cells are suspended. Plasma contains water, salts, enzymes, antibodies, and other proteins.
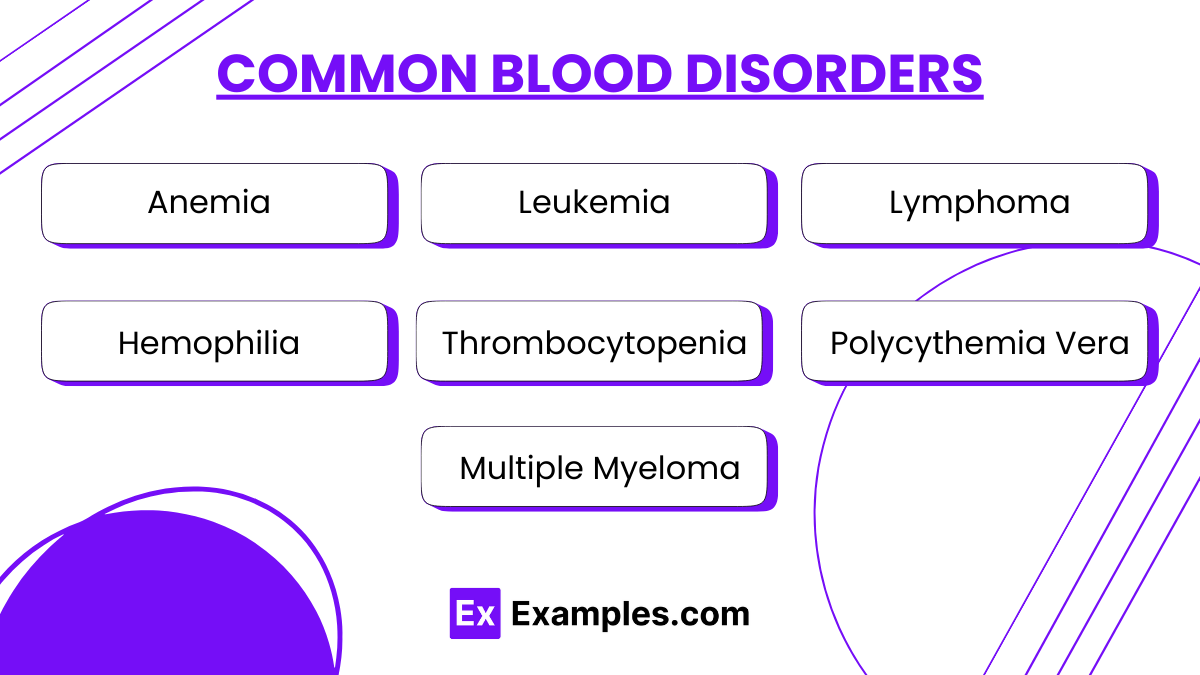
Common Blood Disorders
Anemia:
Description: A condition in which there is a deficiency of red blood cells or hemoglobin, leading to fatigue, weakness, and shortness of breath.
Types: Iron-deficiency anemia, sickle cell anemia, thalassemia, pernicious anemia, etc.
Leukemia:
Description: A type of cancer that affects the bone marrow and leads to the overproduction of abnormal white blood cells.
Types: Acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), chronic myeloid leukemia (CML), chronic lymphocytic leukemia (CLL).
Lymphoma:
Description: Cancer that begins in lymphocytes (a type of white blood cell) and affects the lymphatic system.
Types: Hodgkin's lymphoma and non-Hodgkin's lymphoma.
Hemophilia:
Description: A genetic disorder where the blood does not clot properly, leading to excessive bleeding and easy bruising.
Types: Hemophilia A (factor VIII deficiency) and Hemophilia B (factor IX deficiency).
Thrombocytopenia:
Description: A condition characterized by a low platelet count, which can lead to easy bruising and excessive bleeding from even minor wounds.
Polycythemia Vera:
Description: A disorder in which the bone marrow produces too many red blood cells, thickening the blood and increasing the risk of thrombosis.
Multiple Myeloma:
Description: Cancer of plasma cells which produce abnormal antibodies that can lead to kidney problems and weakened bones.
Oncology: Understanding Cancer
Oncology is the branch of medicine dedicated to the study, diagnosis, treatment, and prevention of cancer. Cancer is a group of diseases characterized by the uncontrolled growth and spread of abnormal cells. If not controlled, cancer can lead to death. Below is an overview of the fundamental aspects of cancer and its management.
Understanding Cancer
Carcinogenesis Process: Involves initiation (mutation in DNA), promotion (mutated cells proliferate), and progression (further mutations lead to malignant traits like invasiveness).
Types of Cancer: Named after the tissue or organ of origin, such as carcinomas (organs), sarcomas (connective tissues), lymphomas (lymphatic system), and leukemias (blood cells).
Grading and Staging: Grading assesses how much cancer cells differ from healthy cells; staging determines the size and spread of cancer, crucial for treatment planning.
Nursing Care in Hematology and Oncology
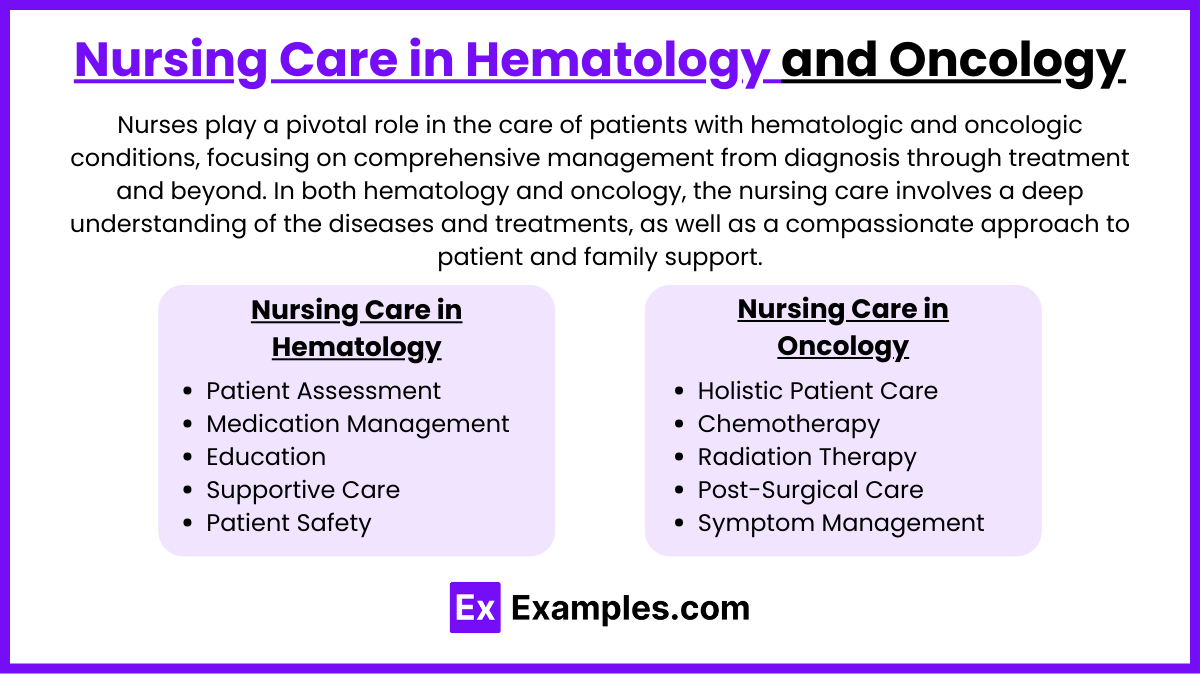
Nurses play a pivotal role in the care of patients with hematologic and oncologic conditions, focusing on comprehensive management from diagnosis through treatment and beyond. In both hematology and oncology, the nursing care involves a deep understanding of the diseases and treatments, as well as a compassionate approach to patient and family support. Here’s an overview of the specific roles and responsibilities of nurses in these fields:
Nursing Care in Hematology
Patient Assessment: Nurses assess patients for symptoms of hematologic disorders such as anemia, bleeding disorders, and blood cancers. This includes monitoring vital signs, blood counts, and other laboratory results to evaluate disease progression or response to treatment.
Medication Management: Administering prescribed medications including chemotherapy, blood transfusions, and growth factors. Nurses also manage side effects and complications from these medications.
Education: Nurses provide patient and family education on disease processes, treatment plans, and potential side effects. They teach about the importance of nutrition, infection prevention, and when to seek medical help for specific symptoms.
Supportive Care: Managing symptoms such as fatigue, pain, and nausea. This includes collaborating with other healthcare professionals to provide comprehensive care, such as dietitians for nutritional support or counselors for emotional support.
Patient Safety: Ensuring the safe handling and administration of chemotherapeutic agents and monitoring for adverse reactions during infusions.
Nursing Care in Oncology
Holistic Patient Care: Nurses in oncology provide care that addresses the physical, emotional, psychological, and social needs of patients. They support patients through the diagnosis, treatment, and survivorship stages, or provide palliative care at end-of-life stages.
Chemotherapy Administration: One of the primary roles of oncology nurses is the preparation and administration of chemotherapy. They must follow strict protocols to ensure safety and effectiveness, including verifying dosages and monitoring for immediate adverse effects.
Radiation Therapy Support: Nurses manage the care of patients receiving radiation therapy, monitoring for side effects, and providing skin care and other supportive measures to minimize discomfort.
Post-Surgical Care: For patients undergoing surgery as part of cancer treatment, oncology nurses manage postoperative care, pain control, wound care, and monitor for complications.
Pain and Symptom Management: Effective management of pain and other debilitating symptoms of cancer and its treatment, using both pharmacologic and non-pharmacologic methods.
Examples
Example 1: Management of Iron Deficiency Anemia
A patient presents with fatigue, pallor, and dizziness. Diagnosed with iron deficiency anemia, the nurse administers oral iron supplements and educates the patient on consuming iron-rich foods like red meat, leafy greens, and fortified cereals. The nurse also monitors for constipation, a common side effect of iron therapy.
Example 2: Care for a Patient with Acute Myelogenous Leukemia (AML)
A newly diagnosed AML patient begins chemotherapy. The nurse manages cytotoxic precautions, monitors for signs of infection due to neutropenia, and educates the patient on recognizing symptoms of bleeding. Emotional support is provided, along with coordination with social services for additional resources.
Example 3: Support for a Patient Undergoing Radiation Therapy for Breast Cancer
A patient receiving radiation therapy for breast cancer experiences skin irritation and fatigue. The nurse provides skin care instructions, advises on gentle cleansing and use of non-irritating moisturizers, and manages fatigue through scheduling rest periods and energy-conserving strategies.
Example 4: Postoperative Care for a Patient After Colon Cancer Surgery
Post-surgery, the nurse monitors the patient for signs of infection at the incision site, manages pain, and assists with early mobilization. The nurse also provides stoma care education if a colostomy was performed, including how to clean and change the colostomy bag.
Example 5: End-of-Life Care for a Patient with Terminal Pancreatic Cancer
For a patient in the terminal stages of pancreatic cancer, the nurse facilitates discussions about advance care planning, administers prescribed pain medications to manage symptoms, and provides emotional support to the patient and family, ensuring comfort and dignity in the patient’s final days.
Practice Questions
Question 1
Which of the following is a common side effect of chemotherapy?
A. Hypertension
B. Hyperglycemia
C. Leukopenia
D. Hypercalcemia
Answer:
C. Leukopenia
Explanation:
Leukopenia, or a decrease in white blood cell count, is a common side effect of chemotherapy, which affects the bone marrow's ability to produce blood cells. This condition increases the patient's risk of infection. Hypertension (option A) and hyperglycemia (option B) are typically not direct side effects of chemotherapy, while hypercalcemia (option D) is generally associated with malignancy rather than treatment.
Question 2
A patient with thrombocytopenia would likely exhibit which of the following symptoms?
A. Prolonged bleeding
B. Frequent nosebleeds
C. Easy bruising
D. All of the above
Answer:
D. All of the above
Explanation:
Thrombocytopenia, a condition characterized by an abnormally low platelet count, can lead to prolonged bleeding, frequent nosebleeds, and easy bruising. Platelets are crucial for blood clotting, and their deficiency impedes the body's ability to stop bleeding effectively.
Question 3
Which diagnostic test is most commonly used to evaluate the extent and spread of lymphoma?
A. X-ray
B. Ultrasound
C. Complete blood count (CBC)
D. Positron Emission Tomography (PET) scan
Answer:
D. Positron Emission Tomography (PET) scan
Explanation:
A Positron Emission Tomography (PET) scan is commonly used to evaluate the extent and spread of cancers such as lymphoma. It provides detailed images and can detect cancerous cells based on their activity levels, making it a valuable tool for staging cancer and assessing treatment response. While CBC (option C) can indicate hematological abnormalities, it does not provide information on cancer spread, which is critical for lymphoma management.