Preparing for the NCLEX PN® Exam requires a thorough understanding of the immune system, a fundamental component of nursing care. Mastery of immune responses, lymphatic structures, and common immunopathologies is essential. This knowledge aids in managing autoimmune diseases, infections, and allergic reactions, crucial for patient health and safety.
Learning Objective
In studying "Immune" for the NCLEX PN® Exam, you should aim to understand the structure and function of the immune system, including innate and adaptive immunity mechanisms. Learn to identify the roles of major cells like lymphocytes and phagocytes, and the biochemical pathways of immune responses. Evaluate common immunological tests and vaccinations, and their clinical relevance. Additionally, explore how autoimmune disorders, immunodeficiencies, and hypersensitivity reactions affect body systems, and apply this knowledge to manage and educate patients about prevention and treatment of infections, and the importance of immunizations in healthcare settings.
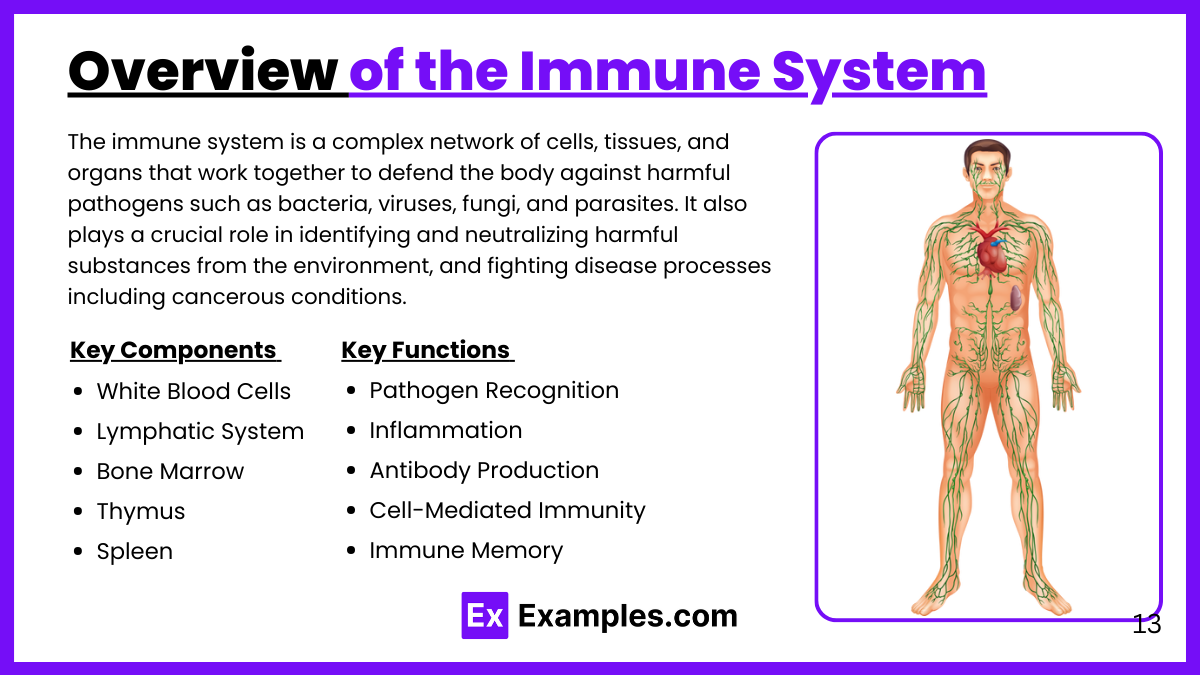
Overview of the Immune System
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens such as bacteria, viruses, fungi, and parasites. It also plays a crucial role in identifying and neutralizing harmful substances from the environment, and fighting disease processes including cancerous conditions. Here’s a detailed overview of the key components and functions of the immune system:
Key Components of the Immune System
White Blood Cells (Leukocytes):
Primary defenders against infection.
Types include lymphocytes (B cells and T cells), neutrophils, eosinophils, basophils, and monocytes.
Lymphatic System:
Network of vessels, nodes, and organs (including the thymus, spleen, and tonsils).
Transports lymph fluid, nutrients, and waste material between bodily tissues and the bloodstream.
Bone Marrow:
Soft tissue in the hollow center of bones.
Site of white blood cell production.
Thymus:
Gland where T cells mature.
Vital for the development of immune competence in youth.
Spleen:
Filters blood, recycles old red blood cells, and stores white blood cells and platelets.
Plays a significant role in response to infection and immune surveillance.
Functions of the Immune System
Pathogen Recognition and Response:
Innate Immunity: First line of defense; non-specific. Includes physical barriers like skin and mucous membranes, chemical barriers such as stomach acid, and cellular defenses like macrophages and neutrophils.
Adaptive Immunity: Specific response involving recognition of antigens by B cells and T cells. B cells produce antibodies, while T cells destroy infected cells.
Inflammation:
Acute inflammation is a response to injury or infection, signaling the immune system to heal and repair damaged tissue, as well as defend against invaders.
Antibody Production:
B cells produce antibodies that specifically target antigens of pathogens. Antibodies neutralize or mark pathogens for destruction.
Cell-Mediated Immunity:
T cells recognize and destroy infected cells. Helper T cells assist in the immune response regulation and activation of other immune cells.
Immune Memory:
Following an infection or vaccination, the immune system remembers the pathogen. If the pathogen re-enters the body, the immune system can respond more rapidly and effectively.
Immunopathology
Immunopathology is the study of diseases caused by dysfunctions of the immune system. These dysfunctions can manifest as either an excessive immune response or an inadequate response, leading to a range of health issues. Immunopathology helps understand the pathogenic mechanisms, diagnosis, and treatment of immune-related disorders. Here’s an overview of the main categories and examples of disorders studied in immunopathology:
Categories of Immunopathological Diseases:
Hypersensitivity Reactions:
These occur when the immune system reacts excessively to an antigen, causing damage to the body's own tissues. Hypersensitivity reactions are classified into four types:
Type I: Immediate hypersensitivity (e.g., allergies to pollen, certain foods, and insect stings that can lead to anaphylaxis).
Type II: Antibody-dependent cytotoxic hypersensitivity (e.g., autoimmune hemolytic anemia, where antibodies target and destroy red blood cells).
Type III: Immune complex-mediated hypersensitivity (e.g., systemic lupus erythematosus, where immune complexes deposit in tissues, causing inflammation).
Type IV: Delayed-type hypersensitivity (e.g., contact dermatitis such as poison ivy reactions and chronic conditions like tuberculosis).
Autoimmune Diseases:
These occur when the immune system mistakenly attacks the body's own cells, tissues, or organs, failing to recognize them as self. Examples include:
Rheumatoid arthritis: Chronic inflammation of the joints.
Type 1 diabetes: Destruction of insulin-producing cells in the pancreas.
Multiple sclerosis: Immune-mediated destruction of the central nervous system's myelin sheath.
Immunodeficiency Disorders:
These arise from an inadequate immune response that leaves the body vulnerable to infections, malignancies, and other diseases. Immunodeficiencies can be congenital or acquired:
Primary immunodeficiencies: Genetic defects affecting immune cells (e.g., Severe Combined Immunodeficiency (SCID)).
Secondary immunodeficiencies: Caused by external factors (e.g., HIV/AIDS, which severely weakens the immune system).
Chronic Inflammation and Autoinflammatory Disorders:
Chronic inflammation is a prolonged inflammatory response that can lead to tissue damage and is often associated with non-infectious diseases.
Autoinflammatory disorders are characterized by recurrent episodes of inflammation without the high-titer autoantibodies or antigen-specific T cells typically seen in autoimmune diseases. Examples include familial Mediterranean fever and gout.
Diagnostic and Therapeutic Approaches in Immunology
Immunology, as a core aspect of understanding and managing diseases related to the immune system, employs a range of diagnostic and therapeutic approaches. These methods are designed to accurately diagnose immune disorders and provide effective treatments that can modulate immune responses and alleviate symptoms. Here’s an outline of the primary diagnostic and therapeutic strategies used in immunology:
Diagnostic Approaches in Immunology
Laboratory Tests:
Complete Blood Count (CBC), Immunophenotyping, Serological Tests, and Autoantibody Tests for assessing immune function and detecting disorders.
Cytokine and Chemokine Tests to measure inflammatory markers.
Genetic Testing:
Identifies genetic mutations linked to immunodeficiencies and autoimmune diseases.
Skin Tests:
Allergy Testing and Delayed-Type Hypersensitivity Testing for assessing allergic reactions and cellular immunity.
Functional Assays:
Evaluate the functionality of immune components such as complement activity and phagocyte function.
Therapeutic Approaches in Immunology
Pharmacotherapy:
Immunosuppressants (e.g., corticosteroids), Biologics (e.g., monoclonal antibodies), and Small Molecule Inhibitors to modulate immune responses.
Immunotherapy:
Includes Allergy Shots for desensitization and Cancer Immunotherapy (e.g., CAR-T cell therapy, checkpoint inhibitors) to enhance anti-cancer immunity.
Plasma and Immunoglobulin Therapies:
IVIG for immune deficiencies and autoimmune diseases, and Plasmapheresis for removing harmful antibodies.
Gene Therapy and Stem Cell Transplantation:
Used for correcting genetic defects in primary immunodeficiencies and replacing dysfunctional immune cells.
Examples
Example 1: Managing Rheumatoid Arthritis
A patient with rheumatoid arthritis is experiencing joint pain and swelling. The nurse administers prescribed NSAIDs and disease-modifying antirheumatic drugs (DMARDs), educates the patient on gentle exercises, and suggests heat and cold therapy to reduce symptoms and improve joint function.
Example 2: Care for a Patient with HIV/AIDS
For a patient diagnosed with HIV, the nurse manages antiretroviral therapy adherence, monitors for opportunistic infections, and provides nutritional counseling to boost immune function. Regular counseling and support groups are recommended to help the patient cope with the psychosocial aspects of the disease.
Example 3: Emergency Response to Anaphylaxis
A patient experiencing anaphylaxis following a bee sting is administered epinephrine immediately. The nurse monitors the patient’s respiratory and cardiovascular status closely, prepares for potential additional doses of epinephrine, and educates the patient and family on the use of epinephrine auto-injectors for future incidents.
Example 4: Managing Seasonal Allergies
A patient with severe seasonal allergies presents with rhinitis and itchy eyes. The nurse recommends and administers non-sedating antihistamines, advises the patient to avoid known allergens, and suggests the use of a high-efficiency particulate air (HEPA) filter at home to reduce allergen exposure.
Example 5: Tuberculosis Screening
A patient suspected of having tuberculosis is given a tuberculin skin test. The nurse administers the test, provides information on how and when to check the reaction, and prepares to manage a positive test, which would include referral for further diagnostic testing and discussion of treatment options.
Practice Questions
Question 1
Which of the following cells is primarily responsible for antibody production?
A. Macrophages
B. T lymphocytes
C. B lymphocytes
D. Natural killer cells
Answer:
C. B lymphocytes
Explanation:
B lymphocytes, or B cells, are primarily responsible for producing antibodies in the adaptive immune response. They recognize specific antigens and differentiate into plasma cells that secrete antibodies to neutralize or mark pathogens for destruction. Macrophages (option A) ingest and digest pathogens, T lymphocytes (option B) are involved in cell-mediated immunity, and Natural killer cells (option D) are part of innate immunity, responsible for killing virus-infected cells and tumor cells without prior sensitization.
Question 2
Which type of hypersensitivity reaction is associated with allergies such as hay fever and asthma?
A. Type I
B. Type II
C. Type III
D. Type IV
Answer:
A. Type I
Explanation:
Type I hypersensitivity reactions are immediate reactions mediated by IgE antibodies. This type of reaction typically involves common allergies such as hay fever, asthma, and anaphylaxis. These reactions occur when an allergen triggers the release of histamine and other chemicals from mast cells and basophils, leading to symptoms like sneezing, itching, and difficulty breathing. Type II involves cytotoxic reactions, Type III involves immune complex reactions, and Type IV involves delayed-type hypersensitivity mediated by T cells.
Question 3
What is the primary function of the complement system in immune defense?
A. To recognize and remember specific pathogens
B. To directly kill infected cells and cancer cells
C. To enhance the ability of antibodies and phagocytic cells to clear microbes and damaged cells
D. To regulate the production of antibodies by B cells
Answer:
C. To enhance the ability of antibodies and phagocytic cells to clear microbes and damaged cells
Explanation:
The complement system is a group of proteins that enhances (complements) the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism, promote inflammation, and attack the pathogen's cell membrane. It does not recognize or remember specific pathogens (option A), which is a function of adaptive immunity. While natural killer cells directly kill infected cells and cancer cells (option B), the complement system primarily assists in marking pathogens for destruction. It does not regulate antibody production (option D), which is controlled by interactions between B cells and helper T cells.