Preparing for the NCLEX PN® Exam requires a thorough understanding of the immune system, a vital component of patient care. Mastery of immune defense mechanisms, immune disorders, and infection control is essential. This knowledge aids in assessing immune function, managing diseases, and ensuring safety, critical for excelling in the exam.
Learning Objectives
In studying "Immune" for the NCLEX PN® Exam, you should learn to understand the structure and function of the immune system, including innate and adaptive immunity. Analyze how the body defends against pathogens, recognizes self from non-self, and responds to infections. Evaluate principles behind hypersensitivity reactions, autoimmune disorders, and immunodeficiency conditions. Additionally, explore clinical interventions such as vaccinations, immunosuppressive therapy, and patient education on preventing infections. Apply your understanding to assess immune responses, identify signs of immune-related disorders, and interpret laboratory results to provide safe, effective nursing care in diverse clinical scenarios.
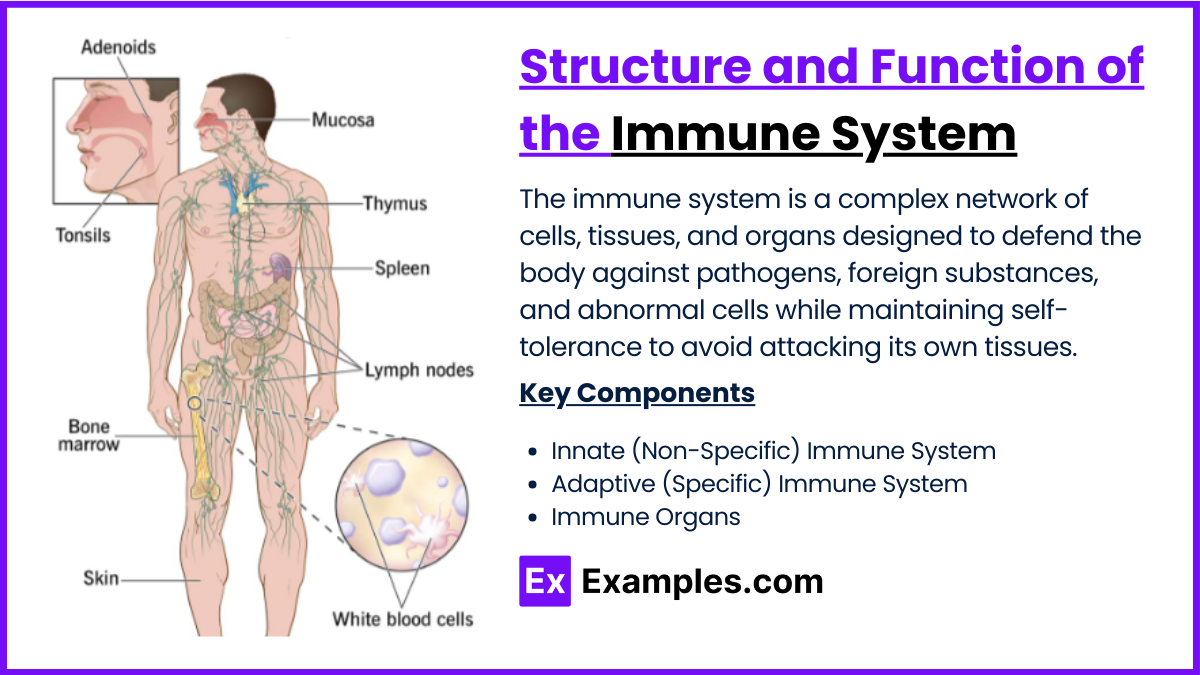
Structure and Function of the Immune System
The immune system is a complex network of cells, tissues, and organs designed to defend the body against pathogens, foreign substances, and abnormal cells while maintaining self-tolerance to avoid attacking its own tissues.
A. Innate (Non-Specific) Immune System
Physical Barriers:
Skin: Acts as a protective barrier against pathogens.
Mucous Membranes: Trap microbes in the respiratory, gastrointestinal, and urogenital tracts.
Chemical Barriers:
Enzymes: Lysozyme in tears and saliva destroys bacterial cell walls.
Acidic Environments: Stomach acid prevents pathogen survival.
Cellular Components:
Phagocytes: Engulf and destroy pathogens.
Neutrophils: First responders to infection.
Macrophages: Ingest and present antigens to adaptive immune cells.
Natural Killer (NK) Cells: Target virus-infected and cancerous cells.
Proteins:
Complement System: Enhances phagocytosis and lyses pathogens.
Cytokines: Signaling molecules that regulate immune responses.
B. Adaptive (Specific) Immune System
Lymphocytes:
B Cells: Produce antibodies and mediate humoral immunity.
T Cells: Mediate cellular immunity.
Helper T Cells (CD4+): Activate other immune cells.
Cytotoxic T Cells (CD8+): Destroy infected or abnormal cells.
Antibodies (Immunoglobulins):
Recognize and neutralize specific antigens.
Types include IgG, IgA, IgM, IgE, and IgD.
Memory Cells:
Retain antigen information for faster responses during future infections.
C. Immune Organs
Primary Organs:
Bone Marrow: Produces immune cells.
Thymus: Site of T-cell maturation.
Secondary Organs:
Lymph Nodes: Filter pathogens and activate lymphocytes.
Spleen: Filters blood and removes old red blood cells.
Mucosa-Associated Lymphoid Tissue (MALT): Protects mucosal surfaces.
Body's Defense Mechanisms
1. First Line of Defense: Physical and Chemical Barriers
The first line of defense consists of innate mechanisms that prevent pathogen entry into the body.
Physical Barriers:
Skin: Acts as a protective barrier, preventing microbial invasion.
Mucous Membranes: Line the respiratory, digestive, and genitourinary tracts, trapping pathogens in mucus.
Cilia: Hair-like structures in the respiratory tract that sweep mucus and trapped particles away from the lungs.
Chemical Barriers:
Lysozyme: Enzyme found in tears, saliva, and sweat that destroys bacterial cell walls.
Stomach Acid (HCl): Creates an acidic environment lethal to ingested pathogens.
Defensins: Antimicrobial peptides produced by epithelial cells.
Sebum and Sweat: Create an acidic pH on the skin that inhibits bacterial growth.
Microbial Barriers:
Normal Flora: Beneficial microorganisms on the skin and in the gut compete with pathogens, preventing their growth.
2. Second Line of Defense: Innate Immune Responses
When pathogens breach the first line of defense, innate immunity provides a nonspecific and rapid response.
Inflammatory Response:
Triggered by tissue injury or infection.
Symptoms: Redness, heat, swelling, pain, and loss of function.
Key Players:
Histamine: Released by mast cells; increases blood flow and capillary permeability.
Cytokines: Signal other immune cells to the site of infection.
Phagocytosis:
Specialized cells engulf and destroy pathogens.
Phagocytes: Include neutrophils, macrophages, and dendritic cells.
Natural Killer (NK) Cells:
Target and kill virus-infected and cancerous cells by inducing apoptosis.
Complement System:
A group of proteins that enhance phagocytosis, lyse pathogens, and promote inflammation.
Fever:
Elevated body temperature inhibits pathogen replication and enhances immune cell function.
Interferons:
Proteins released by virus-infected cells that alert neighboring cells to heighten their antiviral defenses.
3. Third Line of Defense: Adaptive Immune Responses
Adaptive immunity is specific to pathogens and provides long-lasting protection.
Humoral Immunity:
Mediated by B cells and antibodies.
Mechanism:
B cells recognize antigens and differentiate into plasma cells, producing antibodies.
Antibodies neutralize pathogens or mark them for destruction.
Cell-Mediated Immunity:
Mediated by T cells (Helper T cells and Cytotoxic T cells).
Mechanism:
Helper T cells (CD4+): Activate B cells, cytotoxic T cells, and macrophages.
Cytotoxic T cells (CD8+): Kill infected or abnormal cells directly.
Memory Cells:
Created after initial exposure to an antigen.
Allow faster and stronger responses upon re-exposure.
Hypersensitivity Reactions, Autoimmune Disorders, and Immunodeficiency
The immune system's ability to protect the body relies on balance and precision. When this balance is disrupted, it can lead to hypersensitivity reactions, autoimmune disorders, or immunodeficiency, each with distinct mechanisms and clinical implications.
1. Hypersensitivity Reactions
Hypersensitivity reactions are exaggerated or inappropriate immune responses to antigens, classified into four types based on their underlying mechanisms.
Type I (Immediate Hypersensitivity):
Mechanism: IgE antibodies bind to allergens, triggering mast cell degranulation and release of histamine.
Examples: Allergic rhinitis, asthma, anaphylaxis.
Symptoms: Hives, swelling, wheezing, anaphylactic shock (in severe cases).
Management: Avoid allergens, antihistamines, corticosteroids, epinephrine for anaphylaxis.
Type II (Cytotoxic Hypersensitivity):
Mechanism: IgG or IgM antibodies target cells, leading to complement activation and cell destruction.
Examples: Hemolytic anemia, Goodpasture syndrome, Rh incompatibility.
Symptoms: Tissue damage, hemolysis.
Management: Immunosuppressive therapy, plasma exchange.
Type III (Immune Complex-Mediated Hypersensitivity):
Mechanism: Antigen-antibody complexes deposit in tissues, causing inflammation via complement activation.
Examples: Systemic lupus erythematosus (SLE), serum sickness, post-streptococcal glomerulonephritis.
Symptoms: Fever, joint pain, kidney damage.
Management: Corticosteroids, plasmapheresis.
Type IV (Delayed-Type Hypersensitivity):
Mechanism: T-cell-mediated response leading to inflammation and tissue damage.
Examples: Contact dermatitis, tuberculosis (TB) skin test, transplant rejection.
Symptoms: Redness, swelling, granuloma formation.
Management: Immunomodulators, topical steroids.
2. Autoimmune Disorders
Autoimmune disorders occur when the immune system mistakenly attacks the body’s own tissues, failing to differentiate self from non-self.
Systemic Disorders:
Systemic Lupus Erythematosus (SLE): Affects multiple organs with symptoms like butterfly rash, joint pain, and kidney involvement.
Rheumatoid Arthritis (RA): Chronic inflammation of joints leading to pain and deformity.
Organ-Specific Disorders:
Type 1 Diabetes Mellitus: Destruction of insulin-producing pancreatic beta cells.
Hashimoto’s Thyroiditis: Immune-mediated destruction of the thyroid gland, causing hypothyroidism.
Multiple Sclerosis (MS): Immune attack on the central nervous system, leading to neurological symptoms.
Pathophysiology of Autoimmune Disorders
Genetic Predisposition: Involvement of HLA (human leukocyte antigen) genes.
Environmental Triggers: Infections, stress, or toxins.
Loss of Tolerance: Regulatory T cells fail to suppress autoreactive lymphocytes.
Management:
Immunosuppressive Therapy: Corticosteroids, methotrexate, or biologics.
Symptomatic Relief: NSAIDs, disease-modifying antirheumatic drugs (DMARDs).
Lifestyle Modifications: Stress reduction, balanced diet, physical therapy.
3. Immunodeficiency
Immunodeficiency is characterized by the partial or complete failure of the immune system, leading to recurrent infections and susceptibility to opportunistic pathogens.
Primary (Congenital) Immunodeficiency: Caused by genetic defects affecting immune system components.
Examples:
Severe Combined Immunodeficiency (SCID): Defective T and B cells.
X-Linked Agammaglobulinemia: Lack of mature B cells and antibodies.
Symptoms: Frequent infections, poor growth, failure to thrive.
Management: Bone marrow transplant, immunoglobulin replacement therapy.
Secondary (Acquired) Immunodeficiency:
Results from external factors like infections or treatments.
Examples:
HIV/AIDS: Destruction of CD4+ T cells by the human immunodeficiency virus.
Immunosuppression due to chemotherapy or organ transplantation.
Symptoms: Opportunistic infections (e.g., pneumocystis pneumonia, candidiasis), weight loss, fatigue.
Management: Antiretroviral therapy (for HIV), infection control, immune-boosting treatments.
Examples
Example 1: Anaphylaxis
A life-threatening allergic reaction causing airway swelling, low blood pressure, and rash; treated with epinephrine.
Example 2: HIV/AIDS
Immunodeficiency from HIV; monitor for opportunistic infections and emphasize antiretroviral therapy adherence.
Example 3: Lupus (SLE)
An autoimmune disease causing systemic inflammation; monitor for skin rash, joint pain, and kidney involvement.
Example 4: Rheumatoid Arthritis
Chronic autoimmune joint inflammation; manage pain and swelling with NSAIDs and DMARDs.
Example 5: Allergic Rhinitis
Immune response to allergens causing sneezing and congestion; manage with antihistamines and allergen avoidance.
Practice Questions
A client diagnosed with HIV is being educated on infection prevention. Which statement indicates the need for further teaching?
A. "I will avoid raw fruits and vegetables."
B. "I will wash my hands frequently."
C. "I will avoid crowded places when possible."
D. "I can safely receive live-virus vaccines."
D. I can safely receive live-virus vaccines.Answer:
D. I can safely receive live-virus vaccines.
Explanation: Clients with HIV, especially with low CD4 counts, should avoid live-virus vaccines because their immune system may not be able to handle the weakened virus. The other options indicate appropriate infection prevention strategies.
Question 2
A nurse is caring for a client with systemic lupus erythematosus (SLE). Which finding should the nurse report immediately?
A. Facial butterfly rash.
B. Joint pain and swelling.
C. Elevated temperature of 101°F (38.3°C).
D. Fatigue and weakness.
Answer:
C. Elevated temperature of 101°F (38.3°C).
Explanation: An elevated temperature may indicate an infection, which can be life-threatening in clients with SLE due to their compromised immune system. Other symptoms are common in SLE but not immediately life-threatening.
Question 3
A client receiving chemotherapy is at risk for neutropenia. Which instruction should the nurse include in discharge teaching?
A. "Avoid contact with pets and pet waste."
B. "Take acetaminophen for any fever over 100°F (37.8°C)."
C. "Increase fresh fruits and vegetables in your diet."
D. "Limit handwashing to prevent skin irritation."
Answer:
A. Avoid contact with pets and pet waste.
Explanation: Clients with neutropenia are at increased risk of infection, so they should avoid potential sources of pathogens, including pets and pet waste. Fevers should be reported to a healthcare provider, and fresh fruits and vegetables may carry bacteria.