Adult Health: Infectious Disease is a crucial component of the NCLEX-PN® exam, encompassing the understanding of various pathogens, their transmission, and the clinical manifestations of infections in adults. This topic covers key areas such as pathophysiology, prevention strategies, diagnosis, treatment protocols, and essential nursing interventions. Mastery of infectious diseases, including HIV/AIDS, tuberculosis, influenza, and pneumonia, ensures nurses can effectively manage patient care, implement infection control measures, and educate patients, thereby promoting optimal health outcomes and preventing disease spread.
Learning Objectives
In studying “Adult Health: Infectious Disease” for the NCLEX-PN® Exam, you should learn to understand the various types of infectious diseases affecting adults, including bacterial, viral, fungal, and parasitic infections. Analyze the pathophysiology, modes of transmission, clinical manifestations, and treatment protocols for each disease. Evaluate nursing considerations such as infection control measures, patient monitoring, medication administration, potential drug interactions, and safety precautions. Additionally, explore the clinical applications of these diseases in diagnosing and managing patient care, and apply your understanding to effectively respond to infectious disease-related scenarios and questions on the NCLEX-PN® exam.
Fundamentals of Infectious Diseases
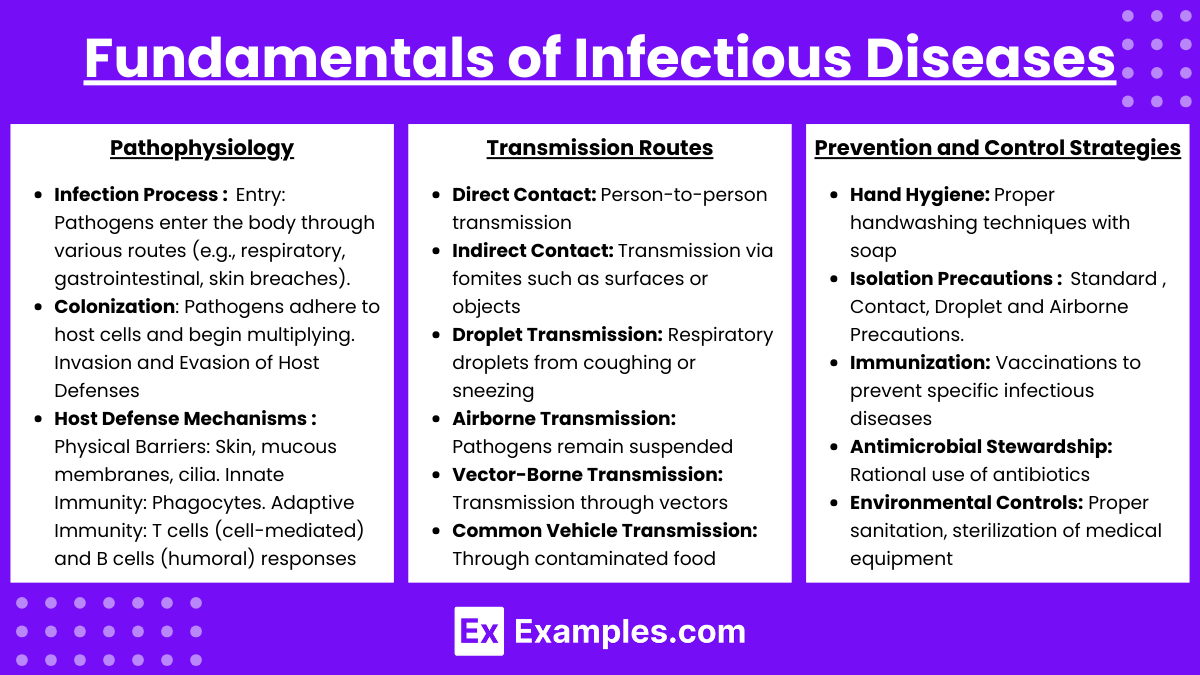
1. Pathophysiology
- Infection Process:
- Entry: Pathogens enter the body through various routes (e.g., respiratory, gastrointestinal, skin breaches).
- Colonization: Pathogens adhere to host cells and begin multiplying.
- Invasion: Pathogens penetrate deeper tissues, evading initial immune defenses.
- Evasion of Host Defenses: Mechanisms like antigenic variation, toxin production, and biofilm formation help pathogens survive.
- Host Defense Mechanisms:
- Physical Barriers: Skin, mucous membranes, cilia.
- Innate Immunity: Phagocytes (e.g., neutrophils, macrophages), natural killer cells, inflammatory response.
- Adaptive Immunity: T cells (cell-mediated) and B cells (humoral) responses, antibody production.
2. Transmission Routes
- Direct Contact: Person-to-person transmission (e.g., herpes simplex, COVID-19).
- Indirect Contact: Transmission via fomites such as surfaces or objects (e.g., influenza, norovirus).
- Droplet Transmission: Respiratory droplets from coughing or sneezing (e.g., tuberculosis, pertussis).
- Airborne Transmission: Pathogens remain suspended in the air for extended periods (e.g., measles, varicella).
- Vector-Borne Transmission: Transmission through vectors like mosquitoes or ticks (e.g., malaria, Lyme disease).
- Common Vehicle Transmission: Through contaminated food, water, or medical equipment (e.g., E. coli, hepatitis A).
3. Prevention and Control Strategies
- Hand Hygiene: Proper handwashing techniques with soap and water or using alcohol-based sanitizers.
- Isolation Precautions:
- Standard Precautions: Basic infection control measures for all patients.
- Contact Precautions: For infections spread by direct or indirect contact.
- Droplet Precautions: For diseases transmitted via respiratory droplets.
- Airborne Precautions: For highly contagious airborne diseases.
- Immunization: Vaccinations to prevent specific infectious diseases (e.g., influenza, pneumococcal vaccines, HPV).
- Antimicrobial Stewardship: Rational use of antibiotics and antivirals to minimize resistance.
- Environmental Controls: Proper sanitation, sterilization of medical equipment, and safe waste disposal.
- Patient Education: Informing patients about hygiene practices, vaccination importance, and recognizing symptoms.
Major Adult Infectious Diseases
1. (HIV)/Acquired Immunodeficiency Syndrome (AIDS)
- HIV is a retrovirus that targets CD4+ T cells, leading to AIDS when immune function is severely compromised.
- Etiology:
- Transmission: Unprotected sexual contact, contaminated needles, mother-to-child during birth or breastfeeding.
- Clinical Manifestations:
- Acute HIV Infection: Flu-like symptoms (fever, lymphadenopathy, rash).
- Chronic HIV Infection: Asymptomatic period that can last years.
- AIDS: Opportunistic infections (e.g., Pneumocystis jiroveci pneumonia), certain cancers (Kaposi sarcoma, non-Hodgkin lymphoma).
- Diagnosis:
- Tests: ELISA, Western blot, CD4 count, viral load assays.
- Treatment:
- Antiretroviral Therapy (ART): Combination of NRTIs, NNRTIs, PIs, integrase inhibitors to suppress viral replication.
- Nursing Considerations:
- Monitoring: Regular CD4 counts and viral load assessments.
- Adherence: Ensuring patients adhere to ART regimens to prevent resistance.
- Prevention: Educating on avoiding opportunistic infections and transmission prevention.
- Patient Teaching:
- Importance of medication adherence.
- Safe sex practices and avoiding needle sharing.
- Nutrition, lifestyle modifications, and mental health support.
2. Tuberculosis (TB)
- A contagious bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs.
- Etiology:
- Transmission: Airborne particles from an infected individual’s cough or sneeze.
- Clinical Manifestations:
- Chronic cough (sometimes with hemoptysis), night sweats, weight loss, fever, fatigue.
- Diagnosis:
- Tests: Tuberculin skin test (Mantoux), interferon-gamma release assays (IGRA), chest X-ray, sputum smear and culture.
- Treatment:
- First-Line Anti-TB Drugs: Isoniazid, Rifampin, Pyrazinamide, Ethambutol.
- Duration: Typically 6 months, with an initial intensive phase followed by a continuation phase.
- Nursing Considerations:
- Monitoring: Liver function tests due to potential hepatotoxicity from medications.
- Adherence: Ensuring patients complete the full course to prevent resistance.
- Isolation: Implementing airborne precautions to prevent spread.
- Patient Teaching:
- Importance of completing therapy even if symptoms improve.
- Reporting side effects promptly.
- Preventing transmission by covering mouth when coughing and ensuring good ventilation.
3. Influenza
- A highly contagious viral respiratory infection caused by influenza viruses (types A, B, and C).
- Etiology:
- Transmission: Respiratory droplets from infected individuals via coughing, sneezing, or talking.
- Clinical Manifestations:
- Sudden onset of fever, chills, myalgia, cough, sore throat, nasal congestion, fatigue.
- Diagnosis:
- Tests: Rapid influenza diagnostic tests (RIDTs), reverse transcription-polymerase chain reaction (RT-PCR).
- Treatment:
- Antiviral Agents: Oseltamivir (Tamiflu), Zanamivir (Relenza) effective when started within 48 hours of symptom onset.
- Supportive Care: Hydration, rest, antipyretics (e.g., acetaminophen, ibuprofen).
- Nursing Considerations:
- Early Treatment: Initiate antivirals promptly to reduce severity and duration.
- Isolation: Implement droplet precautions to prevent spread.
- Patient Teaching:
- Annual influenza vaccination as a preventive measure.
- Hand hygiene and respiratory etiquette (e.g., covering mouth when coughing).
- Recognizing signs of complications that require medical attention.
4. Pneumonia
- Inflammation of the alveoli, typically caused by infection, leading to impaired gas exchange.
- Etiology:
- Bacterial: Streptococcus pneumoniae (most common), Haemophilus influenzae, Staphylococcus aureus.
- Viral: Influenza virus, Respiratory syncytial virus (RSV).
- Fungal: Pneumocystis jiroveci, Histoplasma capsulatum (in immunocompromised individuals).
- Clinical Manifestations:
- Cough with sputum production, fever, chills, dyspnea, chest pain, rales or crackles on auscultation.
- Diagnosis:
- Tests: Chest X-ray, sputum culture and Gram stain, complete blood count (CBC), blood cultures.
- Treatment:
- Antibiotics: Based on the suspected or confirmed causative organism (e.g., Macrolides, Cephalosporins, Fluoroquinolones).
- Supportive Care: Oxygen therapy if hypoxemic, hydration, bronchodilators if needed.
- Nursing Considerations:
- Monitoring: Respiratory status, oxygen saturation, and response to treatment.
- Encouraging: Deep breathing exercises, coughing to promote expectoration, adequate hydration.
- Patient Teaching:
- Adherence to prescribed antibiotic regimen.
- Importance of completing the full course of antibiotics.
- Preventive measures such as vaccination (e.g., pneumococcal vaccine, influenza vaccine).
5. Sepsis
- A life-threatening organ dysfunction caused by a dysregulated host response to infection.
- Etiology:
- Can result from various infections, including pneumonia, urinary tract infections, abdominal infections, bloodstream infections.
- Clinical Manifestations:
- Early Signs: Fever or hypothermia, tachycardia, tachypnea, leukocytosis or leukopenia.
- Advanced Signs: Altered mental status, hypotension, decreased urine output, signs of organ dysfunction (e.g., acute kidney injury).
- Diagnosis:
- Criteria: Systemic Inflammatory Response Syndrome (SIRS) criteria plus evidence of infection.
- Tests: Blood cultures, lactate levels, imaging studies to identify infection source, complete metabolic panel.
- Treatment:
- Immediate Actions: Prompt administration of broad-spectrum antibiotics, fluid resuscitation.
- Supportive Care: Vasopressors for hypotension, mechanical ventilation if needed, renal replacement therapy for kidney failure.
- Nursing Considerations:
- Early Recognition: Identifying signs and symptoms quickly to initiate treatment.
- Monitoring: Vital signs, urine output, mental status, and organ function regularly.
- Administration: Ensuring timely delivery of antibiotics and fluids as per protocols.
- Patient Teaching:
- Recognizing and reporting early signs of infection or sepsis.
- Importance of seeking immediate medical care when experiencing symptoms.
- Understanding the treatment plan and participating in care decisions.
6. Urinary Tract Infections (UTIs)
- Infections affecting any part of the urinary system, commonly the bladder (cystitis) or kidneys (pyelonephritis).
- Etiology:
- Common Pathogens: Escherichia coli (most common), Proteus mirabilis, Klebsiella pneumoniae, Staphylococcus saprophyticus.
- Risk Factors: Female anatomy, sexual activity, urinary catheterization, immunosuppression, diabetes mellitus.
- Clinical Manifestations:
- Cystitis: Dysuria, increased urinary frequency and urgency, suprapubic pain, cloudy or bloody urine.
- Pyelonephritis: Flank pain, high fever, chills, nausea, vomiting, costovertebral angle tenderness.
- Diagnosis:
- Tests: Urinalysis, urine culture and sensitivity, imaging studies (if recurrent or complicated).
- Treatment:
- Antibiotics: Based on culture results; commonly prescribed antibiotics include trimethoprim-sulfamethoxazole, nitrofurantoin, ciprofloxacin.
- Supportive Care: Increased fluid intake, analgesics for pain management.
- Nursing Considerations:
- Monitoring: Assessing for signs of systemic infection or complications.
- Encouraging: Adequate hydration and complete elimination of the bladder.
- Patient Teaching:
- Importance of completing the full antibiotic course.
- Preventive measures such as proper hygiene, urinating after sexual activity, and staying well-hydrated.
- Recognizing signs of recurrent infections and when to seek medical help.
Nursing Management and Patient Education
1. Nursing Interventions
- Assessment:
- Comprehensive health history focusing on exposure risks, travel history, immunization status.
- Monitoring vital signs regularly to detect early signs of infection or deterioration.
- Assessing for specific symptoms related to different infectious diseases.
- Medication Administration:
- Ensuring correct administration of antibiotics, antivirals, and other prescribed medications.
- Monitoring for therapeutic effects and adverse reactions.
- Infection Control:
- Implementing appropriate isolation precautions based on the mode of transmission.
- Educating healthcare staff and patients on proper hygiene practices.
- Supportive Care:
- Providing hydration, nutrition, and comfort measures to support the patient’s recovery.
- Assisting with activities of daily living, especially in debilitated patients.
- Coordination of Care:
- Collaborating with the healthcare team for comprehensive management, including referrals to specialists if needed.
- Ensuring continuity of care, especially during transitions between care settings.
2. Patient Education
- Medication Adherence:
- Emphasizing the importance of taking medications as prescribed and completing the full course, especially antibiotics to prevent resistance.
- Preventive Measures:
- Educating on hand hygiene, respiratory etiquette, safe sex practices, and vaccination schedules.
- Advising on lifestyle modifications such as smoking cessation, proper nutrition, and stress management to enhance immune function.
- Recognizing Symptoms:
- Teaching patients to recognize early signs of infection or complications and when to seek medical attention promptly.
- Self-Care Strategies:
- Encouraging practices like adequate rest, hydration, and proper wound care to support the body’s healing processes.
- Safety Precautions:
- Instructing on the use of personal protective equipment (PPE) when necessary and maintaining a clean environment to minimize infection risks.
3. Special Considerations
- Immunocompromised Patients:
- Extra vigilance in monitoring and preventing infections in patients with weakened immune systems (e.g., HIV/AIDS, chemotherapy patients).
- Elderly Patients:
- Recognizing atypical presentations of infections, such as confusion or falls, which may mask classic symptoms.
- Chronic Disease Management:
- Understanding the interplay between chronic conditions (e.g., diabetes, COPD) and susceptibility to infections, adjusting care plans accordingly.
- Cultural Sensitivity:
- Respecting and incorporating patients’ cultural beliefs and practices into care plans, especially regarding disease prevention and treatment preferences.
Examples
Example 1. Human Immunodeficiency Virus (HIV)/Acquired Immunodeficiency Syndrome (AIDS)
HIV is a retrovirus that targets and destroys CD4+ T cells, leading to progressive immune system failure and ultimately resulting in AIDS when the immune deficiency becomes severe. Transmission occurs through unprotected sexual contact, sharing contaminated needles, or from mother to child during childbirth or breastfeeding. Patients with HIV may initially present with flu-like symptoms during acute infection, followed by a prolonged asymptomatic phase. As the disease progresses to AIDS, individuals become susceptible to opportunistic infections such as Pneumocystis jiroveci pneumonia and certain cancers like Kaposi sarcoma. Diagnosis is confirmed through serologic tests like ELISA and Western blot, alongside monitoring CD4 counts and viral load. Treatment primarily involves antiretroviral therapy (ART), which includes a combination of NRTIs, NNRTIs, PIs, and integrase inhibitors to suppress viral replication. Nursing considerations focus on ensuring medication adherence, monitoring for side effects, providing education on transmission prevention, and supporting patients in managing opportunistic infections and maintaining overall health.
Example 2. Tuberculosis (TB)
Tuberculosis is a highly contagious bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs but capable of disseminating to other organs. TB spreads through airborne particles when an infected individual coughs or sneezes. Clinical manifestations include a chronic cough that may produce hemoptysis, night sweats, significant weight loss, fever, and fatigue. Diagnosis involves a combination of the tuberculin skin test (Mantoux), interferon-gamma release assays (IGRA), chest X-rays, and sputum cultures. Treatment requires a prolonged course of multiple antibiotics, typically including isoniazid, rifampin, pyrazinamide, and ethambutol over at least six months to prevent resistance. Nurses play a crucial role in monitoring patients for drug side effects, ensuring adherence to the treatment regimen, implementing airborne isolation precautions to prevent transmission, and educating patients on the importance of completing their therapy and recognizing symptoms of relapse or complications.
Example 3. Influenza
Influenza is a highly contagious viral respiratory infection caused by influenza viruses types A, B, and C. It spreads rapidly through respiratory droplets when an infected person coughs, sneezes, or talks. Symptoms are characterized by sudden onset of high fever, chills, myalgia, headache, cough, sore throat, and general fatigue. Diagnosis is often made using rapid influenza diagnostic tests (RIDTs) or reverse transcription-polymerase chain reaction (RT-PCR) assays. Treatment includes antiviral medications such as oseltamivir (Tamiflu) or zanamivir (Relenza), which are most effective when administered within 48 hours of symptom onset. Supportive care, including adequate hydration, rest, and antipyretics like acetaminophen or ibuprofen, is also essential. Nursing interventions involve initiating antiviral therapy promptly, implementing droplet precautions to prevent spread, educating patients on the importance of annual influenza vaccination, and promoting preventive measures like hand hygiene and respiratory etiquette.
Examnple 4. Pneumonia
Pneumonia is an inflammatory condition of the alveoli in one or both lungs, typically caused by infectious agents such as bacteria, viruses, or fungi. The most common bacterial cause is Streptococcus pneumoniae, while viral causes include influenza and Respiratory Syncytial Virus (RSV). Symptoms encompass productive or non-productive cough, fever, chills, dyspnea, chest pain, and auscultation findings like rales or crackles. Diagnosis is confirmed through chest X-rays, sputum cultures, and blood tests including complete blood counts (CBC) and blood cultures. Treatment varies based on the etiological agent but generally includes antibiotics for bacterial pneumonia (e.g., macrolides, cephalosporins), antiviral agents for viral pneumonia, and antifungal medications for fungal pneumonia. Supportive care may involve oxygen therapy, hydration, and bronchodilators if necessary. Nursing responsibilities include monitoring respiratory status and oxygenation, encouraging deep breathing and coughing exercises to promote sputum expectoration, ensuring adherence to the antibiotic regimen, and educating patients on preventive measures such as vaccination against pneumococcal pneumonia and influenza.
Example 5. Urinary Tract Infections (UTIs)
Urinary Tract Infections are infections that can affect any part of the urinary system, with the bladder (cystitis) and kidneys (pyelonephritis) being the most commonly involved sites. The primary causative agent is Escherichia coli, although other bacteria like Proteus mirabilis, Klebsiella pneumoniae, and Staphylococcus saprophyticus can also be responsible. Risk factors include female anatomy, sexual activity, urinary catheterization, immunosuppression, and underlying conditions such as diabetes mellitus. Symptoms of cystitis include dysuria, increased urinary frequency and urgency, suprapubic pain, and cloudy or bloody urine, whereas pyelonephritis presents with flank pain, high fever, chills, nausea, vomiting, and costovertebral angle tenderness. Diagnosis is based on urinalysis, urine culture and sensitivity, and sometimes imaging studies if the infection is recurrent or complicated. Treatment typically involves antibiotics such as trimethoprim-sulfamethoxazole, nitrofurantoin, or ciprofloxacin, depending on the pathogen and patient factors. Nursing care includes encouraging increased fluid intake to flush the urinary system, monitoring for signs of systemic infection or complications, ensuring patients complete their antibiotic course, and providing education on preventive measures like proper hygiene, urinating after sexual activity, and staying well-hydrated.
Practice Questions
Question 1
A patient with newly diagnosed HIV presents to the clinic. Which of the following findings would the nurse expect to see in a patient progressing to Acquired Immunodeficiency Syndrome (AIDS)?
A) Elevated CD4+ T-cell count
B) Persistent generalized lymphadenopathy
C) Decreased susceptibility to opportunistic infections
D) Rapid viral replication with increasing CD4+ T-cell count
Answer: B) Persistent generalized lymphadenopathy
Explanation: As HIV progresses towards AIDS, the patient’s immune system becomes increasingly compromised, particularly marked by a decline in CD4+ T-cell counts. Persistent generalized lymphadenopathy, which refers to swollen lymph nodes lasting more than three months, is a common clinical sign observed during this advanced stage. This condition reflects the body’s ongoing immune response to the chronic presence of the virus. In contrast, an elevated CD4+ T-cell count (Option A) would indicate a healthier immune status, which is not expected as HIV advances. Additionally, patients with AIDS exhibit increased susceptibility to opportunistic infections (contrary to Option C) due to their weakened immune defenses. Lastly, while rapid viral replication is characteristic of HIV infection, it is associated with decreasing, not increasing, CD4+ T-cell counts (Option D). Therefore, persistent generalized lymphadenopathy is the most accurate indicator of progression to AIDS.
Question 2
A nurse is caring for a patient diagnosed with tuberculosis (TB). Which of the following isolation precautions should the nurse implement to prevent the spread of TB?
A) Standard precautions only
B) Contact precautions
C) Droplet precautions
D) Airborne precautions
Correct Answer: D) Airborne precautions
Explanation: Tuberculosis is an airborne infectious disease caused by Mycobacterium tuberculosis. Due to its mode of transmission through airborne particles that can remain suspended in the air for extended periods, implementing airborne precautions is essential to prevent its spread within healthcare settings. Airborne precautions involve placing the patient in a negative pressure room, using N95 respirators or higher-level respirators for all healthcare workers entering the room, and minimizing the movement of the patient to reduce contamination. While standard precautions (Option A) are always necessary, they are insufficient alone for TB. Contact precautions (Option B) are reserved for infections spread by direct or indirect contact, such as MRSA or VRE, and droplet precautions (Option C) are appropriate for pathogens transmitted via larger respiratory droplets, like influenza or pertussis, which do not linger in the air as long as airborne particles. Therefore, airborne precautions are the most appropriate and effective measures for containing TB.
Question 3
A patient with pneumonia is prescribed an antibiotic regimen. Which of the following statements by the patient indicates a need for further teaching?
A) “I should take my antibiotic doses at evenly spaced intervals.”
B) “It’s okay to stop taking the antibiotic when I start feeling better.”
C) “I will report any new symptoms like rash or swelling to my nurse.”
D) “I should drink plenty of fluids while taking this medication.”
Answer: B) “It’s okay to stop taking the antibiotic when I start feeling better.”
Explanation: Adherence to the full course of prescribed antibiotics is critical in treating pneumonia effectively and preventing the development of antibiotic-resistant bacteria. The patient’s statement in Option B, “It’s okay to stop taking the antibiotic when I start feeling better,” reflects a misunderstanding that can lead to incomplete treatment and potential relapse or resistance. This indicates a need for further education to emphasize the importance of completing the entire antibiotic regimen, even if symptoms improve before the medication is finished. On the other hand, the statements in Options A, C, and D demonstrate appropriate understanding: taking doses at evenly spaced intervals ensures consistent drug levels in the body, reporting new symptoms like rash or swelling helps monitor for adverse reactions, and drinking plenty of fluids supports the body’s ability to fight infection and can mitigate certain side effects of medications. Therefore, the nurse should address and correct the misconception presented in Option B to ensure effective treatment and patient safety.