The integumentary system, comprising the skin, hair, nails, and associated glands, plays a vital role in adult health by providing protection, regulating temperature, and enabling sensory perception. For NCLEX-PN® candidates, understanding the anatomy and physiology of the integumentary system is essential, as it underpins the assessment, diagnosis, and management of common adult skin disorders such as infections, ulcers, burns, and skin cancers. Mastery of this topic ensures comprehensive patient care and effective intervention strategies, crucial for achieving a high score on the exam.
Learning Objectives
In studying “Adult Health: Integumentary” for the NCLEX-PN® Exam, you should understand the various integumentary system disorders affecting adults, including skin conditions, hair and nail abnormalities, and related injuries. Analyze the pathophysiology, clinical manifestations, and treatment protocols for each disorder. Evaluate nursing considerations such as infection control measures, wound care, medication administration, patient monitoring, potential drug interactions, and safety precautions. Additionally, explore the clinical applications of these disorders in diagnosing and managing patient care, including assessment techniques and preventive strategies, and apply your understanding to effectively respond to integumentary-related scenarios and questions on the NCLEX-PN® exam.
Anatomy and Physiology of the Integumentary System
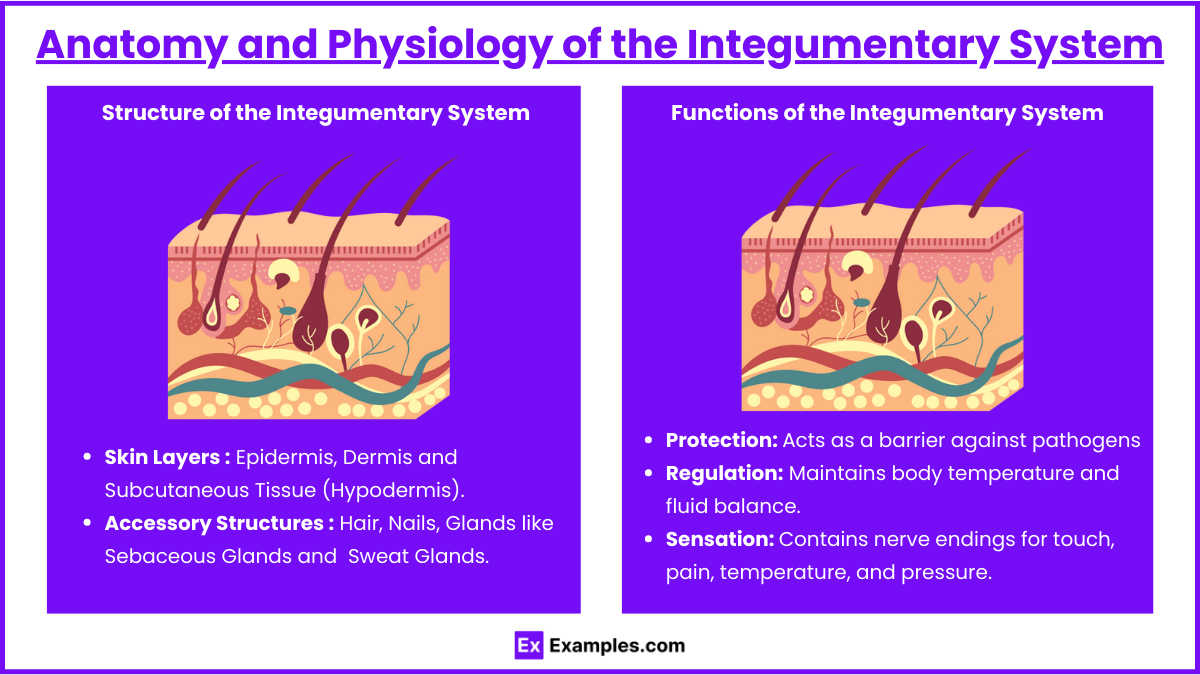
1. Structure of the Integumentary System
- Skin Layers:
- Epidermis: Outermost layer providing a waterproof barrier and determining skin tone.
- Dermis: Contains connective tissue, hair follicles, sweat glands, and nerve endings.
- Subcutaneous Tissue (Hypodermis): Insulates the body and absorbs shock.
- Accessory Structures:
- Hair: Protects against UV radiation and aids in temperature regulation.
- Nails: Protect fingertips and enhance sensory perception.
- Glands:
- Sebaceous Glands: Produce sebum to lubricate skin and hair.
- Sweat Glands: Regulate body temperature through perspiration.
2. Functions of the Integumentary System
- Protection: Acts as a barrier against pathogens, chemicals, and physical injuries.
- Regulation: Maintains body temperature and fluid balance.
- Sensation: Contains nerve endings for touch, pain, temperature, and pressure.
- Vitamin D Synthesis: Facilitates the production of vitamin D when exposed to sunlight.
Common Integumentary Disorders and Their Management
1. Skin Infections : Skin infections are conditions where harmful microorganisms such as bacteria, fungi, or viruses invade and multiply in the skin, causing inflammation, redness, itching, swelling, and in some cases, fluid-filled blisters or pustules. These infections may be superficial or deep, and they often require specific treatment to prevent complications like abscess formation or systemic infection.
- Cellulitis:
- Cause: Bacterial (Streptococcus, Staphylococcus).
- Management: Administer antibiotics, elevate affected area, monitor for spread.
- Impetigo:
- Cause: Highly contagious bacterial (Staphylococcus aureus).
- Management: Apply topical antibiotics, maintain hygiene, isolate to prevent transmission.
- Fungal Infections (Tinea, Candidiasis):
- Symptoms: Itchy, red, scaly patches.
- Management: Use antifungal creams, keep areas dry, educate on proper hygiene.
2. Dermatologic Conditions : Dermatologic conditions refer to a wide range of diseases that affect the skin, hair, and nails. These conditions can be caused by immune system dysfunction, genetic predisposition, irritants, and allergens. They may present with symptoms like itching, scaling, redness, and inflammation. Proper identification, treatment, and management are essential to prevent complications and improve the patient’s quality of life.
- Psoriasis:
- Characteristics: Chronic autoimmune condition with red, scaly patches.
- Management: Topical treatments, phototherapy, systemic medications, patient education.
- Eczema (Atopic Dermatitis):
- Characteristics: Inflammatory with itchy, red, cracked skin.
- Management: Moisturizers, topical corticosteroids, avoiding irritants.
- Acne Vulgaris:
- Characteristics: Blocked hair follicles with oil and dead skin cells.
- Management: Topical retinoids, benzoyl peroxide, antibiotics, skincare education.
3. Skin Cancers : Skin cancer is the abnormal, uncontrolled growth of skin cells, often caused by ultraviolet (UV) radiation from the sun or tanning beds. Skin cancers can be classified into three major types: basal cell carcinoma, squamous cell carcinoma, and melanoma. Early detection and treatment are crucial to prevent the spread (metastasis) of cancer cells to other organs.
- Basal Cell Carcinoma:
- Characteristics: Most common, slow-growing, rarely metastasizes.
- Management: Surgical removal, monitoring, sun protection education.
- Squamous Cell Carcinoma:
- Characteristics: More likely to spread than basal cell.
- Management: Similar to basal cell but may require more aggressive treatment.
- Melanoma:
- Characteristics: Deadly, arises from melanocytes.
- Management: Early detection (ABCDE), surgical excision, possible chemotherapy or radiation.
4. Other Conditions : Other conditions affecting the skin include pressure ulcers, burns, varicose veins, and edema. These conditions require immediate intervention to prevent complications like infections, necrosis, and fluid imbalance. Proper management can promote healing and improve patient outcomes.
- Pressure Ulcers (Bedsores):
- Stages: I-IV based on severity.
- Management: Regular repositioning, pressure-relieving devices, wound care, nutrition support.
- Burns:
- Classification: First-degree (epidermis), second-degree (epidermis and dermis), third-degree (full thickness).
- Management: Airway management, fluid resuscitation, wound care, pain management, infection prevention.
- Varicose Veins and Edema:
- Varicose Veins: Enlarged, twisted veins; management includes compression therapy and leg elevation.
- Edema: Caused by heart, kidney, liver issues; management involves identifying the cause, diuretics, mobility, limb elevation.
Nursing Assessment, Interventions, and Patient Education

1. Assessment of the Integumentary System
- Inspection:
- Color: Look for pallor, cyanosis, jaundice, erythema.
- Temperature: Assess for warmth or coolness.
- Moisture: Check for dryness or excessive moisture.
- Texture and Turgor: Evaluate skin smoothness, elasticity, and hydration.
- Lesions: Identify type, size, location, and characteristics.
- Palpation:
- Temperature and Texture: Detect irregularities or areas of increased/decreased warmth.
- Turgor: Assess skin elasticity by pinching.
- Special Tests: Percussion and auscultation in specific cases (e.g., gas gangrene).
- Documentation: Accurately describe findings, use photographic documentation when appropriate.
2. Nursing Interventions and Management
- Wound Care:
- Assessment: Determine wound type and stage.
- Cleaning and Dressing: Use appropriate solutions and dressings based on wound needs.
- Debridement: Remove necrotic tissue if necessary.
- Monitoring: Observe for signs of healing or complications.
- Managing Pressure Ulcers:
- Repositioning: Every 2 hours to relieve pressure.
- Support Surfaces: Utilize specialized mattresses or cushions.
- Nutrition: Ensure adequate protein and calorie intake.
- Skin Care: Keep skin clean and dry, use barrier creams.
- Treating Burns:
- Fluid Management: Calculate needs using formulas like Parkland.
- Wound Care: Apply topical agents and sterile dressings.
- Pain Management: Administer analgesics as prescribed.
- Infection Prevention: Use antibiotics if necessary, maintain sterile techniques.
- Varicose Veins and Edema Management:
- Compression Therapy: Apply stockings or bandages.
- Elevation: Elevate legs above heart level.
- Mobility: Encourage movement and leg exercises.
- Medication Administration: Administer diuretics as prescribed.
- Skin Cancer Management:
- Surgical Intervention: Assist with excision procedures.
- Education: Teach about sun protection and self-exams.
- Follow-Up: Schedule regular monitoring check-ups.
3. Patient Education
- Skin Protection:
- Sun Protection: Use broad-spectrum sunscreen (SPF 30+), wear protective clothing, avoid peak sun hours.
- Moisturizing: Regular use to prevent dryness and cracking.
- Avoid Irritants: Identify and avoid allergens or irritants.
- Wound Care:
- Home Care Instructions: How to clean and dress wounds, recognize signs of infection.
- Repositioning Techniques: Proper methods for bedridden patients.
- Nutrition:
- Dietary Recommendations: High-protein, high-calorie diets to support healing.
- Hydration: Ensure adequate fluid intake.
- Recognizing Signs of Complications:
- Infections: Redness, increased pain, swelling, purulent drainage, fever.
- Delayed Healing: Persistent wounds, lack of granulation.
- Allergic Reactions: Rash, itching, swelling after exposure to irritants.
- Lifestyle Modifications:
- Smoking Cessation: Improves circulation and healing.
- Weight Management: Reduces risk of varicose veins and pressure ulcers.
- Regular Skin Checks: For early detection of skin cancers.
4. Pharmacological Considerations
- Topical Agents: Antibiotics (e.g., mupirocin), antifungals (e.g., clotrimazole), corticosteroids (e.g., hydrocortisone), emollients.
- Systemic Medications: Oral or IV antibiotics, immunosuppressants for autoimmune conditions, analgesics for pain management.
- Pain Management: Utilize multimodal approaches and regularly assess pain levels.
5. Special Considerations
- Elderly Patients: Thin skin, decreased turgor, slower healing.
- Diabetic Patients: High risk of foot ulcers and infections, require regular inspections.
- Immunocompromised Patients: Higher infection risk, necessitate vigilant monitoring and aseptic techniques.
Examples
Example 1: Cellulitis Management in an Elderly Patient
An 82-year-old female patient presents with a red, swollen, and warm area on her lower leg accompanied by tenderness and mild fever. The nurse suspects cellulitis, a common bacterial skin infection often caused by Streptococcus or Staphylococcus species. Key nursing interventions include administering prescribed antibiotics promptly to combat the infection, elevating the affected limb to reduce swelling, and monitoring vital signs for any signs of systemic infection. Additionally, the nurse should educate the patient on proper skin care and hygiene to prevent recurrence, especially considering the patient’s advanced age, which may impair skin integrity and immune response.
Example 2: Pressure Ulcer Prevention in a Bedridden Patient
A 68-year-old bedridden male patient with limited mobility is at high risk for developing pressure ulcers (bedsores). To prevent skin breakdown, the nurse should implement a comprehensive pressure ulcer prevention plan. This includes repositioning the patient at least every two hours to alleviate pressure on vulnerable areas such as the sacrum, heels, and elbows. Utilizing pressure-relieving devices like specialized mattresses or cushions can further reduce risk. The nurse must also ensure the patient receives adequate nutrition and hydration to maintain skin integrity, perform regular skin assessments to identify early signs of pressure ulcers, and educate the patient and family members about the importance of mobility and skin care.
Example 3: Burn Care and Fluid Management in a Burn Victim
A 35-year-old male patient arrives in the emergency department with second-degree burns covering 30% of his body following a house fire. Immediate nursing care focuses on airway management, especially if there is a risk of inhalation injury due to smoke inhalation. Fluid resuscitation is critical to prevent hypovolemia and maintain organ perfusion, typically guided by formulas such as the Parkland formula. The nurse should administer intravenous fluids as prescribed, provide pain management through analgesics, and apply appropriate wound dressings to promote healing and prevent infection. Continuous monitoring for signs of infection and complications, along with educating the patient on burn care and rehabilitation, are essential components of comprehensive burn management.
Example 4: Identification and Management of Melanoma
A 50-year-old patient presents with a mole that has changed in size, shape, and color over the past few months. The nurse recognizes these changes as potential indicators of melanoma, a serious and potentially deadly form of skin cancer. Using the ABCDE criteria (Asymmetry, Border irregularity, Color variation, Diameter greater than 6mm, and Evolving characteristics), the nurse assesses the lesion and promptly refers the patient for further diagnostic procedures such as a biopsy. Nursing interventions include providing emotional support, educating the patient about the importance of early detection and treatment, and discussing preventive measures like sun protection and regular skin self-examinations. Early identification and management are crucial for improving prognosis in melanoma cases.
Example 5: Diabetic Foot Ulcer Care in a Patient with Peripheral Neuropathy
A 60-year-old diabetic patient with peripheral neuropathy presents with a non-healing ulcer on the plantar surface of the foot. Due to decreased sensation, the patient may not have felt the initial trauma, leading to prolonged ulceration and increased risk of infection. The nurse’s role includes conducting a thorough foot assessment to evaluate the ulcer’s depth, presence of infection, and vascular status. Implementing appropriate wound care techniques, such as cleaning the ulcer, applying suitable dressings, and possibly debriding necrotic tissue, is essential. Additionally, the nurse should educate the patient on proper foot care practices, including daily inspection of feet, wearing protective footwear, and managing blood glucose levels to promote healing and prevent future complications.
Practice Questions
Question 1
A 68-year-old patient with limited mobility presents with a new area of redness over the sacrum. The skin is intact, and the patient reports mild discomfort when the area is pressed. What is the most appropriate initial nursing action?
A. Apply a moisturizing lotion to the affected area.
B. Reposition the patient every 2 hours.
C. Document the redness and continue current care.
D. Initiate a course of broad-spectrum antibiotics.
Answer: B. Reposition the patient every 2 hours.
Explanation: The patient is exhibiting signs of a Stage I pressure ulcer, characterized by non-blanchable erythema of intact skin. The most appropriate initial action is to reposition the patient regularly (every 2 hours) to alleviate pressure on the affected area, promoting blood flow and preventing progression to more severe stages. Applying moisturizing lotion (Option A) may be part of routine skin care but does not address the immediate issue of pressure. Documenting the redness (Option C) is necessary but insufficient as a sole action. Initiating antibiotics (Option D) is inappropriate unless there are signs of infection, which are not present at this stage.
Question 2
A nurse is caring for a patient diagnosed with melanoma. Which of the following instructions should the nurse include in the patient’s discharge teaching?
A. “Use a tanning bed to strengthen your skin against UV rays.”
B. “Perform regular self-examinations of your skin for new or changing moles.”
C. “Apply topical corticosteroids daily to prevent recurrence.”
D. “Limit your intake of vitamin D-rich foods to reduce skin pigmentation.”
Answer: B. “Perform regular self-examinations of your skin for new or changing moles.”
Explanation: For patients diagnosed with melanoma, it is crucial to educate them on the importance of regular self-examinations to detect any new or changing moles early, facilitating prompt medical attention and treatment. Using tanning beds (Option A) is contraindicated as UV exposure is a significant risk factor for melanoma. Topical corticosteroids (Option C) are not a standard preventive measure for melanoma recurrence. Limiting vitamin D intake (Option D) is unnecessary and not related to melanoma management; in fact, some vitamin D is beneficial for overall health.
Question 3
A patient with type 2 diabetes mellitus reports a painful, red, swollen foot with a small open wound on the sole. The nurse recognizes this presentation as a potential complication and knows the priority intervention is to:
A. Apply a warm compress to the affected area.
B. Encourage the patient to increase fluid intake.
C. Elevate the foot and notify the healthcare provider immediately.
D. Instruct the patient to inspect the foot daily for changes.
Answer: C. Elevate the foot and notify the healthcare provider immediately.
Explanation: The patient’s symptoms suggest a diabetic foot ulcer, which poses a high risk for infection and potential complications such as osteomyelitis or sepsis. The priority intervention is to elevate the foot to reduce swelling and notify the healthcare provider immediately for appropriate management, which may include antibiotics or further evaluation. Applying a warm compress (Option A) may exacerbate swelling if there is an infection. Encouraging increased fluid intake (Option B) is beneficial for overall health but not the immediate priority. Instructing daily inspections (Option D) is important for prevention and early detection but does not address the acute issue at hand.