"Leadership & Management: Management Concepts" for the NCLEX-PN® focuses on the essential skills that LPNs need to provide effective patient care. These concepts include delegation, prioritization, time management, and decision-making, all of which are crucial for ensuring patient safety, promoting teamwork, and maintaining efficient healthcare operations. LPNs must apply critical thinking, ethical principles, and legal standards while leading healthcare teams. Mastering these management concepts enhances patient outcomes and increases the likelihood of achieving a high score on the NCLEX-PN® exam.
Learning Objectives
In studying "Leadership & Management: Management Concepts" for the NCLEX-PN® Exam, you should learn to understand essential management principles, including delegation, prioritization, time management, and decision-making. Analyze the roles and responsibilities of LPNs in leading care teams, coordinating patient care, and supporting RNs. Evaluate factors that influence management decisions, such as patient acuity, staffing levels, and available resources. Explore key nursing considerations like accountability, effective communication, and conflict resolution. Apply knowledge to prioritize patient care, promote teamwork, and manage multiple responsibilities efficiently. Mastering these concepts ensures safe, high-quality patient care and enhances your ability to lead in healthcare environments.
1. Core Management Concepts
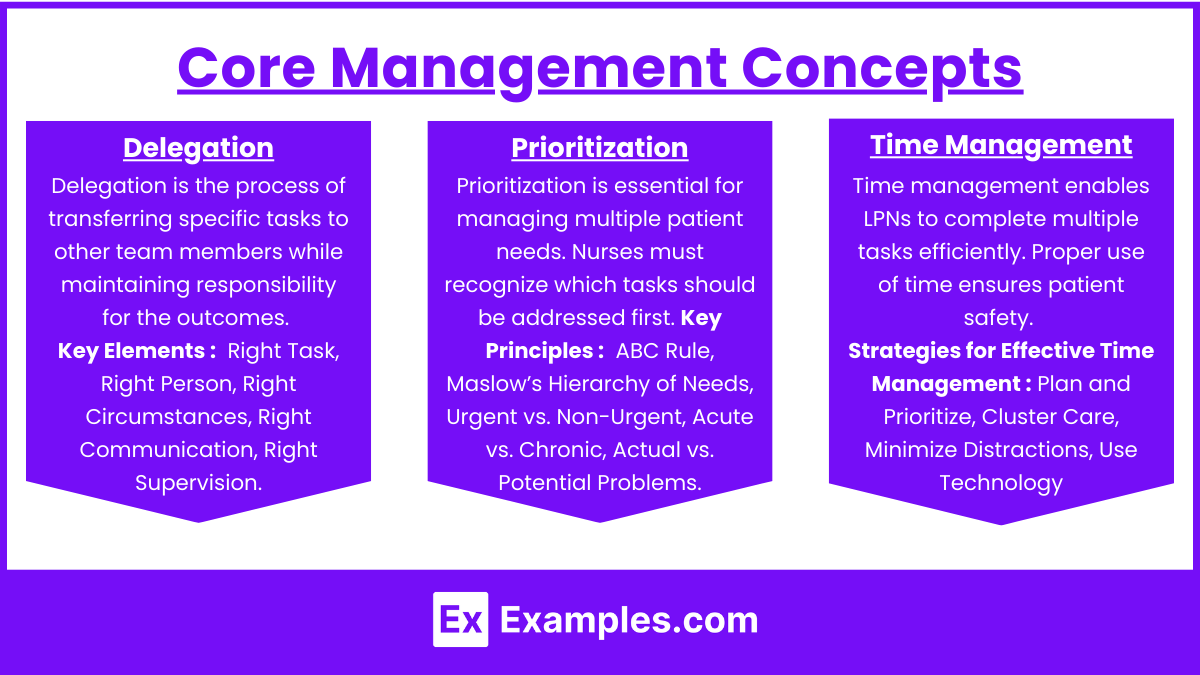
The core management concepts that LPNs must master for the NCLEX-PN® include delegation, prioritization, time management, and decision-making. These concepts are essential for ensuring patient safety, promoting teamwork, and maintaining efficient healthcare operations.
Delegation
Delegation is the process of transferring specific tasks to other team members while maintaining responsibility for the outcomes. LPNs often delegate tasks to certified nursing assistants (CNAs) or unlicensed assistive personnel (UAPs).
Key Elements of Delegation
Right Task: Assign tasks that are within the assistant’s scope of practice.
Right Person: Ensure the individual has the skills and knowledge to complete the task.
Right Circumstances: Consider the patient's condition and the complexity of the task.
Right Communication: Provide clear, specific instructions about what is to be done.
Right Supervision: Monitor the delegatee’s performance and provide feedback.
Tasks LPNs Can Delegate
Assisting with activities of daily living (ADLs) like bathing and feeding.
Vital signs monitoring for stable patients.
Collecting specimens (e.g., urine samples).
Tasks LPNs Should NOT Delegate
Patient assessments.
Administration of medications that require clinical judgment.
Handling complex or unstable patients.
Prioritization
Prioritization is essential for managing multiple patient needs. Nurses must recognize which tasks should be addressed first. The NCLEX-PN® exam often includes questions that require prioritization skills.
Key Principles of Prioritization
ABC Rule (Airway, Breathing, Circulation): Address life-threatening conditions first.
Maslow’s Hierarchy of Needs: Address physiological needs before psychological or social needs.
Urgent vs. Non-Urgent: Focus on urgent and time-sensitive needs before chronic issues.
Acute vs. Chronic: Acute conditions take priority over chronic, stable conditions.
Actual vs. Potential Problems: Address existing patient issues before potential ones.
Time Management
Time management enables LPNs to complete multiple tasks efficiently. Proper use of time ensures patient safety, reduces nurse fatigue, and prevents delays in care.
Strategies for Effective Time Management
Plan and Prioritize: Use a checklist to manage daily tasks.
Cluster Care: Complete multiple tasks during one patient visit (e.g., checking vitals, administering medications, and providing hygiene care).
Minimize Distractions: Limit unnecessary interruptions like personal phone use.
Use Technology: Utilize electronic health records (EHRs) to streamline charting.
2. Key Roles of LPNs in Leadership and Management
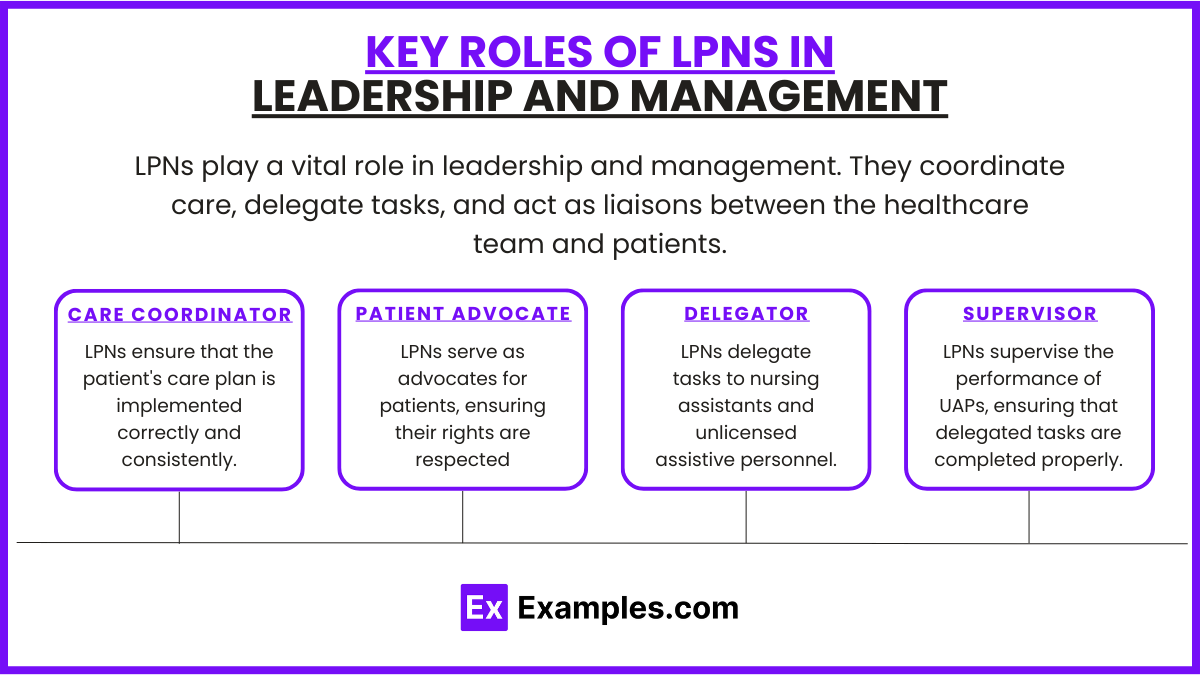
LPNs play a vital role in leadership and management. They coordinate care, delegate tasks, and act as liaisons between the healthcare team and patients.
Care Coordinator
LPNs ensure that the patient's care plan is implemented correctly and consistently.
Responsibilities: Update the care plan, coordinate with RNs, and communicate with families.
Example: Ensuring that wound care is done according to the prescribed treatment plan.
Patient Advocate
LPNs serve as advocates for patients, ensuring their rights are respected and that they receive appropriate care.
Responsibilities: Ensure informed consent is obtained and advocate for patient preferences.
Example: Speaking up for a patient who refuses a medical procedure.
Delegator
LPNs delegate tasks to nursing assistants and unlicensed assistive personnel.
Responsibilities: Assign appropriate tasks, provide clear instructions, and supervise performance.
Example: Instructing a CNA to collect vital signs for a stable patient.
Supervisor
LPNs supervise the performance of UAPs, ensuring that delegated tasks are completed properly.
Responsibilities: Monitor progress, correct errors, and provide feedback.
Example: Monitoring how CNAs assist with patient hygiene and intervening if needed.
3. Legal and Ethical Considerations in Management Concepts
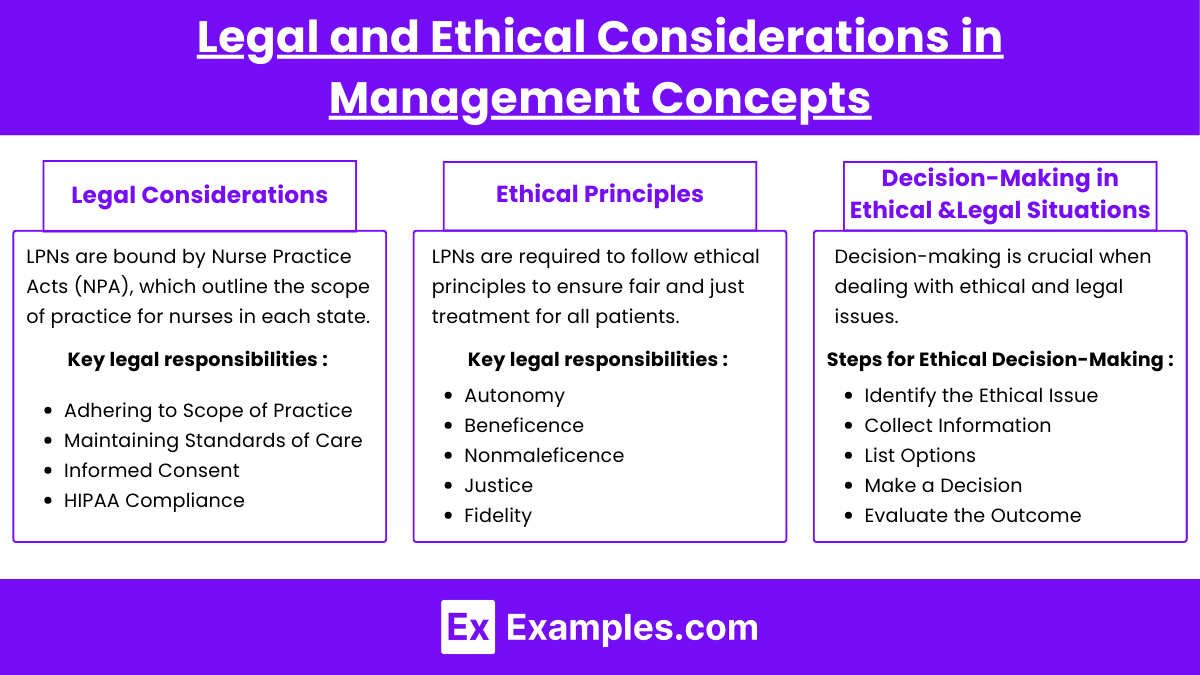
LPNs must follow legal guidelines and ethical principles while managing patient care. These considerations help prevent malpractice, protect patient rights, and maintain ethical standards.
Legal Considerations
LPNs are bound by Nurse Practice Acts (NPA), which outline the scope of practice for nurses in each state. Key legal responsibilities include:
Adhering to Scope of Practice: Ensuring tasks are within the limits of the nurse's role.
Maintaining Standards of Care: Providing care that meets established nursing standards.
Informed Consent: Verifying that the patient understands procedures before they are performed.
HIPAA Compliance: Protecting the privacy and confidentiality of patient information.
Examples of Legal Issues
Negligence: Failing to provide proper care, leading to patient harm.
Malpractice: Committing an act of misconduct, such as administering the wrong medication.
Ethical Principles
LPNs are required to follow ethical principles to ensure fair and just treatment for all patients. Ethical principles include:
Autonomy: Respecting the patient’s right to make their own healthcare decisions.
Beneficence: Acting in the patient’s best interest.
Nonmaleficence: Avoiding actions that may harm the patient.
Justice: Providing equal treatment to all patients.
Fidelity: Maintaining trust and loyalty with patients.
Examples of Ethical Issues
Informed Consent: Ensuring the patient is fully aware of the risks of a procedure.
End-of-Life Care: Providing support for patients with Do-Not-Resuscitate (DNR) orders.
Decision-Making in Ethical and Legal Situations
Decision-making is crucial when dealing with ethical and legal issues. LPNs must use clinical judgment to resolve ethical dilemmas and comply with legal standards.
Steps for Ethical Decision-Making
Identify the Ethical Issue: Determine the nature of the conflict.
Collect Information: Gather facts about the patient, their wishes, and the clinical situation.
List Options: Consider possible actions or solutions.
Make a Decision: Select the best course of action.
Evaluate the Outcome: Assess the impact of the action taken.
Examples
Example 1: Delegation of Tasks
One of the most critical management concepts tested in the NCLEX-PN® exam is the ability to delegate tasks appropriately. As an LPN, you must know how to assign tasks to Certified Nursing Assistants (CNAs) or Unlicensed Assistive Personnel (UAPs) while ensuring that the "Five Rights of Delegation" are met. For example, you may delegate tasks like taking vital signs, assisting with feeding, or helping patients with activities of daily living (ADLs). However, tasks that require clinical judgment, such as patient assessments or medication administration, should not be delegated. The NCLEX-PN® may present a scenario where you must determine which tasks can be assigned to a CNA and which must be handled by the LPN.
Example 2: Prioritization of Patient Care
Prioritization is essential in managing multiple patients with competing needs. LPNs must identify which patients require immediate attention. For instance, a patient with shortness of breath (airway issue) should be attended to before a patient requesting assistance with personal hygiene. This concept is frequently tested using the ABCs (Airway, Breathing, Circulation) and Maslow’s Hierarchy of Needs. Questions may present a list of patient scenarios, requiring you to determine which patient to prioritize first. For example, a patient experiencing chest pain (circulation issue) takes priority over a patient with a request for discharge instructions.
Example 3: Time Management and Efficiency
Managing time effectively is vital in ensuring that all nursing tasks are completed within a shift. On the NCLEX-PN®, you may be asked how to organize your workflow for maximum efficiency. For instance, instead of visiting one patient at a time, you might be tested on how to "cluster care" by performing multiple tasks for one patient during the same visit. This could include administering medications, assessing vital signs, and assisting with hygiene, all at once. This strategy prevents repetitive trips to the patient’s room, saving valuable time. Effective time management is especially important when caring for multiple patients simultaneously.
Example 4: Conflict Resolution and Teamwork
In healthcare, LPNs often encounter conflicts between patients, families, and colleagues. As part of leadership and management, LPNs must resolve disputes and maintain a positive work environment. For example, if a CNA refuses to perform a delegated task, the LPN must use active listening and collaborative problem-solving to resolve the conflict. Questions on the NCLEX-PN® may ask you to choose the best approach to handle team conflicts. Strategies like addressing the issue directly, encouraging open communication, and involving the nurse manager if necessary, are key concepts tested on the exam.
Example 5: Decision-Making and Clinical Judgment
Clinical decision-making is at the heart of effective nursing management. LPNs must make fast, evidence-based decisions while caring for patients. For example, if a patient shows signs of an allergic reaction after taking a new medication, the LPN must recognize the urgency of the situation and act accordingly. The NCLEX-PN® may test your decision-making by presenting a scenario where you must identify the best response to a patient's change in condition. This may involve notifying the registered nurse (RN) or initiating immediate action, such as stopping a medication infusion. Effective decision-making requires the ability to analyze patient information, assess risks, and prioritize appropriate interventions.
Practice Questions
Question 1
A Licensed Practical Nurse (LPN) is assigned to care for four patients. Which of the following tasks is appropriate for the LPN to delegate to an unlicensed assistive personnel (UAP)?
A. Administer oral medications to a stable patient.
B. Measure and record vital signs of a post-operative patient.
C. Assess the pain level of a patient who just had surgery.
D. Teach a patient how to self-administer insulin injections.
Answer: B. Measure and record vital signs of a post-operative patient.
Explanation:
Option A: Incorrect — Administering medications is beyond the scope of a UAP. Only LPNs, RNs, or higher-level licensed providers can administer medications.
Option B: Correct — Measuring and recording vital signs is within the UAP’s scope of practice. It is a routine, non-complex task that does not require clinical judgment.
Option C: Incorrect — Assessing pain requires critical thinking and clinical judgment, which are responsibilities of the LPN or RN.
Option D: Incorrect — Teaching requires specialized knowledge and is part of the LPN's scope of practice, not the UAP's.
Question 2
The LPN is caring for four patients. Which patient should the LPN prioritize first?
A. A 68-year-old patient with chronic back pain requesting medication.
B. A 55-year-old patient who is post-operative and has a heart rate of 120 bpm.
C. A 42-year-old patient with a scheduled discharge at 11:00 AM today.
D. A 30-year-old patient who is ready for routine dressing change.
Answer: B. A 55-year-old patient who is post-operative and has a heart rate of 120 bpm.
Explanation:
Option A: Incorrect — Although pain management is essential, chronic back pain is not life-threatening and does not require immediate intervention.
Option B: Correct — A heart rate of 120 bpm (tachycardia) in a post-operative patient may indicate potential complications such as pain, infection, blood loss, or hemorrhage. This patient is the highest priority.
Option C: Incorrect — While the discharge process is important, it is not urgent compared to a potential medical emergency.
Option D: Incorrect — Dressing changes are routine and not life-threatening. This task can be scheduled after urgent needs are addressed.
Question 3
The LPN begins a shift with several tasks to complete. Which task should the LPN complete first?
A. Administer pain medication to a patient experiencing a pain level of 8 out of 10.
B. Reassess a patient's blood pressure after administering antihypertensive medication 30 minutes ago.
C. Provide discharge instructions to a patient who is scheduled to leave at noon.
D. Change the dressing on a wound that has minimal drainage.
Answer: A. Administer pain medication to a patient experiencing a pain level of 8 out of 10.
Explanation:
Option A: Correct — Managing a patient's pain (rated 8/10) is a priority since unrelieved pain affects vital signs, mobility, and recovery. Pain management should be addressed promptly.
Option B: Incorrect — While it is important to reassess blood pressure after administering antihypertensive medication, this task is less urgent than addressing a pain level of 8/10.
Option C: Incorrect — Discharge planning is important, but it is a lower priority than addressing immediate patient pain.
Option D: Incorrect — A wound with minimal drainage does not require immediate attention compared to a patient in significant pain.