The "Adult Health: Musculoskeletal" section for the NCLEX-PN® exam focuses on the structure, function, and disorders of the musculoskeletal system, which includes bones, muscles, joints, ligaments, and tendons. This system provides support, movement, and protection for vital organs. Understanding musculoskeletal conditions such as fractures, arthritis, osteoporosis, and sprains is essential for providing effective patient care. Practical nursing skills include pain management, mobility support, fall prevention, and patient education. Mastering these concepts will help you answer related questions accurately on the NCLEX-PN® exam.
Learning Objectives
In studying "Adult Health: Musculoskeletal" for the NCLEX-PN® Exam, you should learn to understand the anatomy and physiology of the musculoskeletal system, including bones, joints, muscles, ligaments, and tendons. Analyze common musculoskeletal conditions such as fractures, osteoarthritis, rheumatoid arthritis, osteoporosis, and sprains, focusing on pathophysiology, clinical manifestations, and treatment options. Evaluate nursing considerations like patient assessment, pain management, promoting mobility, and preventing complications such as contractures and pressure ulcers. Explore pharmacological interventions, including analgesics, anti-inflammatory medications, and muscle relaxants. Apply your knowledge to effectively respond to musculoskeletal-related scenarios, ensuring patient safety and prioritizing care in NCLEX-PN® exam questions.
Overview of the Musculoskeletal System
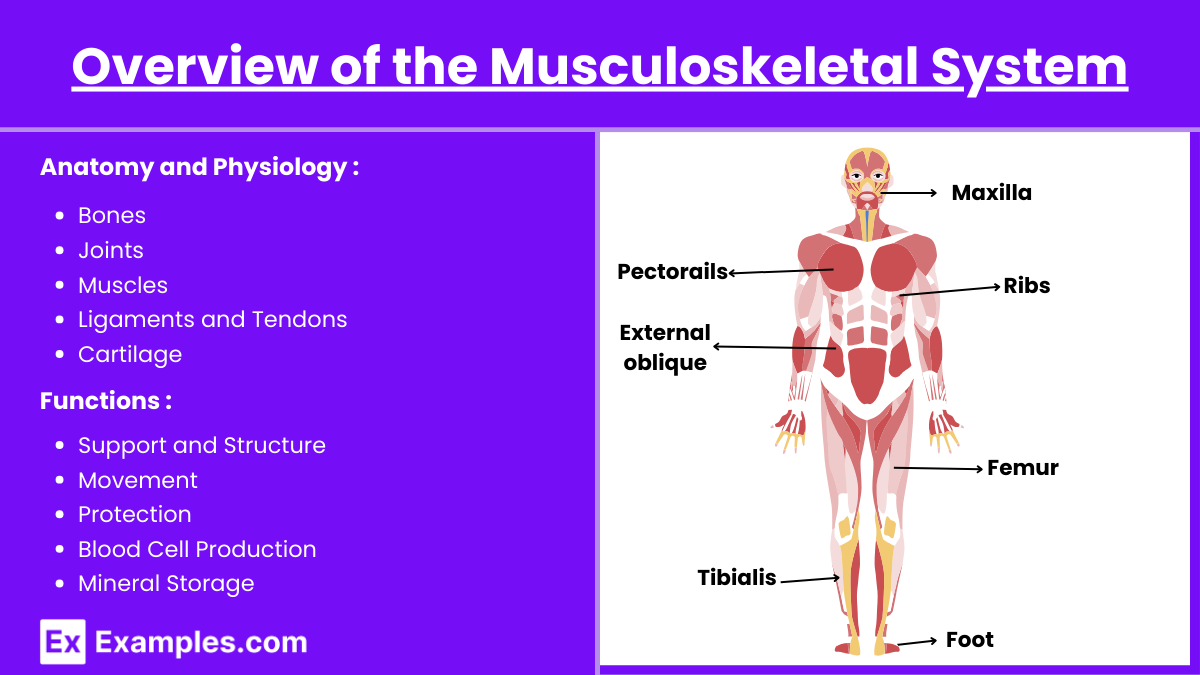
Anatomy and Physiology
The musculoskeletal system is an organ system that provides the body with structure, support, stability, and the ability to move. It is composed of bones, muscles, joints, ligaments, tendons, and cartilage. This system not only facilitates movement and locomotion but also protects vital internal organs, produces blood cells within the bone marrow, and stores essential minerals such as calcium and phosphorus.
Bones: Provide structure, protect organs, anchor muscles, and store calcium.
Joints: Connect bones, allowing movement; classified as fibrous, cartilaginous, or synovial.
Muscles: Facilitate movement through contraction; divided into skeletal, smooth, and cardiac.
Ligaments and Tendons: Ligaments connect bones to bones, while tendons connect muscles to bones.
Cartilage: Cushions joints and contributes to flexibility.
Functions
Support and Structure: Maintains body posture and structure.
Movement: Facilitates locomotion and manipulation of the environment.
Protection: Shields vital organs (e.g., skull protects the brain).
Blood Cell Production: Bone marrow produces red blood cells, white blood cells, and platelets.
Mineral Storage: Stores essential minerals like calcium and phosphorus.
Common Musculoskeletal Disorders
1. Osteoarthritis (OA)
Definition: Degenerative joint disease characterized by the breakdown of cartilage.
Common Sites: Knees, hips, hands, spine.
Symptoms: Joint pain, stiffness (especially after inactivity), swelling, decreased range of motion.
Nursing Considerations: Pain management, promoting joint mobility, patient education on weight management and exercise.
2. Rheumatoid Arthritis (RA)
Definition: Autoimmune disorder causing chronic inflammation of joints.
Common Sites: Hands, wrists, knees.
Symptoms: Joint pain, swelling, morning stiffness lasting more than 30 minutes, symmetrical joint involvement.
Nursing Considerations: Administering disease-modifying antirheumatic drugs (DMARDs), monitoring for side effects, encouraging physical activity.
3. Osteoporosis
Definition: Decreased bone density leading to fragile bones and increased fracture risk.
Risk Factors: Age, female gender, family history, low calcium/vitamin D intake, sedentary lifestyle, smoking, excessive alcohol.
Symptoms: Often asymptomatic until fracture occurs; common fractures include hip, spine, and wrist.
Nursing Considerations: Fall prevention strategies, calcium and vitamin D supplementation, weight-bearing exercises, medications like bisphosphonates.
4. Low Back Pain
Causes: Muscle strain, herniated discs, spinal stenosis, osteoarthritis.
Symptoms: Localized pain, radiating pain (sciatica), limited range of motion.
Nursing Considerations: Pain assessment, promoting proper body mechanics, physical therapy referrals, pharmacologic and non-pharmacologic pain management.
5. Sprains and Strains
Sprains: Injury to ligaments.
Strains: Injury to muscles or tendons.
Symptoms: Pain, swelling, bruising, limited movement.
Nursing Considerations: RICE protocol (Rest, Ice, Compression, Elevation), immobilization, gradual rehabilitation exercises.
6. Carpal Tunnel Syndrome
Definition: Compression of the median nerve at the wrist, leading to numbness, tingling, and weakness in the hand.
Risk Factors: Repetitive hand movements, wrist anatomy, medical conditions like diabetes.
Nursing Considerations: Wrist splinting, ergonomic adjustments, administering anti-inflammatory medications, patient education on activity modification.
Nursing Assessments
1. Health History
Pain Assessment: Utilize the OPQRST method (Onset, Provocation/Palliation, Quality, Region/Radiation, Severity, Timing).
Functional Assessment: Evaluate activities of daily living (ADLs), mobility, and independence.
Medical History: Previous musculoskeletal issues, surgeries, medications, family history.
2. Physical Examination
Inspection: Look for swelling, deformity, redness, muscle wasting.
Palpation: Assess for tenderness, temperature changes, crepitus.
Range of Motion (ROM): Active and passive ROM to determine joint flexibility.
Strength Testing: Evaluate muscle strength using the 5-grade scale (0-5).
Special Tests: Perform specific maneuvers to identify particular conditions (e.g., Lachman test for ACL integrity).
3. Diagnostic Tests
Imaging: X-rays, MRI, CT scans, bone density scans (DEXA).
Laboratory Tests: Complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), uric acid levels.
Joint Aspiration: For synovial fluid analysis in suspected infections or gout.
Examples
Example 1: Osteoarthritis (OA)
Osteoarthritis is a degenerative joint disease characterized by the gradual breakdown of cartilage, the smooth tissue that cushions the ends of bones within joints. This condition primarily affects weight-bearing joints such as the knees, hips, and spine, as well as the hands. Patients with osteoarthritis often experience joint pain, stiffness (especially after periods of inactivity), swelling, and a reduced range of motion. Management strategies include pain relief through non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy to strengthen muscles around the affected joints, weight management to decrease stress on joints, and in severe cases, surgical interventions like joint replacement.
Example 2: Rheumatoid Arthritis (RA)
Rheumatoid arthritis is an autoimmune disorder that causes chronic inflammation of the joints, leading to their eventual destruction. Unlike osteoarthritis, RA typically affects smaller joints first, such as those in the hands and wrists, and presents with symmetrical joint involvement (both sides of the body are equally affected). Common symptoms include persistent joint pain, swelling, morning stiffness lasting more than 30 minutes, and fatigue. Treatment focuses on reducing inflammation and preventing joint damage through the use of disease-modifying antirheumatic drugs (DMARDs), corticosteroids, and biologic agents. Physical therapy and regular exercise are also important to maintain joint flexibility and muscle strength.
Example 3: Osteoporosis
Osteoporosis is a condition characterized by decreased bone density and increased fragility, making bones more susceptible to fractures. It is more prevalent in older adults, particularly postmenopausal women, due to a decline in estrogen levels which are crucial for bone health. Often called a "silent disease," osteoporosis may not present noticeable symptoms until a fracture occurs, commonly in the hip, spine, or wrist. Preventive measures and management include adequate intake of calcium and vitamin D, weight-bearing and muscle-strengthening exercises, lifestyle modifications such as smoking cessation and reducing alcohol consumption, and medications like bisphosphonates that help to strengthen bone density.
Example 4: Gout
Gout is a form of inflammatory arthritis caused by the deposition of monosodium urate crystals in the joints, resulting from elevated levels of uric acid in the blood (hyperuricemia). It most frequently affects the big toe (a condition known as podagra) but can also involve other joints like the ankles, knees, and elbows. Patients typically experience sudden and severe episodes of joint pain, redness, swelling, and warmth. Acute gout attacks are managed with anti-inflammatory medications such as NSAIDs or colchicine, while long-term management focuses on lowering uric acid levels through dietary modifications (e.g., reducing purine-rich foods), maintaining a healthy weight, and using medications like allopurinol or febuxostat to prevent future attacks.
Example 5: Fractures
Fractures refer to breaks or cracks in bones and can vary in type, including closed fractures (where the skin remains intact) and open fractures (where the bone pierces the skin). Common sites for fractures include the clavicle (collarbone), wrist (distal radius), hip, and spine. Symptoms typically include intense pain at the injury site, swelling, bruising, deformity, and an inability to bear weight on the affected limb. Nursing care for fractures involves immobilization of the injured area using casts, splints, or braces to promote proper healing, pain management through medications, monitoring for complications such as impaired circulation or infection (especially in open fractures), and educating patients on care techniques and activity restrictions to facilitate recovery.
Practice Questions
Question 1
A 68-year-old female patient with osteoporosis is prescribed alendronate (Fosamax). Which of the following instructions should the nurse include to ensure the patient correctly administers this medication?
A. Take the medication with a full glass of orange juice.
B. Remain upright for at least 30 minutes after taking the medication.
C. Chew the tablet thoroughly before swallowing.
D. Take the medication at bedtime to improve absorption.
Answer: B. Remain upright for at least 30 minutes after taking the medication.
Explanation: Alendronate is a bisphosphonate used to increase bone density in patients with osteoporosis. To prevent esophageal irritation or ulceration, it is crucial that patients remain upright (sitting or standing) for at least 30 minutes after taking the medication. This helps ensure the tablet reaches the stomach quickly without lingering in the esophagus.
Option A: Alendronate should be taken with plain water, not orange juice or other beverages, as certain liquids can interfere with absorption.
Option C: The tablet should be swallowed whole with water; it should not be chewed or crushed.
Option D: Alendronate is typically taken in the morning upon waking to allow for the required period of remaining upright.
Question 2
A nurse is assessing a patient with suspected rheumatoid arthritis (RA). Which of the following signs is least consistent with RA?
A. Symmetrical joint swelling
B. Morning stiffness lasting more than one hour
C. Erosion of joint margins on X-ray
D. Osteophyte formation at joint margins
Answer: D. Osteophyte formation at joint margins
Explanation: Osteophyte formation is least consistent with rheumatoid arthritis and is more characteristic of osteoarthritis (OA). RA typically presents with:
Symmetrical joint swelling (Option A): RA commonly affects joints symmetrically, such as both hands or both knees.
Morning stiffness lasting more than one hour (Option B): Prolonged morning stiffness is a hallmark of RA, differentiating it from OA where stiffness usually lasts less than 30 minutes.
Erosion of joint margins on X-ray (Option C): RA can lead to joint erosions and narrowing of joint spaces visible on imaging studies.
Osteophyte formation at joint margins (Option D): Osteophytes, or bone spurs, are typically seen in OA due to the degenerative changes in the joint, not in RA.
Question 3
A patient presents to the emergency department with a suspected closed fracture of the distal radius. Which of the following interventions should the nurse perform first?
A. Apply ice to reduce swelling
B. Administer prescribed analgesics
C. Immobilize the fracture with a splint
D. Perform a neurovascular assessment
Answer: D. Perform a neurovascular assessment
Explanation: In the management of fractures, especially in the acute setting, ensuring the integrity of neurovascular status is the priority.
Option A (Apply ice): While reducing swelling is important, it should not precede the assessment of neurovascular status.
Option B (Administer analgesics): Pain management is essential but secondary to ensuring there is no immediate threat to neurovascular function.
Option C (Immobilize the fracture with a splint): Immobilization is necessary but should be done after confirming that there is no neurovascular compromise.