The neurologic system is a vital organ system responsible for controlling and coordinating all bodily functions, including movement, sensation, cognition, and autonomic processes. It consists of the central nervous system (CNS), which includes the brain and spinal cord, and the peripheral nervous system (PNS), made up of cranial and spinal nerves. This system processes sensory input, initiates motor responses, and maintains homeostasis. Proper functioning of the neurologic system is essential for survival, and any disruptions can lead to severe conditions such as strokes, seizures, and traumatic brain injuries.
Learning Objectives
In studying "Adult Health: Neurologic" for the NCLEX-PN® Exam, you should learn to understand the anatomy and physiology of the neurologic system, including the brain, spinal cord, peripheral nerves, and cranial nerves. Analyze common neurologic conditions such as strokes, seizures, traumatic brain injuries (TBI), meningitis, multiple sclerosis (MS), and Parkinson’s disease, focusing on pathophysiology, clinical manifestations, and treatment options. Evaluate nursing considerations like patient assessment, neuro checks, seizure precautions, and monitoring for increased intracranial pressure (ICP). Explore pharmacological interventions, including anticonvulsants, antiplatelets, and diuretics. Apply your knowledge to respond effectively to neurologic-related scenarios, ensuring patient safety and prioritizing care in NCLEX-PN® exam questions.
1. Overview of the Neurologic System
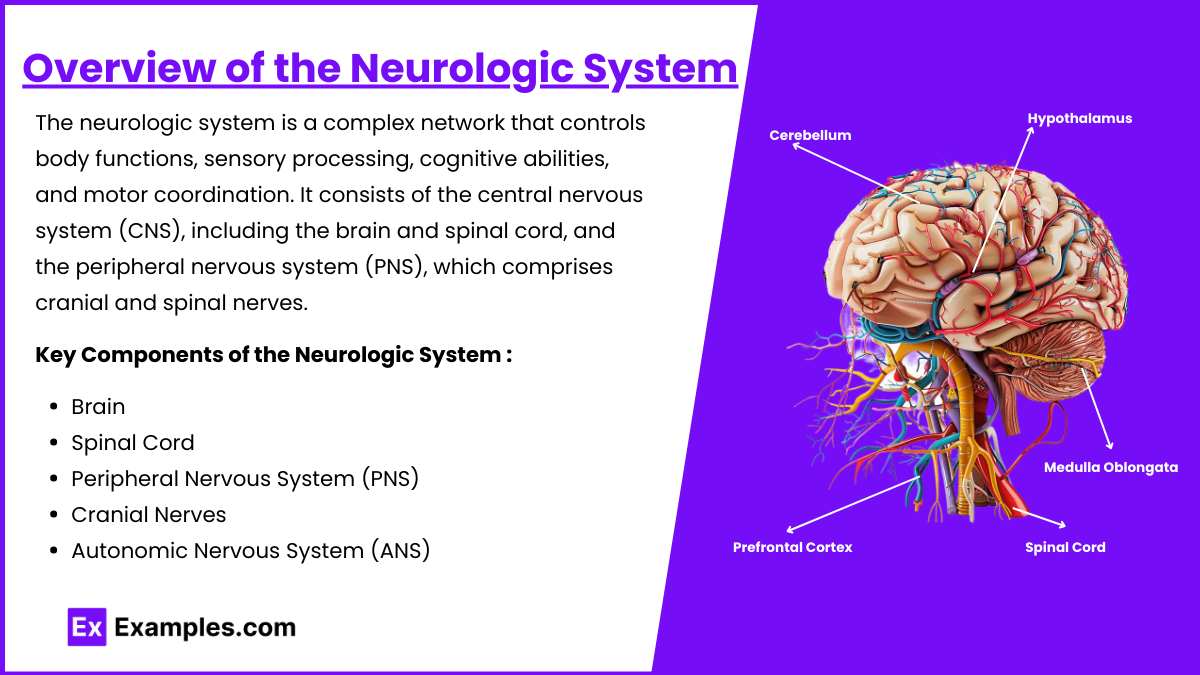
The neurologic system is a complex network that controls body functions, sensory processing, cognitive abilities, and motor coordination. It consists of the central nervous system (CNS), including the brain and spinal cord, and the peripheral nervous system (PNS), which comprises cranial and spinal nerves. This system governs voluntary and involuntary actions, making it vital for maintaining homeostasis.
Central Nervous System (CNS): Composed of the brain and spinal cord.
Peripheral Nervous System (PNS): Includes cranial and spinal nerves that connect the CNS to the rest of the body.
Key Components of the Neurologic System
Brain: The control center for body functions, cognition, memory, and emotions. It has four major lobes:
Frontal Lobe: Controls reasoning, emotions, problem-solving, and voluntary movement.
Parietal Lobe: Processes sensory information like touch, pressure, pain, and temperature.
Temporal Lobe: Responsible for hearing, memory, and language comprehension.
Occipital Lobe: Handles visual processing.
Spinal Cord: Transmits motor, sensory, and reflex information between the brain and body. It also controls reflexes (e.g., withdrawal from pain).
Peripheral Nervous System (PNS): Comprises the somatic nervous system (controls voluntary movement) and autonomic nervous system (controls involuntary functions like heart rate, respiration, and digestion).
Cranial Nerves: There are 12 cranial nerves responsible for sensory and motor functions, such as smell, sight, taste, and hearing.
Autonomic Nervous System (ANS): Divided into the sympathetic nervous system ("fight or flight") and the parasympathetic nervous system ("rest and digest").
2. Common Neurologic Disorders
Neurologic disorders can impair sensory perception, motor control, and cognitive function. As an LPN, you must identify signs and symptoms, provide appropriate nursing care, and ensure patient safety. Here are some key neurologic disorders you need to master for the NCLEX-PN® exam.
Stroke (Cerebrovascular Accident - CVA)
Occurs when blood flow to a part of the brain is interrupted due to a clot (ischemic) or bleeding (hemorrhagic). Interruption of blood flow to the brain causing motor, sensory, and cognitive impairments.
Symptoms (FAST):
Facial drooping
Arm weakness
Speech difficulties
Time to call emergency services
Interventions:
Elevate the head of the bed (HOB) 30 degrees to prevent increased intracranial pressure (ICP).
Monitor for increased ICP (headache, confusion, altered mental status).
Administer thrombolytic agents (e.g., alteplase) for ischemic stroke if prescribed.
Seizure Disorders (Epilepsy)
Abnormal electrical discharges in the brain leading to seizures. Sudden, uncontrolled electrical activity in the brain leading to convulsions or altered awareness.
Types:
Generalized Seizures (entire brain affected)
Focal Seizures (only one part of the brain affected)
Nursing Interventions:
During a seizure: Protect the airway, place the patient on their side, do not restrain, do not place objects in the mouth.
After a seizure: Check for breathing and consciousness, reorient the patient, document seizure activity.
Medications: Administer phenytoin, valproic acid, or carbamazepine as prescribed.
Parkinson’s Disease
A neurodegenerative disorder caused by the depletion of dopamine in the brain.Progressive neurodegenerative disorder affecting movement and muscle control.
Symptoms (TRAP):
Tremors (resting tremors)
Rigidity (stiff muscles)
Akinesia or Bradykinesia (slow movement)
Postural instability (loss of balance)
Nursing Interventions:
Encourage slow, deliberate movements.
Administer levodopa/carbidopa to restore dopamine balance.
Use assistive devices like canes or walkers to prevent falls.
Alzheimer’s Disease
Cognitive decline and memory loss due to neurodegeneration.
Stages: Early, middle, and late stages.
Symptoms: Memory loss, confusion, wandering, personality changes.
Nursing Interventions:
Maintain familiar environments to prevent confusion.
Use bed alarms and fall prevention strategies.
Administer cholinesterase inhibitors (donepezil) to slow cognitive decline.
3. Nursing Interventions for Neurologic Disorders
Effective nursing care for neurologic conditions focuses on maintaining safety, promoting mobility, and ensuring airway patency. Key nursing interventions include:
Airway and Breathing Support: Maintain an open airway, position the patient appropriately (e.g., head of bed elevated 30 degrees).
Seizure Precautions: Pad the side rails, have oxygen and suction available, and turn the patient on their side to prevent aspiration.
Neurological Assessment: Regularly check level of consciousness (LOC) using the Glasgow Coma Scale (GCS).
Infection Control: For meningitis, use isolation precautions and administer antibiotics as prescribed.
Medication Administration: Administer anticonvulsants, antiplatelets, levodopa, and cholinesterase inhibitors as required.
Patient Education: Teach patients and families about safety measures, fall prevention, and medication adherence.
Examples
Example 1: Stroke (Cerebrovascular Accident - CVA)
A stroke occurs when the blood supply to a part of the brain is interrupted, either by a blood clot (ischemic stroke) or ruptured blood vessel (hemorrhagic stroke). Symptoms can be remembered using the FAST mnemonic (Face drooping, Arm weakness, Speech difficulty, Time to call emergency services). Nursing interventions focus on maintaining airway, breathing, and circulation, controlling blood pressure, and administering thrombolytics like alteplase (tPA) for ischemic strokes. Nurses must also monitor for signs of increased intracranial pressure (ICP), such as headache, confusion, and altered mental status. Rehabilitative care often involves speech, occupational, and physical therapy to restore mobility, cognitive function, and swallowing ability.
Example 2: Seizure Disorders (Epilepsy)
Seizures are caused by abnormal electrical activity in the brain, resulting in convulsions, loss of consciousness, or temporary confusion. Generalized seizures affect the whole brain, while focal seizures affect one part of the brain. During a seizure, the nurse's priority is to ensure the patient's safety. This involves placing the patient in a side-lying position to prevent aspiration, padding the side rails, and ensuring no objects are in the patient's mouth. After the seizure (postictal phase), the nurse should check for airway patency, monitor vital signs, and document the event. Medications like phenytoin, valproic acid, and carbamazepine are often used to manage seizures. Nurses should educate patients on medication adherence and triggers that may provoke seizures, such as stress, flashing lights, or sleep deprivation.
Example 3: Parkinson’s Disease
This is a chronic, progressive neurodegenerative disorder caused by low levels of dopamine in the brain. Patients often experience tremors, rigidity, bradykinesia (slow movement), and postural instability. The hallmark symptoms are remembered using the TRAP mnemonic (Tremor, Rigidity, Akinesia, Postural instability). Nurses must promote fall prevention strategies since patients have balance issues and a shuffling gait. Pharmacologic interventions involve levodopa-carbidopa to increase dopamine levels in the brain, which reduces symptoms. Nurses also encourage patients to engage in slow, deliberate movements, use assistive devices (like walkers or canes), and engage in physical therapy to maintain independence in daily living activities.
Example 4: Alzheimer’s Disease
Alzheimer’s is a progressive neurodegenerative disease characterized by cognitive decline, memory loss, confusion, and personality changes. The disease progresses in three stages: early, middle, and late. Early signs include forgetfulness and misplacing items, while later stages involve disorientation, incontinence, and total dependence on caregivers. Nurses must provide a safe and familiar environment to prevent confusion and wandering. This includes using bed alarms, installing grab bars, and encouraging the use of memory aids like clocks, calendars, and labels. Medications like cholinesterase inhibitors (donepezil) help slow cognitive decline. Nurses educate family members on caregiver support since Alzheimer’s disease requires long-term care and support.
Example 5: Meningitis
Meningitis refers to the inflammation of the meninges (the protective layers surrounding the brain and spinal cord) and can be caused by bacteria, viruses, or fungi. Bacterial meningitis is life-threatening and requires immediate intervention. Symptoms include severe headache, neck stiffness (nuchal rigidity), photophobia (light sensitivity), fever, and altered mental status. Nurses must place the patient in droplet precautions for bacterial meningitis to prevent the spread of infection. Lumbar puncture (spinal tap) is the key diagnostic test used to identify the causative organism. Interventions focus on administering IV antibiotics, managing fever, and monitoring for signs of increased ICP (headache, bradycardia, irregular breathing). The nurse should ensure the patient remains calm and in a dark, quiet environment to prevent sensory overload and agitation.
Practice Questions
Question 1
A nurse is caring for a patient who is suspected of having a stroke. Which of the following is the nurse's priority action?
A) Check the patient’s blood glucose level.
B) Obtain a complete health history from the patient.
C) Position the patient flat on the bed.
D) Notify the healthcare provider immediately.
Answer: A) Check the patient’s blood glucose level.
Explanation:
When a stroke is suspected, it is essential to quickly identify the type of stroke (ischemic vs. hemorrhagic) and rule out other conditions, like hypoglycemia, which can present with similar symptoms (confusion, slurred speech, and altered mental status). Checking the blood glucose level is a rapid, non-invasive step that can prevent unnecessary delays in treatment.
Option A: Correct. Hypoglycemia can mimic stroke symptoms, and it must be ruled out immediately. If blood glucose is low, treatment for hypoglycemia is initiated, not stroke management.
Option B: Incorrect. While a health history is essential, it does not take precedence over ruling out life-threatening causes like hypoglycemia.
Option C: Incorrect. Placing the patient flat can increase intracranial pressure (ICP). Typically, the head of the bed is elevated to 30 degrees to promote venous drainage and reduce ICP.
Option D: Incorrect. Notifying the provider is necessary, but the nurse must first assess for critical conditions like hypoglycemia before escalating care.
Question 2
A patient with a history of seizures suddenly begins having a generalized tonic-clonic seizure while in bed. Which nursing intervention should the nurse perform first?
A) Place a padded tongue blade in the patient’s mouth.
B) Turn the patient on their side.
C) Hold the patient down to prevent injury.
D) Call for emergency medical assistance.
Answer: B) Turn the patient on their side.
Explanation:
The nurse’s priority action during a seizure is to ensure patient safety and prevent aspiration. Turning the patient on their side prevents aspiration of saliva, mucus, or vomit, which can occur during the postictal phase (after the seizure). This position also promotes an open airway.
Option A: Incorrect. Placing any object (like a tongue blade) in the patient’s mouth during a seizure is dangerous as it can cause injury, break teeth, or obstruct the airway.
Option B: Correct. Turning the patient on their side maintains an open airway and reduces the risk of aspiration. This is the standard of care for patients experiencing a seizure.
Option C: Incorrect. Restraining a patient during a seizure increases the risk of injury and may cause harm to both the nurse and the patient.
Option D: Incorrect. While calling for help is essential, ensuring the patient’s safety is the immediate priority.
Question 3
A nurse is caring for a patient with a traumatic brain injury (TBI). Which of the following indicates a possible increase in intracranial pressure (ICP)?
A) Bradycardia, hypertension, and irregular respirations.
B) Tachycardia, hypotension, and increased respiratory rate.
C) Low-grade fever, bradycardia, and hyperactivity.
D) Confusion, bradycardia, and increased urine output.
Answer: A) Bradycardia, hypertension, and irregular respirations.
Explanation:
Bradycardia (slow heart rate)
Hypertension (increased systolic pressure with widening pulse pressure)
Irregular respirations (also called Cheyne-Stokes breathing or ataxic breathing)
These changes occur because increased pressure on the brainstem affects vital centers controlling heart rate, blood pressure, and respiration.
Option A: Correct. These signs reflect Cushing’s Triad, which is a late sign of increased ICP. Bradycardia, irregular breathing, and hypertension indicate compression of the brainstem.
Option B: Incorrect. Tachycardia and hypotension are signs of hypovolemic shock, not increased ICP.
Option C: Incorrect. Fever can occur due to damage to the hypothalamus, but bradycardia and hyperactivity are not typical signs of increased ICP.
Option D: Incorrect. Confusion is a sign of increased ICP, but bradycardia and increased urine output are not hallmark signs of elevated ICP.