Luxurious products and services whether they be a spa, a resort, or a high-class residential apartment can give off a distant feeling to a lot of people. One way to reach out to them is by using promotional materials that make them more accessible to the public, and one way to do that is by making a beautiful luxury brochure!
[bb_toc content=”][/bb_toc]
10+ Beautiful Luxury Brochure Examples
1. Luxury Resort Bi-fold Brochure Template
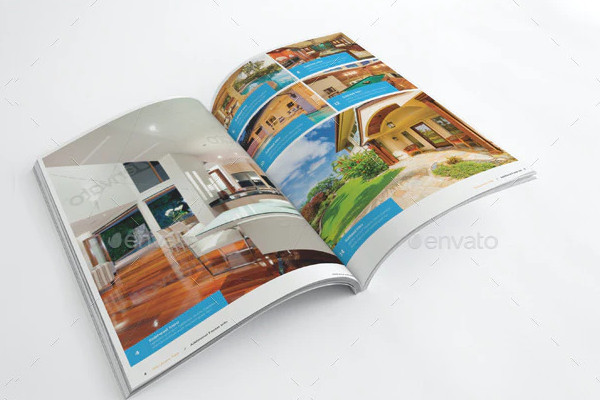
2. Luxury Property Management Bi-Fold Brochure Template
3. Luxury Real Estate Broker Tri-Fold Brochure Template

4. Luxury Real Estate Agent Agency Tri-Fold Brochure Template
5. Free Luxury Hotel Tri-Fold Template
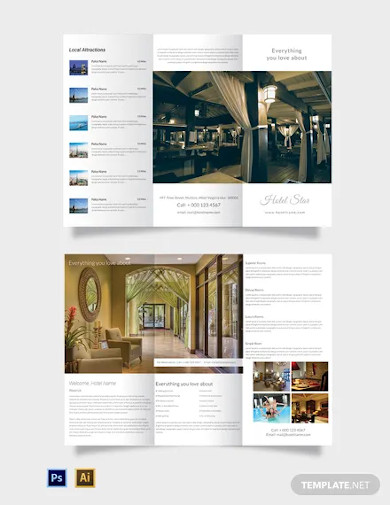
6. Free Luxury Hotel Bi-Fold Template

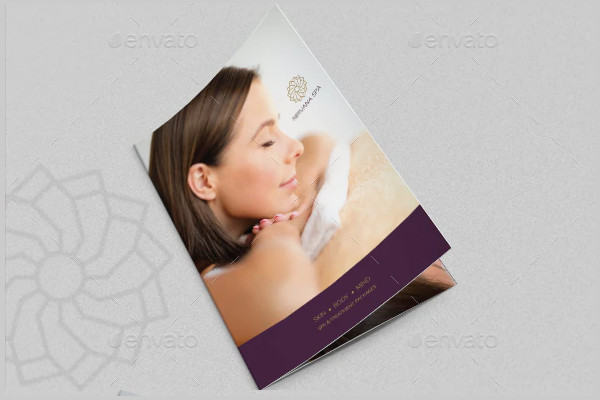
7. Luxury Spa Brochure
8. Luxury Hotel Brochure

9. Luxury Retro Brochure Tri-fold
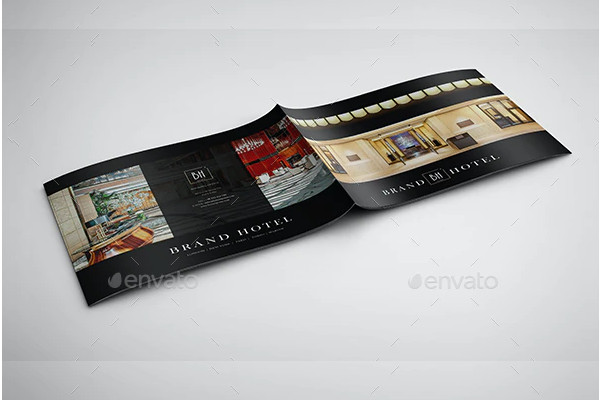
10. Luxury Hotel Landscape Brochure
11. Luxury Real Estate Brochure
What is a Luxury Brochure?
A luxury brochure is a brochure specifically used as an advertising tool for luxurious items and services such as a penthouse apartment, a hotel business, or a restaurant business. These brochure designs are specifically made for audiences who can afford high-class products and services.
How to Create a Beautiful Luxury Brochure?
While there are various luxury brochure templates to choose one, making one on your own is a pretty simple endeavor. Take note of these five steps when creating a luxury brochure.
1.) Know Your Audience
Recognizing who you are making this brochure for is a good way to start. Once you realize who your audience is, you can easily figure out what your content should be and how you can make it effective. For example, if you want to make a luxury hotel brochure, determine first if it is aimed exclusively at high-class, tourists, or for anybody who can afford it, that way you can add the appropriate type of content to draw those customers in.
2.) Choose the Layout
Pick the layout of your luxury brochure before you start with any of the content. Choose the type of layout suitable for your content and the aesthetic you are going for. For example, if you are making a luxury real estate property brochure, choose a layout where you are able to add photos, and text in an organized manner on your pages making the perfect real estate brochure layout. Of course, also consider whether your layout will be a bi-fold or a tri-fold brochure.
3.) Add Images
When it comes to advertising luxurious goods and services, sometimes pictures are all you need to get clients interested. So add photos of whatever luxury-related things you are promoting. For example, if you are advertising a luxury resort, then add photos of the resort’s facilities like the swimming pool, the spa, the rooms, etc.
4.) Include Graphic Designs
Place graphic designs to enhance the aesthetic of your brochure. People generally have short attention spans when looking through promotional materials such as brochures, so adding graphics to the pages will certainly grab their attention. Make the graphics go with the luxury theme of your content.
5.) Keep Written Content Concise
Lastly, make your written content short and understandable. Depending on your audience, most of them won’t likely be expecting a high vocabulary on a brochure. Keep it simple and straight to the point. if you are promoting a luxury jewelry business, then talk about what sort of jewelry and other products they’ll find there and avoid going on a tangent about how great it is to wear jewelry.
FAQs
What is the difference between a luxury brochure and a luxury flyer?
A luxury brochure has more content on its pages in comparison to a luxury flyer.
What are luxury brochures used for specifically?
Luxury brochures are specifically used to inform potential clients who are interested in getting themselves the luxurious goods and services that the brochure promotes in the first place.
Who writes the luxury brochure content?
Content of luxury brochures tends to be created by the company’s marketing or advertising department since they know how to attract clients to the business they work for.
With a well-written luxury brochure, you can attract clients who will want to buy what you are selling, which in turn can lead to huge profits considering the prices of such luxury. If you want any more references, feel free to check out our other brochure templates.