The “Adult Health: Respiratory” section of the NCLEX-PN® exam focuses on critical respiratory concepts essential for patient care. This section emphasizes the assessment, management, and treatment of respiratory disorders such as COPD, asthma, pneumonia, tuberculosis, and pulmonary embolism. Key areas include airway management, oxygenation, ventilation, infection control, and diagnostic testing (e.g., ABGs, pulse oximetry). Practical nurses must prioritize interventions using the ABC approach (Airway, Breathing, Circulation) to ensure patient safety. Mastery of these concepts is crucial for achieving a high score on the NCLEX-PN®.
Learning Objectives
In studying “Adult Health: Respiratory” for the NCLEX-PN® Exam, you should learn to understand the anatomy and physiology of the respiratory system, including the lungs, airways, alveoli, and respiratory muscles. Analyze common respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), pneumonia, tuberculosis (TB), pulmonary embolism (PE), and acute respiratory distress syndrome (ARDS), focusing on pathophysiology, clinical manifestations, and treatment options. Evaluate nursing considerations such as airway management, oxygen therapy, suctioning, breathing techniques, and infection control measures. Explore pharmacological interventions, including bronchodilators, corticosteroids, and oxygen therapy. Apply knowledge to prioritize care, ensure patient safety, and respond effectively to respiratory-related scenarios.
Respiratory System
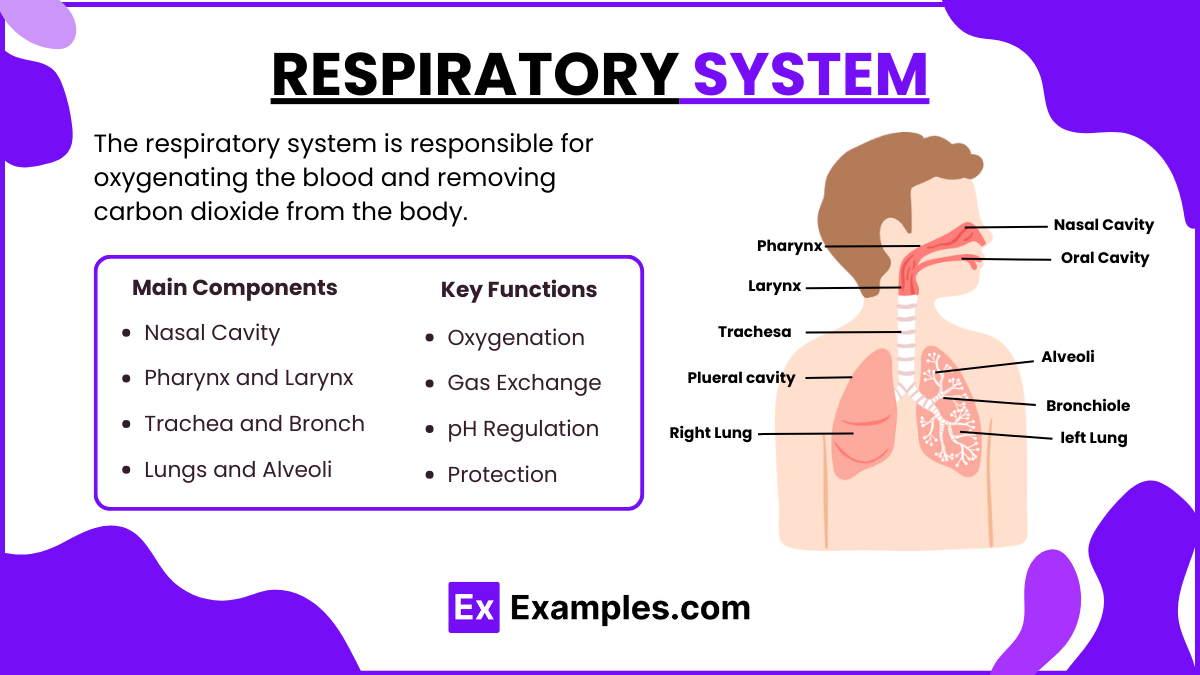
The respiratory system is responsible for oxygenating the blood and removing carbon dioxide from the body. It includes the upper and lower respiratory tracts, lungs, and alveoli where gas exchange occurs.
The main components include:
- Nasal Cavity: Filters, warms, and humidifies air.
- Pharynx and Larynx: Channels air to the trachea; the larynx also produces sound.
- Trachea and Bronchi: Air passages leading to the lungs.
- Lungs and Alveoli: Facilitate oxygen and carbon dioxide exchange.
Key Functions of the Respiratory System
- Oxygenation: Delivers oxygen to tissues and organs.
- Gas Exchange: Exhales carbon dioxide as a waste product.
- pH Regulation: Maintains the body’s acid-base balance.
- Protection: Traps particles with cilia and mucus.
Common Respiratory Disorders
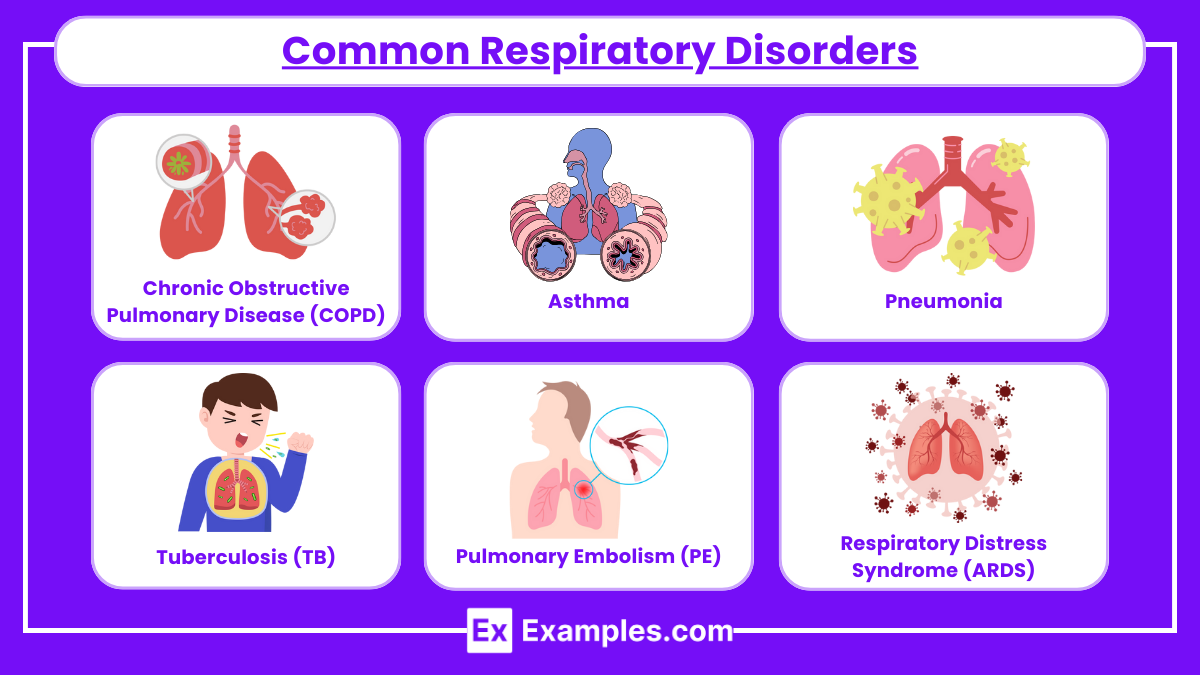
1.Chronic Obstructive Pulmonary Disease (COPD)
- Description: Progressive, irreversible lung disease (chronic bronchitis + emphysema).
- Symptoms: Chronic cough, dyspnea, wheezing, cyanosis, and sputum production.
- Nursing Interventions:
- Positioning: High Fowler’s to improve breathing.
- Oxygen Therapy: Use low-flow oxygen to prevent CO2 retention.
- Medications: Bronchodilators, corticosteroids, and mucolytics.
- Patient Education: Smoking cessation, breathing exercises, and pursed-lip breathing.
2. Asthma
- Description: Reversible airway obstruction due to inflammation, bronchoconstriction, and mucus production.
- Symptoms: Wheezing, shortness of breath (SOB), chest tightness, and coughing.
- Nursing Interventions:
- Monitor: Peak expiratory flow rate (PEFR) to assess severity.
- Medications: Inhaled beta-agonists (albuterol) for rescue, corticosteroids for maintenance.
- Patient Education: Use of inhalers, avoid allergens, and manage triggers (e.g., dust, pollen, pet dander).
3. Pneumonia
- Description: Infection of the lungs (bacterial, viral, or fungal) causing inflammation and fluid accumulation.
- Symptoms: Productive cough, fever, chills, dyspnea, pleuritic chest pain, and crackles on auscultation.
- Nursing Interventions:
- Positioning: Elevate head of the bed (HOB) to 30-45 degrees.
- Medications: Administer antibiotics, antipyretics, and analgesics.
- Infection Control: Hand hygiene, PPE, and isolation (if necessary).
- Patient Education: Encourage coughing, deep breathing, and adequate hydration.
4. Tuberculosis (TB)
- Description: Airborne infection caused by Mycobacterium tuberculosis.
- Symptoms: Persistent cough (≥ 3 weeks), night sweats, weight loss, and hemoptysis.
- Nursing Interventions:
- Isolation Precautions: Airborne precautions (N95 mask, negative pressure room).
- Medications: Anti-TB drugs (Rifampin, Isoniazid) for 6-12 months.
- Monitoring: Sputum culture to confirm negative status.
- Patient Education: Adherence to medication regimen and follow-up sputum tests.
5. Pulmonary Embolism (PE)
- Description: Blockage of pulmonary arteries by a blood clot, fat, or air embolism.
- Symptoms: Sudden dyspnea, chest pain, tachypnea, and hypoxia.
- Nursing Interventions:
- Positioning: High Fowler’s position.
- Oxygen Therapy: Administer oxygen as prescribed.
- Medications: Anticoagulants (heparin, warfarin) and thrombolytics.
- Patient Education: Avoid prolonged immobility, use compression devices, and recognize DVT signs.
6. Respiratory Distress Syndrome (ARDS)
- Description: Fluid accumulation in alveoli leading to hypoxemia.
- Symptoms: Severe dyspnea, crackles, cyanosis, and decreased oxygen saturation.
- Nursing Interventions:
- Ventilatory Support: Use of mechanical ventilation with PEEP.
- Medications: Diuretics, antibiotics, and corticosteroids.
- Positioning: Prone position improves oxygenation.
- Patient Monitoring: Close monitoring of ABGs, SpO2, and respiratory status.
Diagnostic Tests for Respiratory Disorders
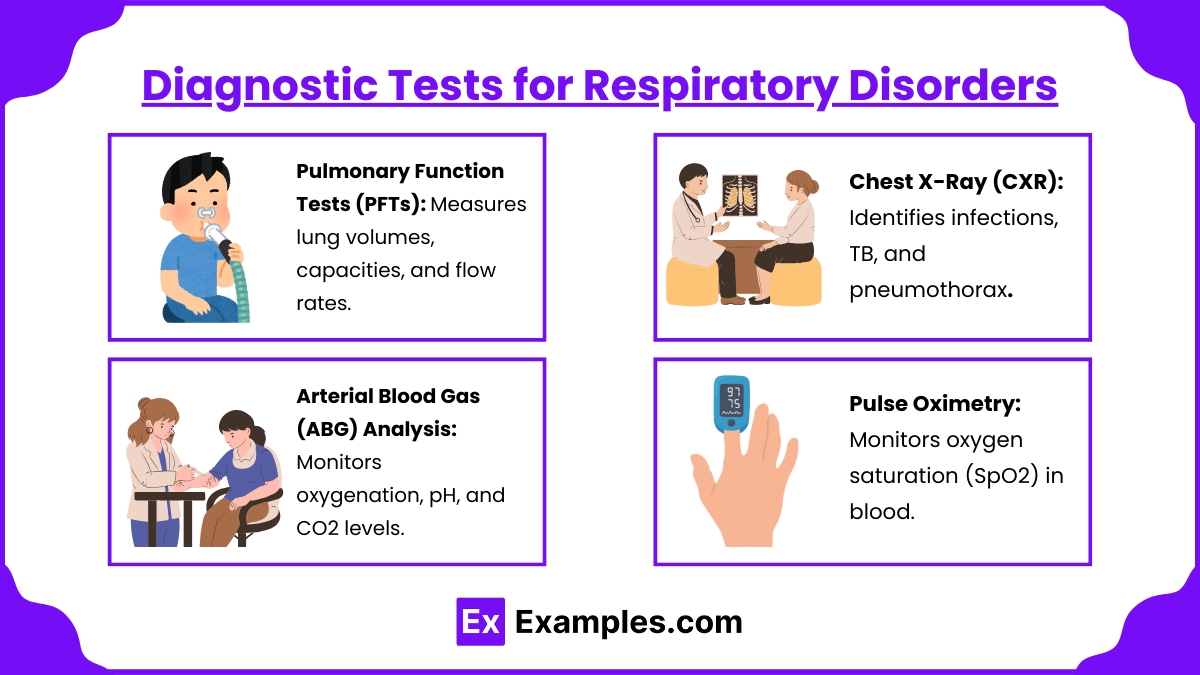
Accurate diagnosis of respiratory disorders is essential for effective treatment and management. The NCLEX PN® exam requires nurses to understand common diagnostic tests, their purposes, procedures, and expected results. Here are the key diagnostic tests used in the evaluation of respiratory conditions:
- Pulmonary Function Tests (PFTs): Measures lung volumes, capacities, and flow rates.
- Chest X-Ray (CXR): Identifies infections, TB, and pneumothorax.
- Arterial Blood Gas (ABG) Analysis: Monitors oxygenation, pH, and CO2 levels.
- Pulse Oximetry: Monitors oxygen saturation (SpO2) in blood.
Examples
Example 1: Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a progressive, irreversible lung disease that includes chronic bronchitis and emphysema. It is primarily caused by long-term exposure to irritants like cigarette smoke and air pollutants. Symptoms include chronic cough, sputum production, dyspnea, and wheezing. Nursing interventions involve positioning the patient in high Fowler’s position to facilitate breathing, administering low-flow oxygen to prevent CO2 retention, and teaching pursed-lip breathing to improve oxygenation. Medications such as bronchodilators, corticosteroids, and mucolytics are used to manage symptoms. Nurses must educate patients on smoking cessation, infection prevention, and the proper use of inhalers. Pulmonary rehabilitation, including physical exercises and breathing techniques, is essential for improving quality of life.
Example 2: Asthma
Asthma is a chronic, reversible airway disorder marked by bronchoconstriction, airway inflammation, and increased mucus production. It is often triggered by allergens, respiratory infections, exercise, or irritants like smoke and dust. Symptoms include shortness of breath (dyspnea), wheezing, chest tightness, and coughing, especially at night or early morning. Nursing interventions include administering rescue inhalers (like albuterol) to relieve acute bronchospasms and using corticosteroids to reduce inflammation. Nurses should monitor the patient’s peak expiratory flow rate (PEFR) and educate them on trigger avoidance, inhaler use, and early recognition of warning signs of an asthma attack. In severe cases, oxygen therapy may be required. Patients should be taught to use a spacer with their inhaler for better medication delivery.
Example 3: Pneumonia
Pneumonia is an infection that inflames the air sacs (alveoli) in the lungs, leading to fluid or pus accumulation. It can be caused by bacteria, viruses, or fungi. Symptoms include fever, chills, productive cough with yellow or green sputum, dyspnea, chest pain, and crackles heard during auscultation. Nursing interventions include promoting lung expansion through incentive spirometry, elevating the head of the bed to improve breathing, and administering oxygen therapy as needed. Medications such as antibiotics, antipyretics, and analgesics are used to treat bacterial pneumonia. Nurses should monitor for signs of respiratory distress, assess the patient’s oxygen saturation (SpO2), and encourage hydration to loosen secretions. Proper hand hygiene and infection control measures are crucial in preventing the spread of pneumonia.
Example 4: Tuberculosis (TB)
Tuberculosis (TB) is a highly contagious airborne infection caused by Mycobacterium tuberculosis. It primarily affects the lungs but can also spread to other organs. Symptoms include a persistent cough lasting more than three weeks, night sweats, fatigue, weight loss, hemoptysis (coughing up blood), and chest pain. Nursing interventions focus on placing the patient under airborne precautions, including the use of N95 masks and a negative pressure isolation room. Nurses must administer anti-tuberculosis medications, such as isoniazid (INH), rifampin (RIF), and ethambutol (EMB), for a treatment period of 6-12 months. The nurse should educate the patient about medication adherence and the importance of follow-up sputum tests. Monitoring for liver toxicity and visual changes caused by these medications is essential during treatment.
Example 5: Acute Respiratory Distress Syndrome (ARDS)
Acute Respiratory Distress Syndrome (ARDS) is a life-threatening condition characterized by sudden, severe respiratory failure due to fluid buildup in the alveoli. It often results from sepsis, trauma, pneumonia, or inhalation injury. Symptoms include severe dyspnea, hypoxemia (low blood oxygen), tachypnea (rapid breathing), and cyanosis (bluish skin). Nursing interventions focus on providing mechanical ventilation with positive end-expiratory pressure (PEEP) to keep alveoli open. Nurses must closely monitor arterial blood gas (ABG) values to assess oxygenation and carbon dioxide levels. Medications like diuretics, antibiotics, and corticosteroids are administered to reduce fluid and treat infection. Patients are often placed in a prone position to improve oxygenation, and continuous monitoring of lung sounds and respiratory effort is required. Nurses must also provide emotional support to patients and families due to the critical nature of the condition.
Practice Questions
Question 1
A patient with chronic obstructive pulmonary disease (COPD) is admitted to the emergency department with complaints of shortness of breath, wheezing, and increased respiratory rate. Which of the following interventions should the nurse prioritize first?
A. Administer a prescribed oral corticosteroid.
B. Place the patient in a high Fowler’s position.
C. Call the healthcare provider to request a chest X-ray.
D. Encourage the patient to perform pursed-lip breathing.
Answer: B. Place the patient in a high Fowler’s position.
Explanation
This question assesses your understanding of airway and breathing prioritization. The NCLEX PN® requires test-takers to apply the ABC framework (Airway, Breathing, Circulation) when answering prioritization questions. Here’s the rationale for each option:
- Option A: Administer a prescribed oral corticosteroid – While corticosteroids reduce inflammation, they do not act immediately. This intervention is important but not the priority.
- Option B: Place the patient in a high Fowler’s position – Correct answer. Placing the patient in a high Fowler’s position helps maximize lung expansion, promotes better oxygenation, and is the fastest intervention.
- Option C: Call the healthcare provider to request a chest X-ray – Although a chest X-ray might be necessary to rule out complications (like pneumonia), it is not an immediate intervention to improve oxygenation.
- Option D: Encourage the patient to perform pursed-lip breathing – Pursed-lip breathing helps manage dyspnea, but positioning is faster and more effective for immediate relief.
Question 2
A nurse is caring for a patient with pneumonia who has an oxygen saturation (SpO₂) of 85% on room air. Which of the following oxygen delivery devices should the nurse choose to improve oxygenation?
A. Nasal cannula at 2 L/min.
B. Simple face mask at 8 L/min.
C. Non-rebreather mask at 15 L/min.
D. Venturi mask at 24% FiO₂.
Answer: C. Non-rebreather mask at 15 L/min.
Explanation
This question assesses your knowledge of oxygen delivery devices and when to use them. Here’s the rationale for each option:
- Option A: Nasal cannula at 2 L/min – This delivers low-flow oxygen (24-28%) and is used for mild hypoxemia, but an SpO₂ of 85% requires immediate, high-concentration oxygen.
- Option B: Simple face mask at 8 L/min – A simple mask provides oxygen at 40-60% FiO₂, which may not be sufficient for SpO₂ as low as 85%.
- Option C: Non-rebreather mask at 15 L/min – Correct answer. The non-rebreather mask delivers the highest oxygen concentration (up to 90-100%) without intubation. It is appropriate for patients with severe hypoxemia.
- Option D: Venturi mask at 24% FiO₂ – This option delivers a precise oxygen concentration but is not appropriate for a patient with an SpO₂ of 85%, as it is too low.
Question 3
A nurse is assigned to care for a patient with suspected tuberculosis (TB). Which of the following nursing actions is the highest priority to prevent the spread of infection?
A. Place the patient in a private room with contact precautions.
B. Instruct the patient to wear a surgical mask during transport.
C. Place the patient in a negative pressure room with airborne precautions.
D. Require visitors to wear a surgical mask when visiting the patient.
Answer: C. Place the patient in a negative pressure room with airborne precautions.
Explanation
This question tests your knowledge of infection control precautions related to tuberculosis. Here’s the rationale for each option:
- Option A: Place the patient in a private room with contact precautions – While isolation is necessary, contact precautions are incorrect. TB requires airborne precautions because it spreads via respiratory droplets that remain suspended in the air.
- Option B: Instruct the patient to wear a surgical mask during transport – While this is an important action when transporting the patient, the higher priority is to place the patient in a negative pressure room.
- Option C: Place the patient in a negative pressure room with airborne precautions – Correct answer. This is the highest priority action because airborne precautions prevent the spread of the TB pathogen via tiny airborne droplets. This includes using N95 masks and negative pressure ventilation.
- Option D: Require visitors to wear a surgical mask when visiting the patient – Visitors should wear an N95 respirator, not a surgical mask, when visiting a patient with suspected TB.