Quickly and accurately convert micrograms to pounds and vice versa with Examples.com. Simply enter your values to get conversion results.
Microgram to Pound
Formula: Mass in Pound (lb) = Mass in Microgram (μg) × 2.205×10-9
| Microgram | Pound |
|---|---|
| 1 | 2.2046e-9 |
Pound to Microgram
Formula: Mass in Microgram (μg) = Mass in Pound (lb) × 4.536×108
| Pound | Microgram |
|---|---|
| 1 | 4.53592e8 |
Mass Converters to Microgram (µg)
| Tonne to Microgram | Kilogram to Microgram | Gram to Microgram |
| Milligram to Microgram | Imperial ton to Microgram | US ton to Microgram |
| Stone to Microgram | Pound to Microgram | Ounce to Microgram |
Mass Converters to Pound (lb)
| Tonne to Pound | Kilogram to Pound | Gram to Pound |
| Milligram to Pound | Microgram to Pound | Imperial ton to Pound |
| US ton to Pound | Stone to Pound | Ounce to Pound |
Conversion Factors:
- Micrograms to Pounds: 1 pound = 453,592,370 micrograms
- Pounds to Micrograms: 1 microgram = 0.00000000220462 pounds
How to Convert Micrograms to Pounds:
To convert micrograms to pounds, use the multiplication formula:
Pounds=Micrograms×0.00000000220462
Example: Convert 5,000,000 micrograms to pounds:
Pounds=5,000,000×0.00000000220462=0.0110231 pounds
How to Convert Pounds to Micrograms:
To convert pounds to micrograms, use the multiplication formula:
Micrograms=Pounds×453,592,370
Example: Convert 3 pounds to micrograms:
Micrograms=3×453,592,370=1,360,777,110 micrograms
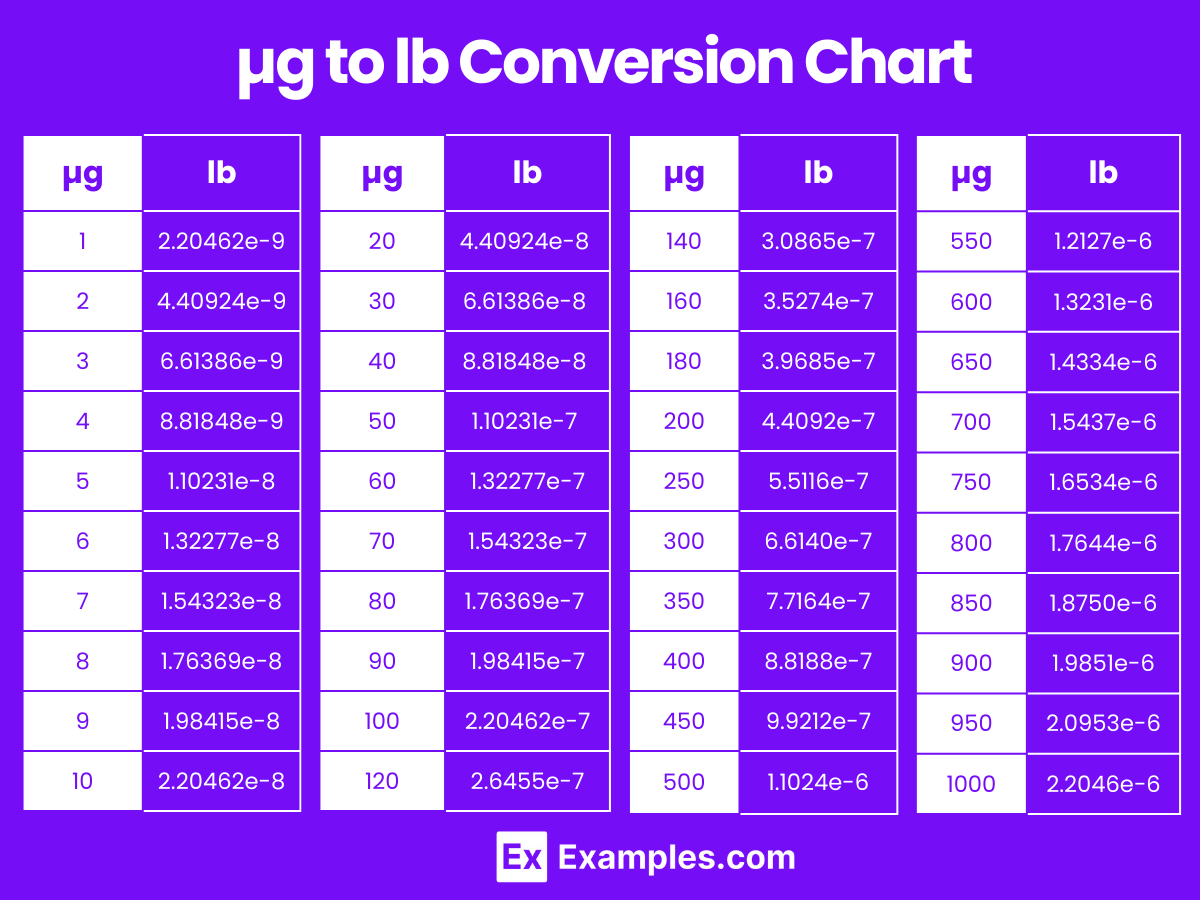
Microgram to Pound Conversion Table
| Micrograms (µg) | Pounds (lb) |
|---|---|
| 1 µg | 2.20462e-9 lb |
| 2 µg | 4.40924e-9 lb |
| 3 µg | 6.61386e-9 lb |
| 4 µg | 8.81848e-9 lb |
| 5 µg | 1.10231e-8 lb |
| 6 µg | 1.32277e-8 lb |
| 7 µg | 1.54323e-8 lb |
| 8 µg | 1.76369e-8 lb |
| 9 µg | 1.98415e-8 lb |
| 10 µg | 2.20462e-8 lb |
| 20 µg | 4.40924e-8 lb |
| 30 µg | 6.61386e-8 lb |
| 40 µg | 8.81848e-8 lb |
| 50 µg | 1.10231e-7 lb |
| 60 µg | 1.32277e-7 lb |
| 70 µg | 1.54323e-7 lb |
| 80 µg | 1.76369e-7 lb |
| 90 µg | 1.98415e-7 lb |
| 100 µg | 2.20462e-7 lb |
µg to lb Conversion Chart
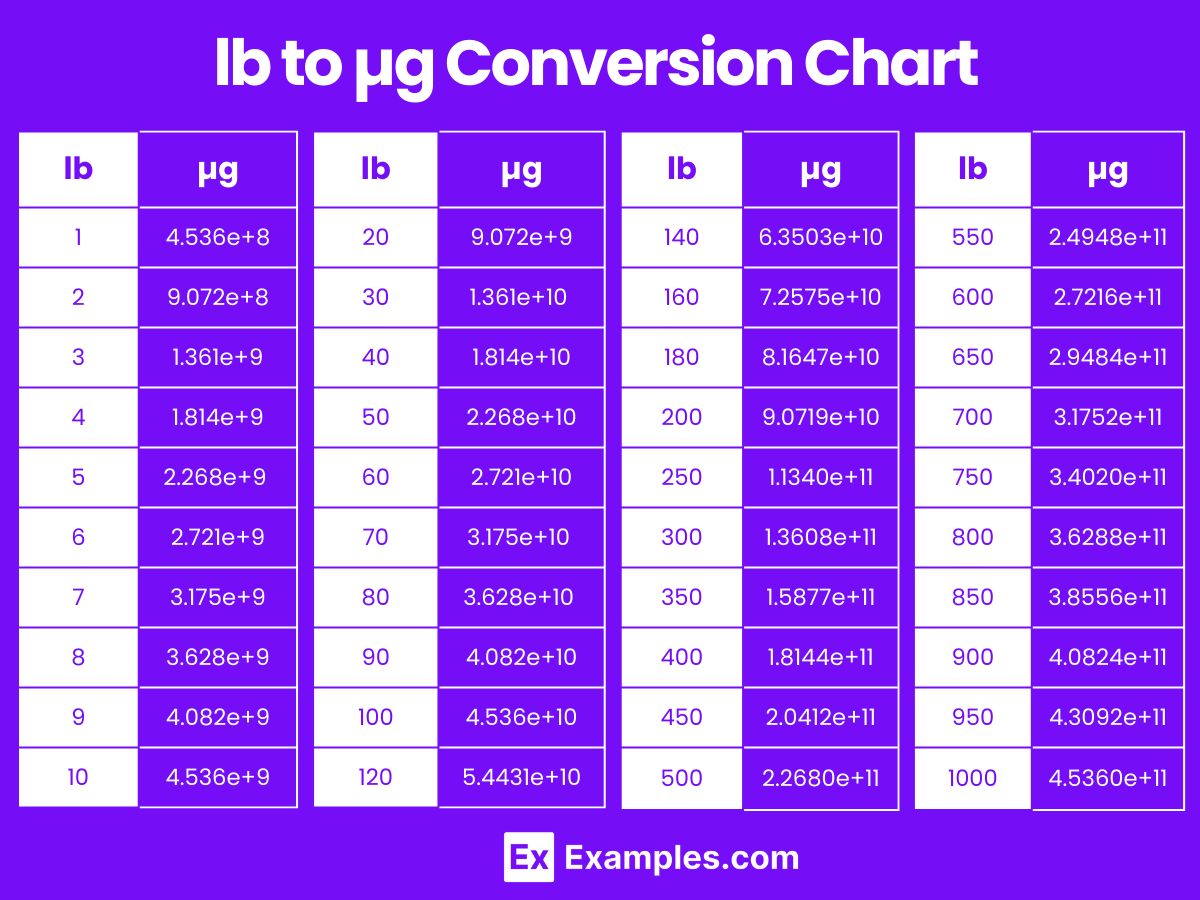
Pound to Microgram Conversion Table
| Pounds (lb) | Micrograms (µg) |
|---|---|
| 1 lb | 4.536e+8 µg |
| 2 lb | 9.072e+8 µg |
| 3 lb | 1.361e+9 µg |
| 4 lb | 1.814e+9 µg |
| 5 lb | 2.268e+9 µg |
| 6 lb | 2.721e+9 µg |
| 7 lb | 3.175e+9 µg |
| 8 lb | 3.628e+9 µg |
| 9 lb | 4.082e+9 µg |
| 10 lb | 4.536e+9 µg |
| 20 lb | 9.072e+9 µg |
| 30 lb | 1.361e+10 µg |
| 40 lb | 1.814e+10 µg |
| 50 lb | 2.268e+10 µg |
| 60 lb | 2.721e+10 µg |
| 70 lb | 3.175e+10 µg |
| 80 lb | 3.628e+10 µg |
| 90 lb | 4.082e+10 µg |
| 100 lb | 4.536e+10 µg |
lb to µg Conversion Chart
Differences Between Micrograms to Pounds
| Aspect | Microgram | Pound |
|---|---|---|
| Definition | A microgram (µg) is a unit of mass. | A pound (lb) is a unit of weight. |
| Size | Extremely small mass measurement. | Much larger mass measurement. |
| Metric System | Part of the metric system. | Part of the imperial system. |
| Conversion | 1 µg = 1 x 10⁻⁶ grams. | 1 lb = 453.59237 grams. |
| Usage | Used for measuring very light objects or substances. | Used for measuring larger weights such as body weight, packages, etc. |
| Common Applications | Pharmaceutical dosages, scientific measurements. | Everyday weight measurements, shipping, and groceries. |
| Abbreviation | µg | lb |
| Conversion to Pounds | 1 µg = 2.20462 x 10⁻⁹ pounds. | 1 lb = 453,592,370 µg. |
1. Solved Examples on Converting Micrograms to Pounds
Example 1
Problem: Convert 500,000 micrograms to pounds.
Solution: Pounds=500,000×2.2046e−9
Pounds=0.0011023
Example 2
Problem: Convert 1,200,000 micrograms to pounds.
Solution: Pounds=1,200,000×2.2046e−9
Pounds=0.002644
Example 3
Problem: Convert 2,500,000 micrograms to pounds.
Solution: Pounds=2,500,000×2.2046e−9
Pounds=0.0055115
Example 4
Problem: Convert 750,000 micrograms to pounds.
Solution: Pounds=750,000×2.2046e−9
Pounds=0.00165345
Example 5
Problem: Convert 3,000,000 micrograms to pounds.
Solution: Pounds=3,000,000×2.2046e−9
Pounds=0.0066138
2. Solved Examples on Converting Pounds to Micrograms
Example 1
Problem: Convert 0.1 pounds to micrograms.
Solution: Micrograms=0.1×4.536e+8
Micrograms=45,360,000
Example 2
Problem: Convert 2 pounds to micrograms.
Solution: Micrograms=2×4.536e+8
Micrograms=907,200,000
Example 3
Problem: Convert 0.5 pounds to micrograms.
Solution: Micrograms=0.5×4.536e+8
Micrograms=226,800,000
Example 4
Problem: Convert 3.25 pounds to micrograms.
Solution: Micrograms=3.25×4.536e+8
Micrograms=1,476,000,000
Example 5
Problem: Convert 7 pounds to micrograms.
Solution: Micrograms=7×4.536e+8
Micrograms=3,175,200,000
Why do I need to convert micrograms to pounds?
Converting micrograms to pounds may be necessary for scientific research, quality control in manufacturing, or when working with products and substances that are measured in different units.
Can I use an online converter for this calculation?
Yes, online converters and calculators can simplify the conversion process. Just input the number of micrograms, and the tool will provide the equivalent weight in pounds.
What are some common uses for converting micrograms to pounds?
Common uses include measuring ingredients in pharmaceuticals, assessing small quantities in chemical experiments, and determining weight in industries where both metric and imperial units are used.
How do I handle very large numbers in these conversions?
For very large numbers, use scientific notation or a calculator to avoid errors. Ensure that you multiply accurately to maintain precision.
Are there any common errors to watch out for in these conversions?
Common errors include incorrect placement of decimal points, misusing conversion factors, and not maintaining precision. Always double-check your calculations.
How do I convert micrograms to pounds for scientific research?
For scientific research, use precise measurement tools and follow standard conversion formulas. Ensure that all units are correctly aligned and that measurements are taken accurately.
How do conversion factors affect the accuracy of my results?
The accuracy of your results depends on using the correct and precise conversion factor. An incorrect factor will lead to inaccurate results, so always verify that you are using the right value.

