Preparing for the NCLEX PN® Exam requires a comprehensive understanding of skills and procedures in fundamentals, essential for effective nursing care. Mastery of techniques such as vital sign monitoring, wound care, catheterization, and medication administration is crucial. This knowledge ensures safe, accurate, and patient-centered care, promoting recovery and maintaining health outcomes.
Learning Objective
In studying “Skills/Procedures in Fundamentals” for the NCLEX PN® Exam, you should aim to understand and apply essential nursing techniques to ensure safe and effective patient care. Learn to perform procedures such as vital sign measurement, wound care, catheterization, and medication administration with precision and confidence. Evaluate the principles of aseptic technique, proper documentation, and patient communication during procedures. Additionally, explore strategies for adapting skills to diverse patient needs and clinical scenarios. Apply this knowledge to deliver high-quality care, minimize risks, and address patient comfort and safety while mastering the fundamental nursing procedures critical for professional practice.
Overview of Nursing Skills and Procedures
Nursing skills and procedures are foundational for delivering safe, effective, and high-quality patient care. These skills encompass a wide range of technical, interpersonal, and critical thinking abilities that allow nurses to address patients’ physical, emotional, and psychological needs. Below is an overview of key nursing skills and procedures:
1. Basic Nursing Skills
- Vital Signs Monitoring: Measure temperature, pulse, respiration, blood pressure, and oxygen saturation.
- Hygiene: Assist with bathing, grooming, and oral care to maintain comfort and prevent infections.
- Mobility: Help patients move and reposition to prevent complications.
2. Medication Administration
- Five Rights: Right patient, medication, dose, route, time.
- Routes: Oral, IV, IM, SC, or topical.
- Monitoring: Observe for side effects and adverse reactions.
3. Wound Care
- Dressing Changes: Use sterile techniques to clean and dress wounds.
- Skin Assessment: Prevent pressure ulcers through repositioning and skin care.
4. Infection Control
- Hand Hygiene: Follow protocols for washing hands or using sanitizers.
- PPE: Wear gloves, masks, and gowns when necessary.
5. Respiratory and IV Therapy
- Oxygen Therapy: Administer via nasal cannula or masks.
- IV Management: Insert and monitor IVs, ensuring proper fluid and medication administration.
6. Patient Education
- Provide health teaching on medications, lifestyle, and disease management.
- Educate on post-procedure care and follow-up needs.
Measurement of Vital Signs
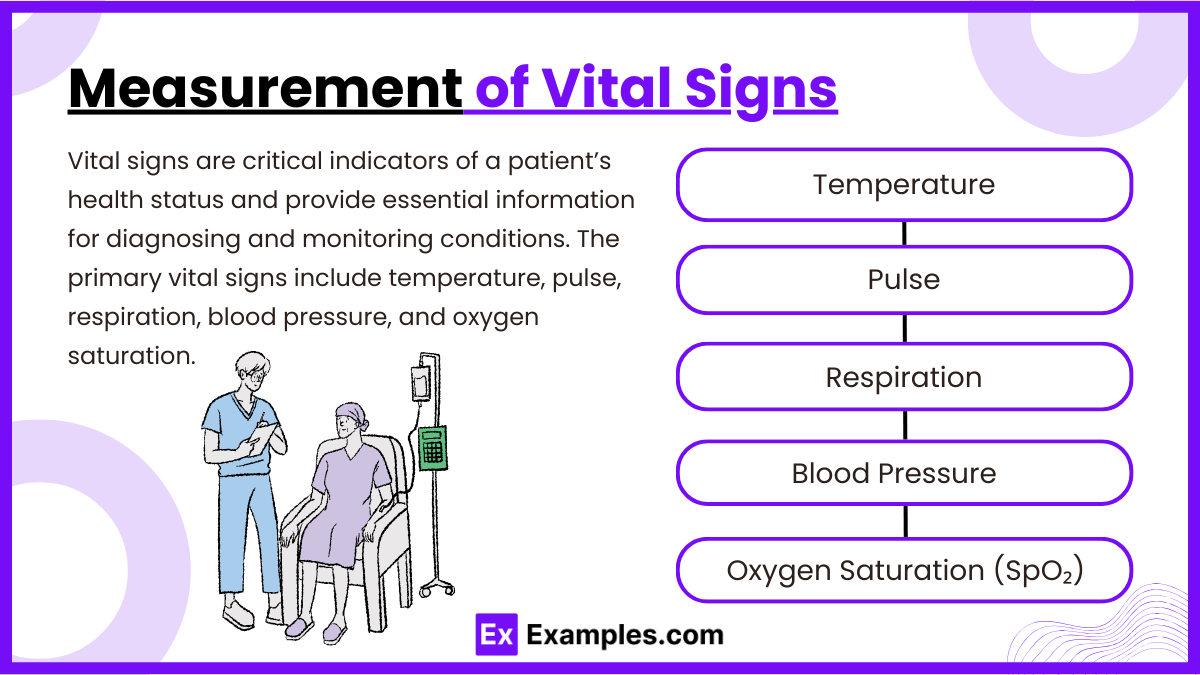
Vital signs are critical indicators of a patient’s health status and provide essential information for diagnosing and monitoring conditions. The primary vital signs include temperature, pulse, respiration, blood pressure, and oxygen saturation.
1. Temperature
- Normal Range: 36.5°C–37.5°C (97.7°F–99.5°F).
- Methods: Oral, rectal (most accurate), axillary, tympanic, and temporal.
- Considerations: Avoid hot/cold drinks before oral measurement.
2. Pulse
- Normal Range: 60-100 bpm.
- Sites: Radial (wrist), carotid (neck), apical (heart).
- Assessment: Check rate, rhythm, and strength.
3. Respiration
- Normal Range: 12-20 breaths per minute.
- Assessment: Observe chest rise and fall, note rhythm and effort.
4. Blood Pressure
- Normal Range: <120/80 mmHg.
- Methods: Manual (sphygmomanometer) or automatic.
- Considerations: Use proper cuff size, ensure arm is at heart level.
5. Oxygen Saturation (SpO₂)
- Normal Range: 95%-100%.
- Measurement: Pulse oximeter on fingertip or earlobe.
- Considerations: Remove nail polish for accurate readings.
Medication Administration
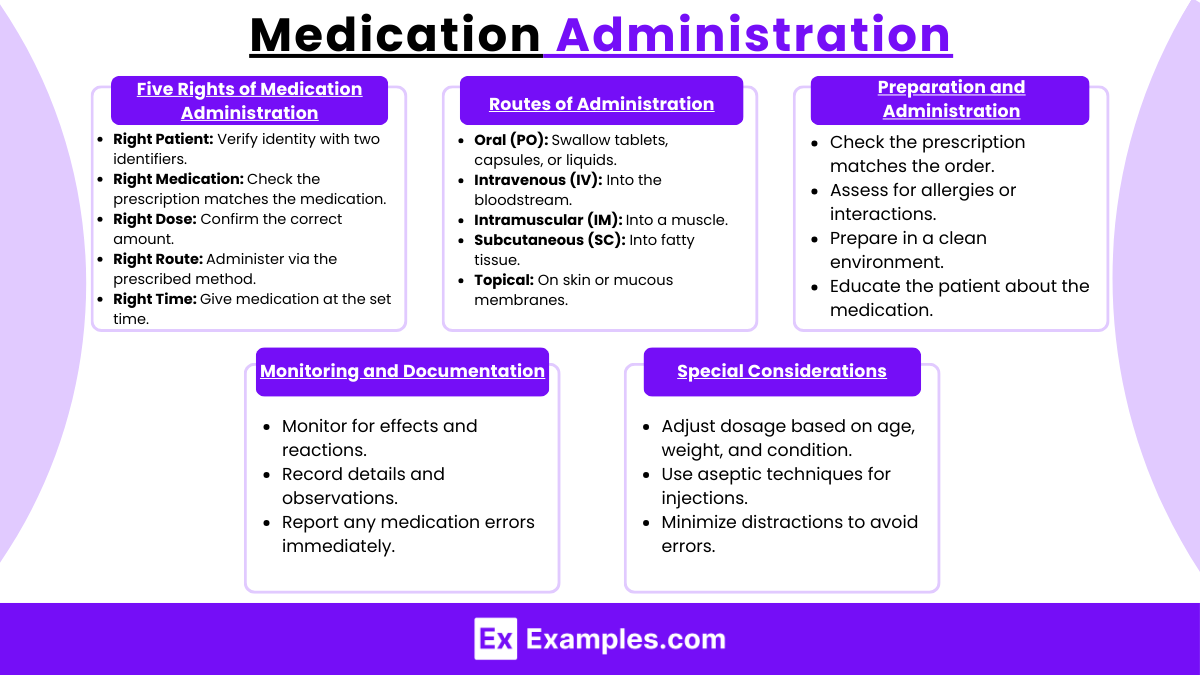
1. The Five Rights of Medication Administration
- Right Patient: Verify patient identity using two identifiers (e.g., name and date of birth).
- Right Medication: Match the prescribed medication to the order.
- Right Dose: Confirm the correct amount to be administered.
- Right Route: Ensure the medication is given via the correct method (e.g., oral, IV).
- Right Time: Administer at the prescribed time, considering intervals and frequency.
2. Routes of Administration
- Oral (PO): Tablets, capsules, or liquids swallowed.
- Intravenous (IV): Delivered directly into the bloodstream.
- Intramuscular (IM): Injected into a muscle.
- Subcutaneous (SC): Injected into the fatty tissue beneath the skin.
- Topical: Applied directly to the skin or mucous membranes.
3. Preparation and Administration
- Check the prescription against the medication order.
- Assess for contraindications (e.g., allergies, interactions).
- Prepare medication in a clean environment.
- Educate the patient on the purpose and potential side effects.
4. Monitoring and Documentation
- Observe for therapeutic effects or adverse reactions.
- Record medication name, dose, route, time, and any observations.
- Report and document any medication errors promptly.
5. Special Considerations
- Adjust for patient age, weight, and health conditions.
- Use aseptic techniques for injections and IV administration.
- Avoid distractions to reduce the risk of errors.
Examples
Example 1: Measuring Blood Pressure Manually
- A nurse uses a sphygmomanometer and stethoscope to measure a patient’s blood pressure. The nurse ensures the cuff is the correct size, places it on the upper arm, inflates it to the appropriate pressure, and listens for Korotkoff sounds to determine systolic and diastolic values. Results are documented accurately.
Example 2: Performing Wound Care
- A nurse changes the dressing for a surgical incision. After donning sterile gloves, the nurse removes the old dressing, cleans the wound using a sterile solution, and applies a fresh, sterile dressing. The nurse assesses the wound for signs of infection, such as redness, swelling, or discharge.
Example 3: Administering a Subcutaneous Injection
- A nurse administers insulin to a diabetic patient. The nurse verifies the correct dose, selects an appropriate injection site (e.g., abdomen or thigh), cleanses the area with an alcohol swab, and injects the medication at a 45- or 90-degree angle, ensuring proper technique to minimize discomfort.
Example 4: Inserting an Indwelling Catheter
- A nurse inserts a urinary catheter for a patient experiencing acute urinary retention. Using sterile technique, the nurse prepares the equipment, lubricates the catheter, inserts it into the urethra, and secures it in place after urine flow is established. The nurse monitors and records urine output.
Example 5: Providing Oxygen Therapy
- A patient with low oxygen saturation is placed on oxygen therapy. The nurse selects a nasal cannula, sets the flow rate per the provider’s order, and monitors the patient’s oxygen levels using a pulse oximeter. The nurse educates the patient on using the equipment safely and checks for skin irritation around the cannula.
Practice Questions
Question 1
What is the most appropriate step to ensure accurate blood pressure measurement?
A. Use a cuff that is the correct size for the patient’s arm.
B. Inflate the cuff to 100 mmHg regardless of the patient’s baseline.
C. Position the patient’s arm below heart level.
D. Measure blood pressure while the patient is actively talking.
Answer:
A. Use a cuff that is the correct size for the patient’s arm.
Explanation:
Using a properly sized cuff is essential for accurate blood pressure measurement. A cuff that is too small or too large can give false readings. Inflating the cuff to 100 mmHg (option B) may not be adequate for all patients. Positioning the arm below heart level (option C) or measuring while the patient is talking (option D) can also result in inaccurate readings.
Question 2
What is the correct angle for administering a subcutaneous injection?
A. 15 degrees
B. 30 degrees
C. 45 degrees or 90 degrees
D. 90 degrees only
Answer:
C. 45 degrees or 90 degrees
Explanation:
Subcutaneous injections are typically administered at a 45-degree or 90-degree angle, depending on the patient’s body type and the thickness of subcutaneous tissue. A 90-degree angle is often used for patients with more adipose tissue, while a 45-degree angle is used for those with less. A 15-degree angle (option A) is used for intradermal injections, and 30 degrees (option B) is not appropriate for subcutaneous administration.
Question 3
What should the nurse do first before inserting an indwelling urinary catheter?
A. Clean the patient’s perineal area with soap and water.
B. Inflate the catheter balloon to check for leaks.
C. Position the patient in a side-lying position.
D. Obtain the patient’s vital signs.
Answer:
A. Clean the patient’s perineal area with soap and water.
Explanation:
Cleaning the patient’s perineal area is the first step before inserting a urinary catheter to reduce the risk of introducing infection. Inflating the catheter balloon (option B) is done later to ensure proper placement, and positioning the patient in a side-lying position (option C) is not the standard approach for catheter insertion. While obtaining vital signs (option D) is important, it is not the priority step immediately before catheter insertion.