The urinary/renal system plays a crucial role in filtering waste, maintaining fluid and electrolyte balance, and regulating blood pressure. It includes the kidneys, ureters, bladder, and urethra, all of which work together to eliminate toxins from the body. For NCLEX-PN® candidates, understanding renal anatomy, physiology, and common disorders like UTIs, kidney stones, and renal failure is essential. Mastery of nursing interventions, lab value interpretation, and patient care strategies related to the urinary system is critical for achieving a high score on the exam.
Learning Objectives
In studying “Adult Health: Urinary/Renal” for the NCLEX-PN® Exam, you should learn to understand the anatomy and physiology of the urinary system, including the kidneys, ureters, bladder, and urethra. Analyze common renal conditions such as acute kidney injury (AKI), chronic kidney disease (CKD), urinary tract infections (UTIs), renal calculi (kidney stones), and incontinence, focusing on pathophysiology, clinical manifestations, and treatment options. Evaluate nursing considerations such as fluid balance, electrolyte management, catheter care, and infection prevention. Explore pharmacological interventions, including diuretics, antibiotics, and erythropoietin therapy. Apply knowledge to prioritize care, monitor fluid status, and respond effectively to urinary/renal-related patient scenarios.
1. Anatomy and Physiology of the Urinary/Renal System
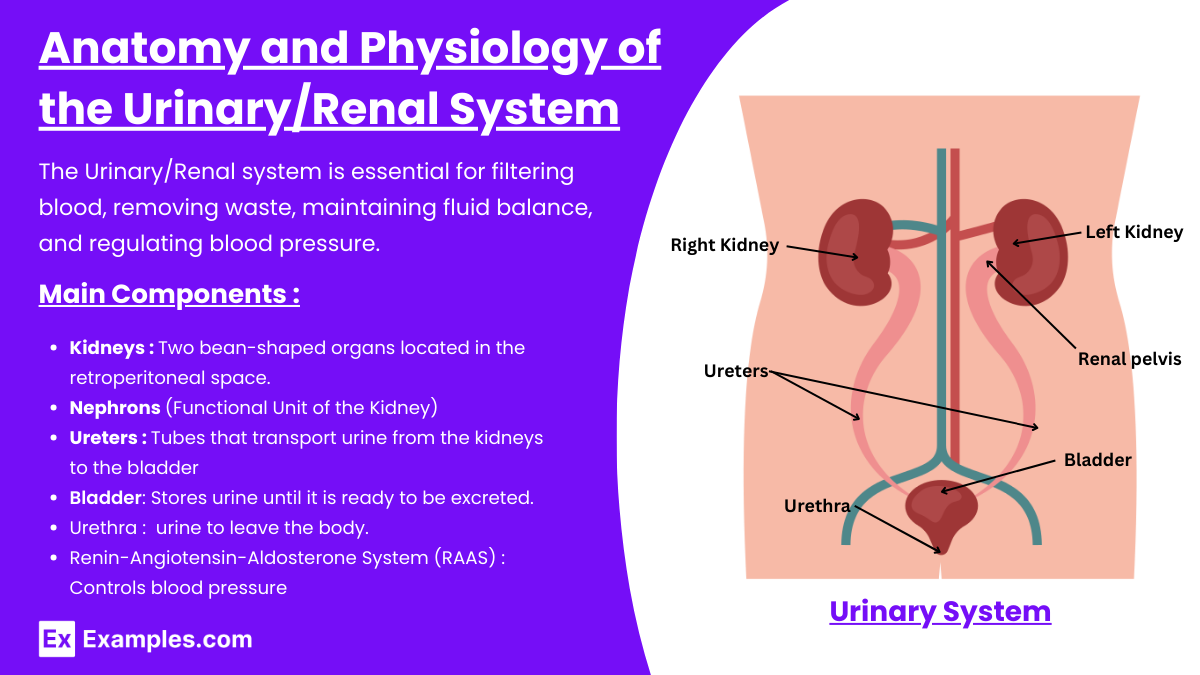
The Urinary/Renal system is essential for filtering blood, removing waste, maintaining fluid balance, and regulating blood pressure. A strong grasp of this system is vital for success in the NCLEX-PN® exam, especially for patient care and nursing interventions.
Main Components
- Kidneys:
- Location: Two bean-shaped organs located in the retroperitoneal space.
- Function:
- Filtration: Remove waste products and toxins from the blood.
- Reabsorption: Water, electrolytes, and glucose are reabsorbed into the bloodstream.
- Secretion: Removes excess ions, drugs, and metabolic byproducts.
- Hormonal Role: Produces erythropoietin for RBC production and activates Vitamin D.
- Nephrons (Functional Unit of the Kidney):
- Glomerulus: Filters blood to produce filtrate (pre-urine).
- Bowman’s Capsule: Collects the filtrate.
- Renal Tubules: Includes proximal tubule, loop of Henle, distal tubule, and collecting duct for reabsorption and secretion.
- Ureters:
- Tubes that transport urine from the kidneys to the bladder using peristaltic movement.
- Bladder:
- Stores urine until it is ready to be excreted. The bladder has stretch receptors that signal the need to urinate.
- Urethra:
- The final passageway for urine to leave the body.
- Renin-Angiotensin-Aldosterone System (RAAS):
- Controls blood pressure by adjusting fluid retention and vasoconstriction.
2. Common Disorders of the Urinary/Renal System
This section covers renal diseases and conditions most likely to appear on the NCLEX-PN® exam. Nurses must understand the symptoms, causes, diagnostics, and nursing interventions for each disorder.
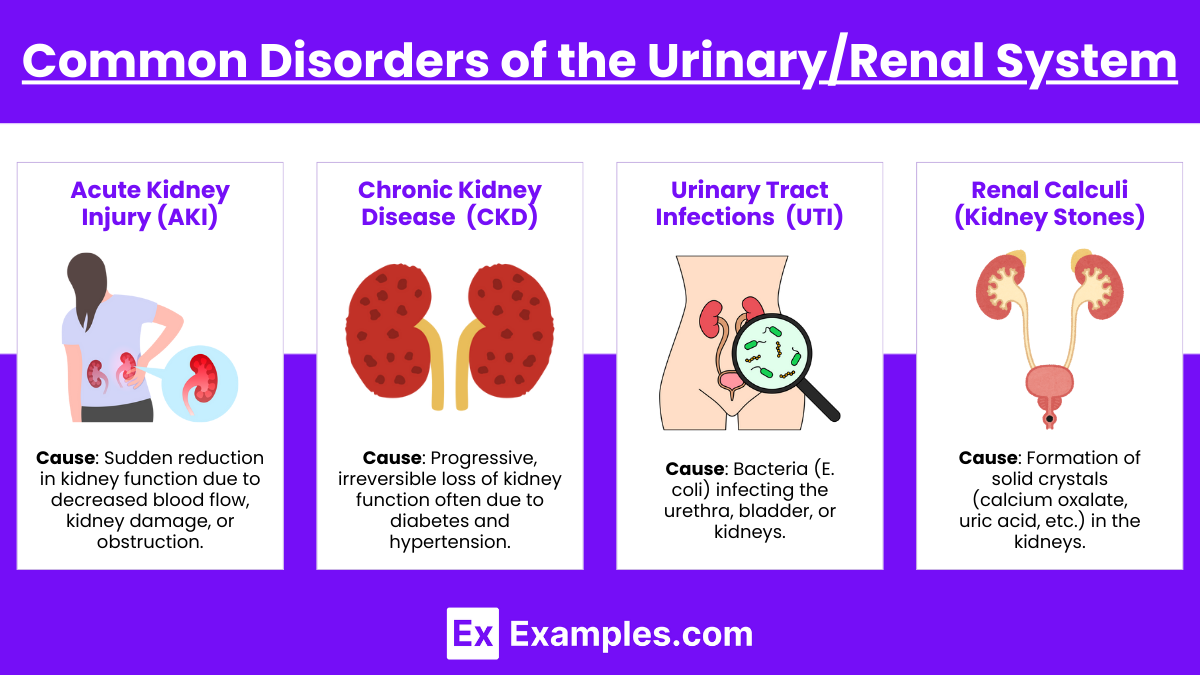
1. Acute Kidney Injury (AKI)
- Cause: Sudden reduction in kidney function due to decreased blood flow, kidney damage, or obstruction.
- Types:
- Prerenal: Caused by reduced perfusion (shock, dehydration).
- Intrarenal: Caused by direct damage to the kidneys (nephrotoxic drugs, infections).
- Postrenal: Caused by obstructions (renal calculi, tumors, enlarged prostate).
- Signs/Symptoms:
- Oliguria (urine output < 400 mL/day)
- Edema
- Elevated BUN and creatinine
- Hyperkalemia (life-threatening)
- Nursing Interventions:
- Monitor I&O and daily weight.
- Manage electrolyte imbalance (reduce potassium).
- Fluid restriction and administer diuretics.
2. Chronic Kidney Disease (CKD)
- Cause: Progressive, irreversible loss of kidney function often due to diabetes and hypertension.
- Stages:
- Stage 1: GFR > 90 mL/min (Normal but with kidney damage)
- Stage 2-4: Progressive decrease in GFR
- Stage 5: End-stage renal disease (ESRD) requiring dialysis or transplant
- Signs/Symptoms:
- Uremia (build-up of toxins in the blood)
- Fatigue, pruritus, confusion
- Fluid overload (edema, dyspnea)
- Nursing Interventions:
- Encourage low-protein, low-sodium, and low-phosphorus diets.
- Fluid restrictions and blood pressure control.
- Prepare patients for dialysis and kidney transplant education.
3. Urinary Tract Infections (UTI)
- Cause: Bacteria (E. coli) infecting the urethra, bladder, or kidneys.
- Types:
- Lower UTI: Affects the bladder (cystitis) and urethra.
- Upper UTI: Affects the kidneys (pyelonephritis).
- Signs/Symptoms:
- Dysuria (painful urination)
- Urgency and frequency
- Suprapubic pain
- Cloudy, foul-smelling urine
- Nursing Interventions:
- Administer antibiotics.
- Encourage fluids (2-3L/day) unless contraindicated.
- Teach proper hygiene (wipe front-to-back).
4. Renal Calculi (Kidney Stones)
- Cause: Formation of solid crystals (calcium oxalate, uric acid, etc.) in the kidneys.
- Risk Factors: Dehydration, high protein/salt diet, and genetic predisposition.
- Signs/Symptoms:
- Severe flank pain (radiating to groin)
- Hematuria (blood in urine)
- Nausea and vomiting
- Nursing Interventions:
- Administer pain medications (morphine, NSAIDs).
- Strain all urine to detect stones.
- Encourage hydration (2-3L/day).
3. Key Nursing Interventions and NCLEX Strategies
This section focuses on the nursing interventions and test-taking strategies for the urinary/renal system.
Nursing Interventions
- Fluid Balance: Monitor intake and output, daily weights, and fluid restrictions.
- Electrolyte Management: Monitor potassium, sodium, and calcium levels.
- Infection Prevention: Teach hygiene practices to prevent UTIs and ensure proper catheter care.
- Dialysis Care:
- Assess for complications (hypotension, bleeding, infection).
- Check for AV fistula (feel for thrill, listen for bruit).
- Medications:
- Diuretics (furosemide) to remove excess fluid.
- Phosphate binders (sevelamer) for CKD patients.
- Erythropoietin for anemia in CKD patients.
NCLEX Test-Taking Strategies
- Apply the ABCs (Airway, Breathing, Circulation)
- Prioritize life-threatening issues first.
- Example: For hyperkalemia, immediate action is to prevent cardiac issues.
- Master Lab Values
- BUN: 10-20 mg/dL (elevated in renal failure)
- Creatinine: 0.6-1.2 mg/dL (increased in kidney failure)
- GFR: > 90 mL/min (GFR < 15 requires dialysis)
- Prioritization and Delegation
- Do not delegate assessment tasks to UAPs.
- Assign UAPs for hygiene, vital signs, and intake/output monitoring.
- Focus on Patient Safety
- Prevent falls in patients with incontinence.
- Check for AV fistula function (thrill and bruit) in dialysis patients.
- Critical Thinking Skills
- Analyze labs, prioritize tasks, and respond to emergencies like hyperkalemia.
Examples
Example 1: Acute Kidney Injury (AKI)
This is a sudden loss of kidney function caused by conditions such as dehydration, sepsis, nephrotoxic drugs, or urinary obstruction. It is categorized into prerenal, intrarenal, and postrenal types, each requiring specific nursing interventions like fluid management, electrolyte correction, and continuous monitoring of intake and output (I&O).
Example 2: Chronic Kidney Disease (CKD)
CKD is a progressive, irreversible loss of kidney function that occurs over months or years. It is commonly caused by hypertension or diabetes. Patients with CKD often require dietary modifications (low protein, sodium, and potassium) and may need dialysis or kidney transplantation as part of their long-term treatment.
Example 3: Urinary Tract Infection (UTI)
A UTI is a bacterial infection affecting the urinary tract (bladder, urethra, or kidneys). Symptoms include burning urination (dysuria), frequent urination, urgency, and cloudy or foul-smelling urine. Nursing care includes encouraging hydration, administering antibiotics, and educating the patient on proper hygiene practices to prevent recurrence.
Example 4: Renal Calculi (Kidney Stones)
Kidney stones are solid crystal deposits that form in the urinary tract, causing severe flank pain, hematuria (blood in urine), and difficulty urinating. Nursing care focuses on pain management, encouraging hydration to help pass the stones, and straining urine to catch the stones for laboratory analysis. Diet modifications may be needed to prevent stone recurrence.
Example 5: Urinary Incontinence
This condition occurs when a person loses control of their bladder, leading to involuntary urine leakage. It can be classified into stress incontinence, urge incontinence, overflow incontinence, and functional incontinence. Nursing interventions include bladder training, pelvic floor exercises (Kegels), and providing support devices like absorbent pads or catheters when necessary.
Practice Questions
Question 1
A patient with chronic kidney disease (CKD) is admitted with complaints of shortness of breath, swelling in the ankles, and weight gain of 2 kg in 24 hours. Which nursing intervention should the practical nurse (PN) prioritize?
A) Encourage the patient to increase fluid intake
B) Administer a potassium supplement as prescribed
C) Monitor daily weights and restrict fluid intake
D) Apply warm compresses to the patient’s legs to reduce swelling
Answer: C) Monitor daily weights and restrict fluid intake
Explanation:
- Why “C” is correct: Patients with CKD often experience fluid overload due to the kidneys’ inability to excrete fluid properly. Fluid restrictions and daily weight monitoring are critical nursing interventions. A rapid weight gain (like 2 kg in 24 hours) indicates fluid retention, and the nurse must track daily weights as a key indicator of fluid balance.
- Why other options are incorrect:
- Option A: Increasing fluid intake would worsen the patient’s condition by causing further fluid overload.
- Option B: Potassium is not administered unless there is documented hypokalemia. CKD patients are often at risk of hyperkalemia due to the inability to excrete potassium properly.
- Option D: Warm compresses will not address fluid retention. The correct intervention is to reduce the overall fluid volume, not just treat local swelling.
Question 2
A nurse is caring for a patient with a urinary tract infection (UTI) who reports burning during urination, frequency, and urgency. Which of the following nursing actions should be prioritized?
A) Encourage the patient to drink 2-3 liters of fluid daily
B) Restrict fluid intake to reduce urinary frequency
C) Advise the patient to reduce caffeine and spicy foods
D) Apply a heating pad to the abdomen to relieve discomfort
Answer: A) Encourage the patient to drink 2-3 liters of fluid daily
Explanation:
- Why “A” is correct: Adequate hydration helps flush bacteria from the urinary tract. Increasing fluid intake to 2-3 liters per day is one of the primary interventions for UTI treatment. It reduces the concentration of bacteria in the urine and promotes frequent urination, which helps flush out the infection.
- Why other options are incorrect:
- Option B: Restricting fluid intake would worsen the infection by allowing bacteria to accumulate. Increasing urine flow is essential for clearing the infection.
- Option C: While reducing caffeine and spicy foods may help avoid bladder irritation, it is not the priority action. Hydration takes precedence over dietary changes.
- Option D: Using a heating pad may provide comfort but does not address the root cause of the infection (bacterial growth).
Question 3
A patient with end-stage renal disease (ESRD) is undergoing hemodialysis. The nurse notices the arteriovenous (AV) fistula site is red, warm, and has purulent drainage. Which action should the nurse take first?
A) Document the findings as normal post-dialysis symptoms
B) Apply a warm compress to reduce inflammation
C) Notify the healthcare provider immediately
D) Assess for the presence of a bruit and thrill
Answer: C) Notify the healthcare provider immediately
Explanation:
- Why “C” is correct: Redness, warmth, and purulent drainage at an AV fistula site are signs of infection. Infection at the AV site poses a significant risk for sepsis, especially in dialysis patients. Immediate notification of the healthcare provider is essential to initiate antibiotic therapy.
- Why other options are incorrect:
- Option A: These signs are not normal for a fistula. Redness, warmth, and purulent drainage indicate infection, which requires prompt attention.
- Option B: Applying a warm compress may provide temporary relief but will not address the underlying infection. Early antibiotic treatment is necessary.
- Option D: While checking for a bruit and thrill is important, this action does not take precedence over the potential for infection. Reporting infection signs takes priority.