Preparing for the NCLEX PN® Exam requires a thorough understanding of the visual and auditory systems in adult health, essential components of comprehensive nursing care. Mastery of eye and ear anatomy, common disorders, and their management is crucial. This knowledge aids in promoting optimal sensory function and quality of life for patients.
Learning Objective
In studying “Visual/Auditory in Adult Health” for the NCLEX PN® Exam, you should aim to understand the anatomy and physiology of the eye and ear, including the mechanisms of vision and hearing. Learn to identify and manage common visual and auditory disorders such as cataracts, glaucoma, macular degeneration, hearing loss, and infections. Evaluate diagnostic techniques like ophthalmoscopy, tonometry, audiometry, and tympanometry. Additionally, explore the impact of aging on sensory functions and apply this knowledge to nursing interventions that enhance sensory health, assist in adaptation to sensory changes, and improve communication for patients experiencing visual and auditory impairments.
Anatomy and Physiology of the Visual/Auditory
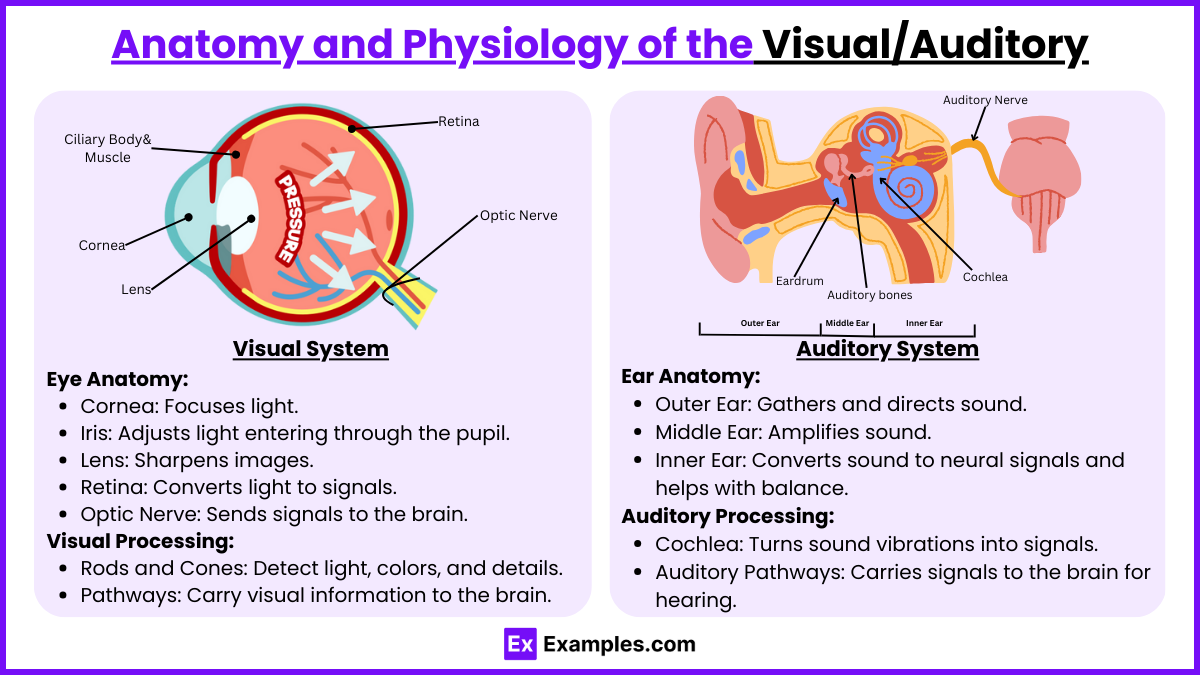
The anatomy and physiology of the visual and auditory systems are complex, involving multiple structures that work together to process sensory information from our environment. Here is a detailed overview of each system:
Visual System
- Eye Anatomy:
- Cornea: The clear, dome-shaped surface that covers the front of the eye and helps focus incoming light.
- Iris: The colored part of the eye that controls the size of the pupil.
- Pupil: The opening in the iris through which light enters the eye.
- Lens: Focuses light onto the retina, changing shape to adjust focus (accommodation).
- Retina: The layer of light-sensitive cells at the back of the eye that converts light into electrical signals.
- Optic Nerve: Transmits visual information from the retina to the brain.
- Visual Processing:
- Photoreceptors (rods and cones): Rods detect light and dark changes, shapes, and movements; cones detect colors and finer details.
- Visual Pathways: Signals from the retina are processed by the brain via the optic nerve, optic chiasm, optic tracts, and finally to the visual cortex in the occipital lobe.
Auditory System
- Ear Anatomy:
- Outer Ear: Includes the pinna (earlobe) and the ear canal, which collect and channel sound waves toward the eardrum.
- Middle Ear: Contains the ossicles (malleus, incus, stapes), small bones that amplify sound vibrations from the eardrum to the inner ear.
- Inner Ear: Consists of the cochlea (converts sound vibrations into neural signals) and the vestibular system (involved in balance).
- Auditory Processing:
- Cochlea: Sound vibrations cause the fluid inside the cochlea to move, stimulating hair cells that convert these movements into electrical signals.
- Auditory Pathways: Signals are sent from the cochlea through the auditory nerve to various brainstem nuclei, then to the thalamus, and finally to the auditory cortex in the temporal lobe.
Common Visual Disorders
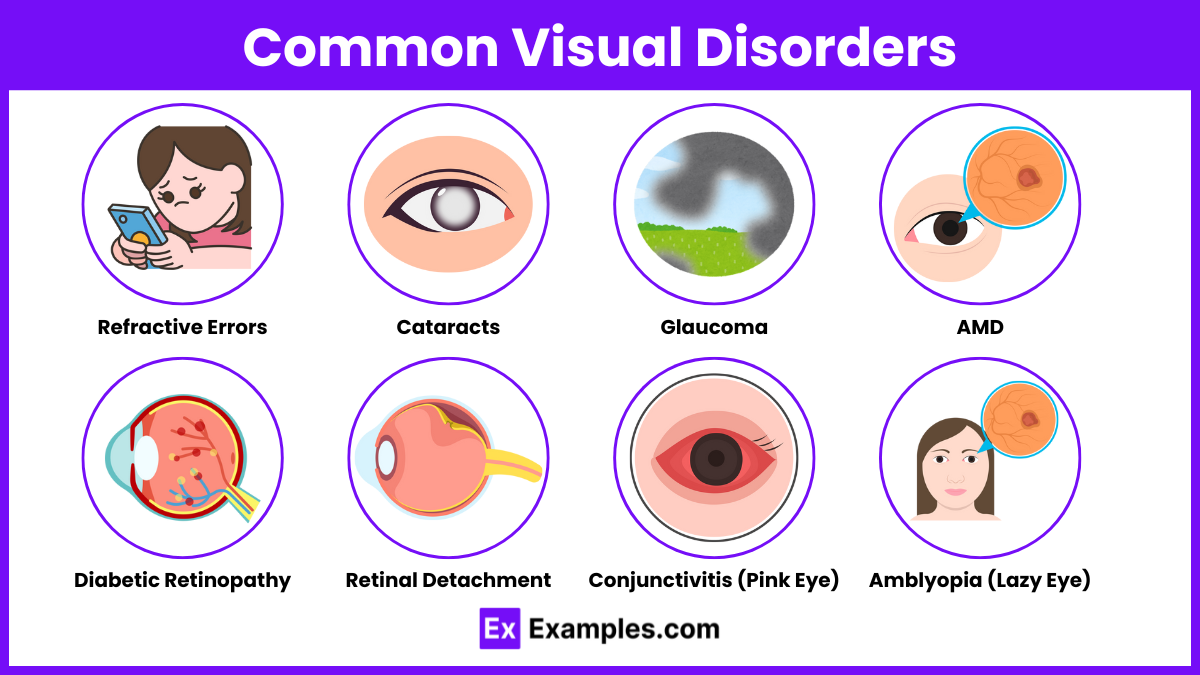
Visual disorders can affect any part of the visual system, from the eyes to the visual cortex in the brain. These disorders can range from common refractive errors to more complex conditions affecting vision. Here is an overview of some of the most common visual disorders:
1. Refractive Errors
- Myopia (Nearsightedness): Difficulty seeing distant objects clearly. It occurs when the eye is too long relative to the focusing power of the cornea and lens, causing light rays to focus in front of the retina.
- Hyperopia (Farsightedness): Difficulty seeing close objects clearly. It occurs when the eye is too short, causing light rays to focus behind the retina.
- Astigmatism: Blurred vision at any distance due to an irregular curvature of the cornea or lens, which prevents light from focusing properly on the retina.
- Presbyopia: Age-related loss of the eye’s ability to focus on nearby objects due to the hardening of the lens.
2. Cataracts
- A condition where the lens of the eye becomes progressively opaque, resulting in blurred vision. It is often related to aging but can also result from trauma, radiation exposure, or be congenital.
3. Glaucoma
- A group of eye conditions that damage the optic nerve, often associated with abnormally high pressure in the eye. Glaucoma is one of the leading causes of blindness for people over the age of 60.
4. Age-related Macular Degeneration (AMD)
- A disease that causes deterioration of the macula, the central portion of the retina, leading to loss of central vision. AMD is a leading cause of vision loss in older adults.
5. Diabetic Retinopathy
- A complication of diabetes that affects the eyes. It is caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). It can lead to blindness if not properly managed.
6. Retinal Detachment
- An emergency condition in which the retina at the back of the eye pulls away from its normal position. If not promptly treated, this condition can cause permanent vision loss.
7. Conjunctivitis (Pink Eye)
- Inflammation or infection of the outer membrane of the eyeball and the inner eyelid. It can be caused by allergies, bacteria, viruses, or irritants.
8. Amblyopia (Lazy Eye)
- A vision development disorder where an eye fails to achieve normal visual acuity, even with prescription eyeglasses or contact lenses. Amblyopia typically begins during infancy or childhood.
Common Auditory Disorders
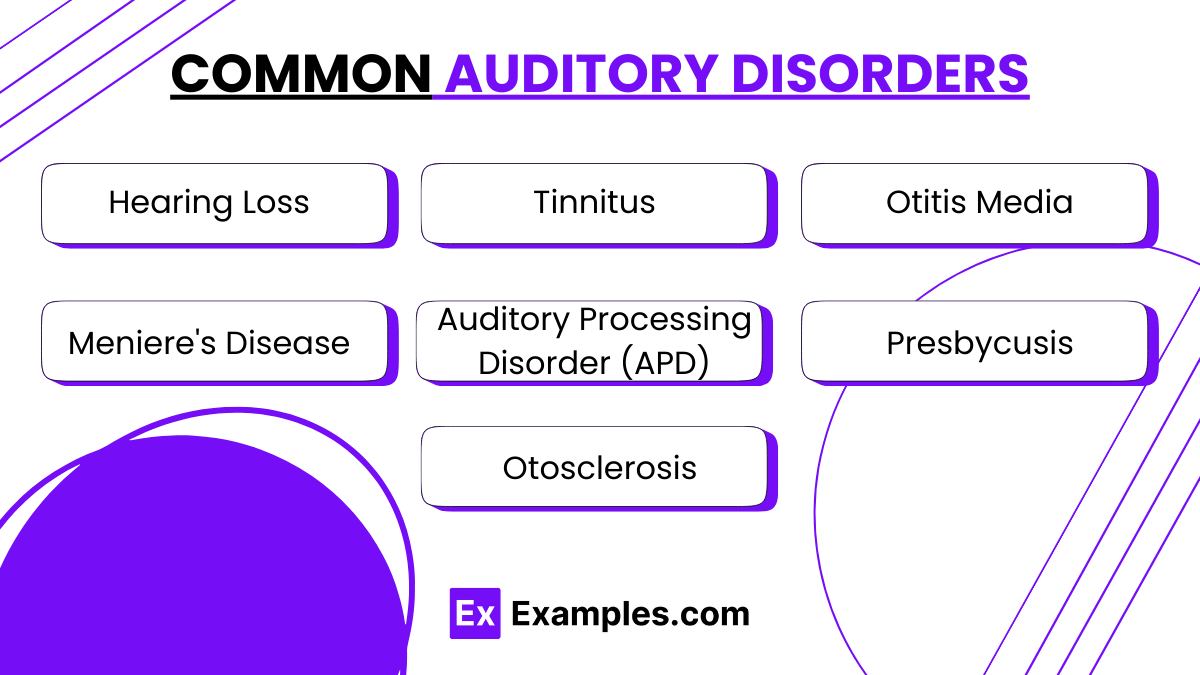
Auditory disorders affect the hearing ability and can range from mild hearing loss to total deafness, along with other complications related to the processing of auditory information. Here’s an overview of some common auditory disorders:
1. Hearing Loss
- Conductive Hearing Loss: Occurs when there is a problem conducting sound waves anywhere along the route through the outer ear, tympanic membrane (eardrum), or middle ear. Common causes include ear infections, fluid in the middle ear, earwax buildup, and abnormalities of the eardrum or ossicles.
- Sensorineural Hearing Loss (SNHL): Occurs due to damage to the inner ear (cochlea) or to the nerve pathways from the inner ear to the brain. Common causes are aging, noise exposure, genetic factors, and diseases.
- Mixed Hearing Loss: Involves both conductive and sensorineural hearing loss.
2. Tinnitus
- Characterized by hearing ringing, buzzing, or other sounds in the ears when no external sound is present. Tinnitus can result from a variety of underlying causes, including age-related hearing loss, exposure to loud noises, earwax accumulation, and medications that damage the inner ear.
3. Otitis Media
- An infection of the middle ear, which is particularly common in children. This can cause pain, fever, and reduced hearing. Chronic otitis media can lead to complications including persistent fluid, recurring ear infections, and damage to the middle ear structures.
4. Meniere’s Disease
- A disorder of the inner ear that can lead to dizzy spells (vertigo) and hearing loss. In most cases, Meniere’s disease affects only one ear and can cause a progressive loss of hearing, as well as a feeling of fullness or pressure in the ear.
5. Auditory Processing Disorder (APD)
- Occurs when the brain has difficulty processing auditory information. This condition does not necessarily involve hearing loss but affects the ability to understand speech, especially in noisy environments, follow oral instructions, or distinguish sounds.
6. Presbycusis
- Age-related hearing loss that gradually occurs as individuals get older. This type of hearing loss is generally bilateral (affecting both ears) and involves the loss of high-frequency sounds initially.
7. Otosclerosis
- Involves abnormal bone growth in the middle ear, which can lead to conductive hearing loss. This condition often starts in early adulthood and may slowly worsen over time.
Diagnostic Techniques
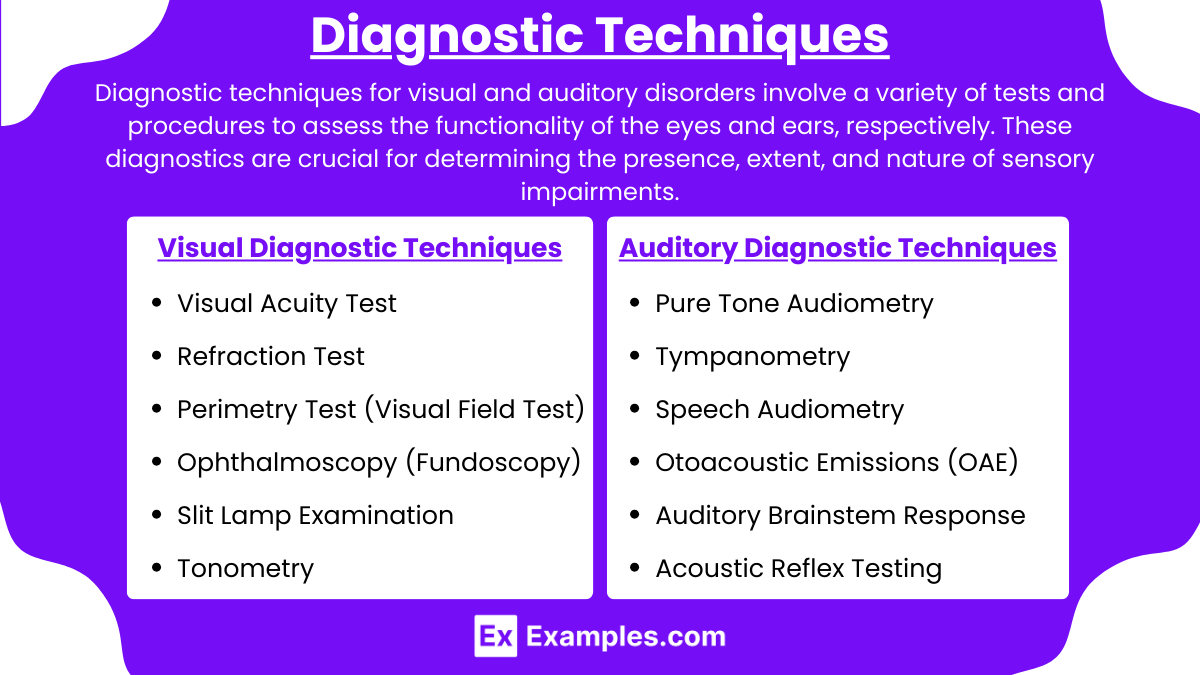
Diagnostic techniques for visual and auditory disorders involve a variety of tests and procedures to assess the functionality of the eyes and ears, respectively. These diagnostics are crucial for determining the presence, extent, and nature of sensory impairments. Here’s an overview of the key diagnostic techniques used in ophthalmology and audiology:
Visual Diagnostic Techniques
- Visual Acuity Test:
- Measures the clarity or sharpness of vision, typically using a Snellen chart.
- Refraction Test:
- Determines the lens power needed to compensate for any refractive error (like myopia or hyperopia).
- Perimetry Test (Visual Field Test):
- Assesses the visual field to identify any central or peripheral vision deficits.
- Ophthalmoscopy (Fundoscopy):
- Examines the back of the eye (retina, optic nerve, blood vessels) using an ophthalmoscope.
- Slit Lamp Examination:
- Provides a magnified, three-dimensional view of the different parts of the eye to detect any abnormalities.
- Tonometry:
- Measures intraocular pressure, which is important for glaucoma detection.
Auditory Diagnostic Techniques
- Pure Tone Audiometry:
- Measures a person’s ability to hear sounds at different pitches and volumes. The patient listens to sounds through headphones and indicates when they hear a sound.
- Tympanometry:
- Assesses the function of the middle ear by varying air pressure in the ear canal, which helps detect fluid in the middle ear, otosclerosis, or eardrum perforations.
- Speech Audiometry:
- Evaluates the ability to understand speech, providing information about hearing loss and its impact on comprehension.
- Otoacoustic Emissions (OAE) Testing:
- Measures sound waves produced in the inner ear, which can help detect hearing loss in newborns and children who cannot participate in conventional hearing tests.
- Brainstem Auditory Evoked Potentials (BAEPs) or Auditory Brainstem Response (ABR) Test:
- Measures the brain’s activity in response to sounds. It can detect hearing loss, especially in newborns, and also assess the brain pathways for hearing.
- Acoustic Reflex Testing:
- Measures the reflexive contraction of the middle ear muscles in response to loud sounds, which can help determine the location of the hearing problem.
Examples
Example 1: Managing Cataracts
- A patient diagnosed with cataracts experiences blurred and diminished vision. The nurse schedules regular eye examinations, facilitates surgical consultations, and educates the patient on postoperative care to restore visual clarity, ensuring they understand the recovery process and any potential complications.
Example 2: Treatment for Chronic Otitis Media
- For a patient suffering from recurrent otitis media, the nurse administers prescribed antibiotics, teaches the patient ear care techniques to prevent future infections, and recommends follow-up audiometric testing to assess any hearing impairment caused by the condition.
Example 3: Care for Age-Related Macular Degeneration (AMD)
- A patient with AMD struggles with central vision loss. The nurse assists in adapting the living environment to enhance safety, coordinates low vision aids, and educates the patient about potential lifestyle modifications that could slow the progression, such as nutritional supplementation with vitamins and antioxidants.
Example 4: Intervention for Noise-Induced Hearing Loss
- A factory worker exhibits signs of noise-induced hearing loss. The nurse conducts baseline audiometry, advocates for the use of protective earplugs or earmuffs in noisy environments, and provides education on the importance of regular hearing screenings to monitor any further auditory decline.
Example 5: Supporting a Patient with Glaucoma
- A patient with glaucoma needs help managing intraocular pressure to prevent optic nerve damage. The nurse teaches the patient how to correctly administer eye drops, discusses the importance of adhering to medication schedules, and arranges for periodic visual field tests to monitor the effectiveness of treatment.
Practice Questions
Question 1
What is the primary treatment for a patient diagnosed with cataracts?
A. Laser eye surgery
B. Prescription glasses
C. Cataract surgery
D. Steroid eye drops
Answer:
C. Cataract surgery
Explanation:
Cataract surgery is the primary treatment for cataracts, which involves removing the clouded lens and replacing it with a clear artificial lens. This procedure restores clear vision. Laser eye surgery (option A) is more commonly used for refractive errors, prescription glasses (option B) can help with vision but do not treat the cataract itself, and steroid eye drops (option D) are not a treatment for cataracts.
Question 2
Which test is used to diagnose glaucoma by measuring the pressure inside the eye?
A. Visual acuity test
B. Retinal scan
C. Tympanometry
D. Tonometry
Answer:
D. Tonometry
Explanation:
Tonometry is the diagnostic test used to measure intraocular pressure (IOP) and is essential for diagnosing and managing glaucoma. Elevated IOP is a major risk factor for glaucoma, which can lead to optic nerve damage. Visual acuity test (option A) and retinal scan (option B) assess different aspects of eye health, and tympanometry (option C) is used to evaluate middle ear function in audiology.
Question 3
A patient complaining of progressive hearing loss should undergo which diagnostic evaluation to assess inner ear function?
A. Audiometry
B. Ophthalmoscopy
C. Spirometry
D. Electrocardiogram (ECG)
Answer:
A. Audiometry
Explanation:
Audiometry is the standard diagnostic tool used to measure hearing acuity and assess both the type and degree of hearing loss. It is crucial for evaluating inner ear function and determining the appropriate management or intervention. Ophthalmoscopy (option B) examines the interior of the eye, spirometry (option C) assesses lung function, and an ECG (option D) measures heart rhythm and activity, none of which are relevant to hearing assessment.