Analgesics are essential medications used to relieve pain, a critical component of patient care in both acute and chronic conditions. For the NCLEX-RN® exam, understanding the classification, mechanisms of action, and nursing considerations of analgesics is crucial. These drugs are classified into non-opioid analgesics, opioid analgesics, and adjuvant analgesics, each with distinct uses, side effects, and nursing interventions. Key focus areas for NCLEX-RN® include pain assessment, respiratory monitoring, and patient education on drug safety, especially regarding opioid overdose and liver toxicity from acetaminophen.
Learning Objectives
In studying “Pharmacology: Analgesics” for the NCLEX-RN® exam, you should learn to understand the different classes of analgesics, including non-opioids, opioids, and adjuvant analgesics. Analyze the mechanisms of action, therapeutic uses, side effects, and contraindications of key drugs like acetaminophen, NSAIDs, and morphine. Evaluate the nursing considerations related to dosage limits, respiratory depression, and patient education. Additionally, explore how these medications are used to manage acute, chronic, and neuropathic pain. Apply your understanding to prioritize patient safety, interpret clinical scenarios, and answer NCLEX-style questions focusing on drug interactions, toxicity, and patient response to pain management interventions.
Classification of Analgesics
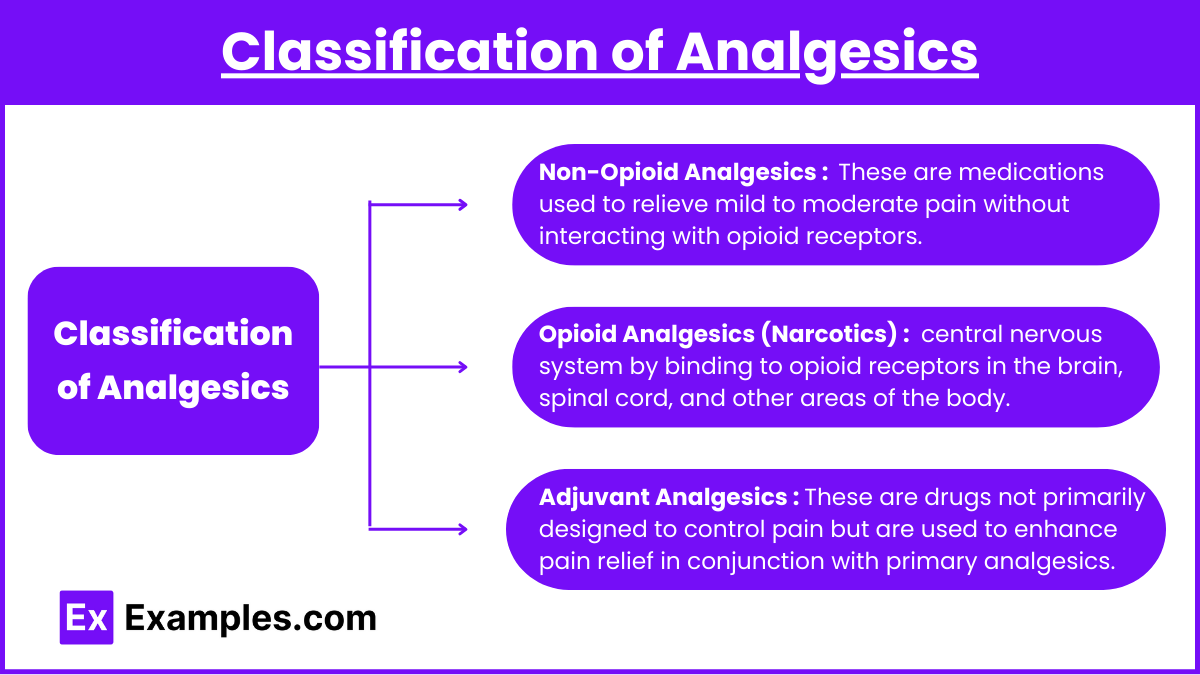
Analgesics are medications used to relieve pain, a critical component of patient care for those with acute, chronic, or postoperative pain. For the NCLEX-RN® exam, understanding analgesic drug classifications, mechanisms of action, nursing interventions, and patient education is crucial. Mastering this knowledge can significantly increase your chances of achieving a high score on the NCLEX-RN® exam. Analgesics are broadly classified into three main categories:
1. Non-Opioid Analgesics : These are medications used to relieve mild to moderate pain without interacting with opioid receptors. They typically include nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, and acetaminophen (paracetamol). They work by inhibiting the production of prostaglandins, which are chemicals that cause inflammation and pain.
- Examples: Acetaminophen (Tylenol), NSAIDs (Ibuprofen, Aspirin, Naproxen)
- Mechanism of Action:
- Inhibits cyclooxygenase (COX) enzymes to block prostaglandin production.
- Prostaglandins are responsible for pain, fever, and inflammation.
- Indications:
- Mild to moderate pain
- Fever
- Inflammation (only NSAIDs, not acetaminophen)
- Key Side Effects:
- Acetaminophen: Liver toxicity (hepatotoxicity) if taken in excess.
- NSAIDs: GI irritation, ulcers, bleeding, and nephrotoxicity (kidney damage).
- Nursing Interventions:
- Monitor for signs of liver damage (jaundice, elevated liver enzymes) in patients taking acetaminophen.
- Advise patients to avoid alcohol when taking acetaminophen.
- Monitor for GI bleeding and kidney function in patients taking NSAIDs.
- Educate patients not to exceed 4,000 mg/day of acetaminophen.
2. Opioid Analgesics (Narcotics) : These are powerful pain-relieving medications that act on the central nervous system by binding to opioid receptors in the brain, spinal cord, and other areas of the body. Examples include morphine, oxycodone, and fentanyl. They are used to treat moderate to severe pain, particularly in post-surgical, cancer, or chronic pain cases, but they carry a risk of dependence and addiction.
- Examples: Morphine, Hydromorphone (Dilaudid), Fentanyl, Oxycodone, Codeine
- Mechanism of Action:
- Binds to opioid receptors (mu, kappa, delta) in the brain, spinal cord, and peripheral tissues.
- Inhibits pain signals sent to the brain.
- Indications:
- Moderate to severe pain (e.g., post-surgical pain, cancer pain)
- Used as part of anesthesia or during labor and delivery.
- Key Side Effects:
- Respiratory depression (most severe)
- Constipation (common with chronic use)
- Sedation, dizziness, confusion
- Nausea and vomiting
- Urinary retention
- Opioid overdose can cause pinpoint pupils, respiratory depression, and unconsciousness.
- Nursing Interventions:
- Monitor respiratory rate. If the respiratory rate drops below 12 breaths per minute, hold the medication and notify the provider.
- Assess pain level before and after administration.
- Use a pain scale to determine the effectiveness of the drug.
- Antidote: Naloxone (Narcan) is used for opioid overdose.
- Educate the patient on the risk of addiction with long-term use.
3. Adjuvant Analgesics : These are drugs not primarily designed to control pain but are used to enhance pain relief in conjunction with primary analgesics. Examples include antidepressants (like amitriptyline) and anticonvulsants (like gabapentin), which can help manage neuropathic pain, and corticosteroids, which reduce inflammation-related discomfort.
- Examples: Antidepressants (Amitriptyline), Anticonvulsants (Gabapentin, Pregabalin), Corticosteroids (Dexamethasone)
- Mechanism of Action:
- These medications have properties that help with pain relief through indirect mechanisms.
- Antidepressants alter serotonin and norepinephrine levels.
- Anticonvulsants calm overactive nerve impulses.
- Indications:
- Used to treat neuropathic pain, fibromyalgia, and chronic pain conditions.
- Used as a supplement to opioids or non-opioids for better pain control.
- Key Side Effects:
- Drowsiness, dizziness (with anticonvulsants)
- Weight gain (with some anticonvulsants)
- GI upset, mood changes (with antidepressants)
- Nursing Interventions:
- Educate patients on the potential for drowsiness and sedation.
- Monitor for suicidal ideation in patients taking antidepressants.
- Encourage compliance, as some of these drugs require several weeks to achieve full effectiveness.
Common Uses of Analgesics
- Postoperative Pain: Opioids are frequently used to control pain after surgery.
- Chronic Pain: NSAIDs, opioids (with caution), and adjuvants (like antidepressants) are used.
- Neuropathic Pain: Adjuvant medications, especially anticonvulsants and antidepressants, are most effective.
- Headaches and Migraines: NSAIDs and certain adjuvants are used.
- Fever: Acetaminophen and NSAIDs (ibuprofen) are effective antipyretics.
Examples
Example 1. Acetaminophen (Tylenol)
Acetaminophen is a widely used non-opioid analgesic and antipyretic (fever reducer). It works by inhibiting prostaglandin synthesis in the central nervous system (CNS), which helps reduce pain and fever. Unlike NSAIDs, it does not have anti-inflammatory properties. It is often used for mild to moderate pain, such as headaches, menstrual cramps, and musculoskeletal pain. One of the most critical considerations for NCLEX-RN® is monitoring for liver toxicity (hepatotoxicity), especially in patients with pre-existing liver disease or those who consume excessive alcohol. The maximum daily dose for adults is 4,000 mg to prevent liver damage. Nurses should educate patients about the risks of liver injury and encourage them to avoid concurrent use of multiple acetaminophen-containing medications.
Example 2. Ibuprofen (Advil, Motrin)
Ibuprofen is a non-steroidal anti-inflammatory drug (NSAID) used to relieve mild to moderate pain, inflammation, and fever. It works by inhibiting the cyclooxygenase (COX) enzymes, reducing the production of prostaglandins, which are responsible for pain, fever, and inflammation. It is commonly prescribed for conditions such as arthritis, dysmenorrhea (menstrual cramps), and muscle pain. For NCLEX-RN®, it is essential to recognize that prolonged use can cause gastrointestinal (GI) bleeding, peptic ulcers, and kidney damage (nephrotoxicity). Patients should be advised to take ibuprofen with food or milk to reduce gastrointestinal discomfort. Nurses must monitor for signs of GI bleeding, such as black tarry stools, and ensure renal function tests (BUN, creatinine) are within normal limits for patients on long-term therapy.
Example 3. Morphine
Morphine is a powerful opioid analgesic used for the management of moderate to severe pain, particularly in post-surgical, cancer, and end-of-life (palliative) care. It works by binding to mu-opioid receptors in the central nervous system (CNS) to block the transmission of pain signals to the brain. For NCLEX-RN®, a key safety consideration is the risk of respiratory depression, especially in opioid-naive patients or those with underlying respiratory issues like COPD. Nurses should monitor the patient’s respiratory rate, and if it drops below 12 breaths per minute, the next dose should be withheld, and the healthcare provider notified. Another essential NCLEX topic is opioid overdose management, with Naloxone (Narcan) being the antidote. Side effects such as constipation, drowsiness, and sedation are common, and nurses should develop a bowel regimen for patients on long-term opioid therapy.
Example 4. Hydromorphone (Dilaudid)
Hydromorphone is a semi-synthetic opioid analgesic that is more potent than morphine. It is used to treat severe pain that does not respond to less potent analgesics. Like morphine, it binds to opioid receptors in the CNS, blocking the transmission of pain. For the NCLEX-RN®, nurses must be aware of its high potency and risk of respiratory depression. The same nursing considerations for morphine apply here, but special attention is given to dosing, as hydromorphone requires lower doses than morphine to achieve the same effect. Sedation, confusion, and drowsiness are common side effects, and patients are often placed on fall precautions. The antidote for hydromorphone overdose is Naloxone (Narcan). Nurses should also educate patients on proper use, especially if taking hydromorphone at home, to prevent misuse or overdose.
Example 5. Gabapentin (Neurontin)
Gabapentin is classified as an adjuvant analgesic rather than a primary pain reliever. It is originally an anticonvulsant but is widely used for neuropathic pain, such as pain caused by diabetic neuropathy, postherpetic neuralgia, and fibromyalgia. It works by inhibiting calcium channels in nerve cells, reducing nerve excitability. For NCLEX-RN®, nurses should focus on the side effects of drowsiness, dizziness, and confusion, especially in elderly patients. Patients should be advised not to operate heavy machinery or drive until they know how the drug affects them. Gradual discontinuation of gabapentin is essential to avoid withdrawal symptoms. Nurses should educate patients on the importance of compliance, as gabapentin requires several weeks of use before full effects are achieved. This is a key point for patient education on the NCLEX-RN®.
Practice Questions
Question 1
A nurse is caring for a patient who is prescribed morphine for severe postoperative pain. Which of the following findings would require the nurse to withhold the medication and notify the healthcare provider?
A) The patient reports a pain score of 7 out of 10.
B) The patient has a respiratory rate of 10 breaths per minute.
C) The patient reports nausea and vomiting.
D) The patient reports mild drowsiness and lethargy.
Answer: B) The patient has a respiratory rate of 10 breaths per minute.
Explanation : B is correct: Opioid analgesics like morphine have a primary side effect of respiratory depression. If a patient’s respiratory rate falls below 12 breaths per minute, the nurse must withhold the medication and notify the healthcare provider. Respiratory depression can lead to oxygen deprivation, making this a critical safety priority for the NCLEX-RN®.
- Why A is incorrect: A pain score of 7 out of 10 indicates moderate to severe pain, which is an indication for morphine administration, not a reason to withhold it.
- Why C is incorrect: Nausea and vomiting are common side effects of opioids. While these symptoms should be managed (e.g., by administering antiemetics), they do not warrant withholding the morphine.
- Why D is incorrect: Drowsiness and lethargy are normal effects of opioids. Unless the patient is excessively sedated or unarousable, this is not a reason to withhold the medication.
Question 2
A patient is taking acetaminophen (Tylenol) for the management of mild back pain. The nurse educates the patient about safe use of the medication. Which of the following statements made by the patient indicates the need for further teaching?
A) “I will avoid taking more than 4,000 mg of acetaminophen in one day.”
B) “I will avoid drinking alcohol while taking this medication.”
C) “I can take this medication with food to avoid an upset stomach.”
D) “I can take an over-the-counter cold medicine containing acetaminophen if I have a cold.”
Answer: D) “I can take an over-the-counter cold medicine containing acetaminophen if I have a cold.”
Explanation:
- Why D is correct: Many over-the-counter (OTC) cold and flu medications contain acetaminophen. If a patient takes both acetaminophen and an OTC product containing acetaminophen, they may exceed the daily limit of 4,000 mg, increasing the risk of liver toxicity (hepatotoxicity). The nurse should educate the patient to read labels carefully and avoid combining multiple acetaminophen-containing products.
- Why A is incorrect: This statement is correct. The daily limit for acetaminophen is 4,000 mg for adults, and taking more than this can result in liver damage. This is an important safety measure for the NCLEX-RN®.
- Why B is incorrect: This statement is correct. Combining acetaminophen with alcohol increases the risk of hepatotoxicity. The nurse should always educate the patient to avoid alcohol while taking acetaminophen.
- Why C is incorrect: This statement is correct, but it’s more applicable to NSAIDs like ibuprofen. Acetaminophen does not irritate the stomach lining like NSAIDs, so it does not need to be taken with food. However, this statement is still not dangerous or incorrect.
Question 3
A patient with diabetic neuropathy is prescribed gabapentin (Neurontin) to manage chronic nerve pain. Which of the following side effects should the nurse teach the patient to report to the healthcare provider immediately?
A) Mild drowsiness or dizziness
B) Nausea and occasional vomiting
C) Thoughts of self-harm or suicidal ideation
D) Weight gain of 2-3 pounds over 2 months
Answer: C) Thoughts of self-harm or suicidal ideation
Explanation:
- Why C is correct: Gabapentin (Neurontin) is classified as an adjuvant analgesic used to treat neuropathic pain. It can alter brain activity and increase the risk of suicidal ideation. The FDA requires healthcare providers to monitor patients for changes in mood, behavior, or thoughts of self-harm. If this occurs, the nurse must notify the provider immediately.
- Why A is incorrect: Drowsiness and dizziness are common side effects of gabapentin. While they should be monitored, they are expected effects, especially when first starting the drug.
- Why B is incorrect: Nausea and vomiting are mild, self-limiting side effects of many medications, including gabapentin. They do not require immediate intervention unless they are severe or persistent.
- Why D is incorrect: Weight gain is a known side effect of gabapentin, particularly with long-term use. This is not an emergency, but it should be monitored, especially if weight gain is rapid.