Assignment and delegation are essential components of leadership and management in nursing, ensuring safe and efficient patient care delivery. For the NCLEX-RN®, understanding these concepts helps nurses prioritize tasks, utilize team members effectively, and maintain accountability. Assignment involves distributing tasks based on scope of practice, while delegation requires transferring responsibilities while ensuring proper oversight. Mastering these skills enables nurses to make informed decisions, promote teamwork, and enhance patient outcomes, all of which are critical for success in the NCLEX-RN® exam.
Learning Objectives
In studying “Leadership & Management: Assignment/Delegation” for the NCLEX-RN® exam, you should learn to understand the principles of assigning and delegating tasks among healthcare team members. Analyze the Five Rights of Delegation and how they ensure safe, effective patient care. Evaluate the roles and scope of practice for RNs, LPNs, and UAPs to prioritize and allocate care activities appropriately. Explore frameworks like Maslow’s Hierarchy of Needs and the ABCs to guide decision-making. Apply these concepts to clinical scenarios, ensuring accountability, effective communication, and supervision, and interpret questions that test these principles in practice passages to enhance exam readiness.
Key Concepts of Assignment and Delegation
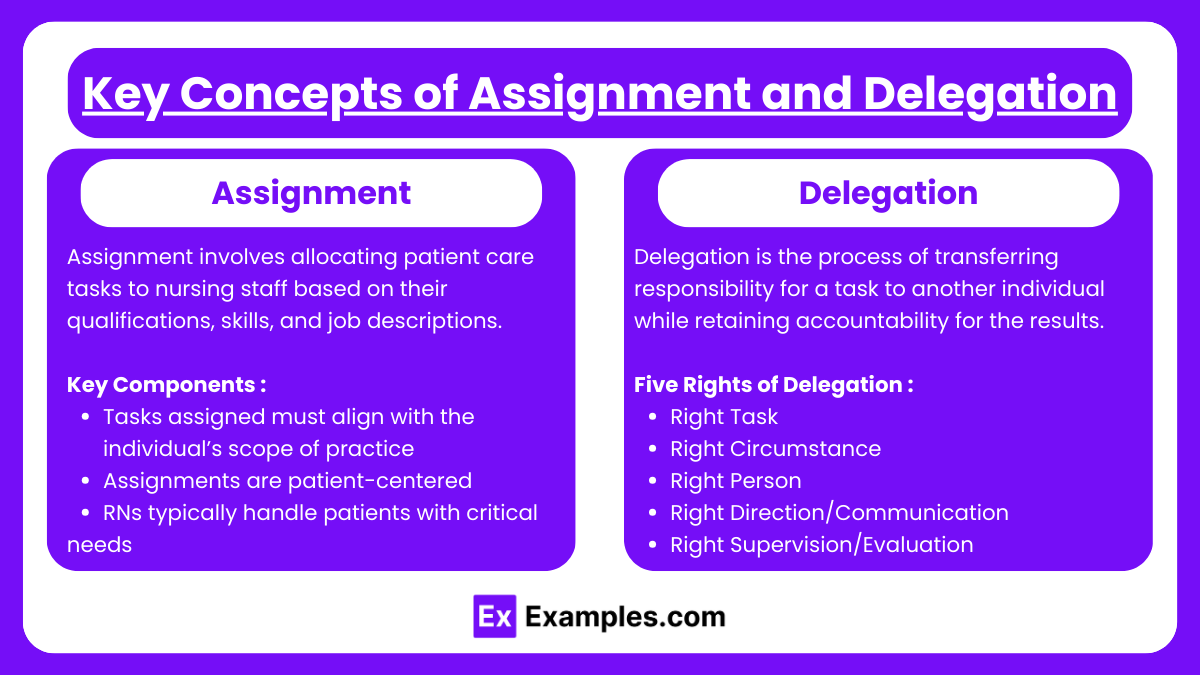
1. Assignment
- Assignment involves allocating patient care tasks to nursing staff based on their qualifications, skills, and job descriptions.
- Key Components:
- Tasks assigned must align with the individual’s scope of practice and legal parameters as outlined in the Nurse Practice Act.
- Assignments are patient-centered, focusing on the needs of the individual while optimizing the efficiency of the care team.
- RNs typically handle patients with critical or complex needs, while LPNs and UAPs manage stable patients requiring predictable care.
2. Delegation
- Delegation is the process of transferring responsibility for a task to another individual while retaining accountability for the results.
- Five Rights of Delegation:
- Right Task: Only delegate tasks that can safely be performed by another individual within their scope of practice.
- Right Circumstance: Delegate only when the patient’s condition is stable and predictable.
- Right Person: Choose a delegatee who possesses the necessary skills and training.
- Right Direction/Communication: Provide clear, detailed instructions, including the expected outcomes and any necessary follow-up.
- Right Supervision/Evaluation: Monitor the task’s completion and evaluate outcomes to ensure quality care.
- Delegation Challenges: Miscommunication, lack of training, or unclear expectations can compromise patient safety. Effective leadership is essential to prevent such issues.
Principles in Assignment
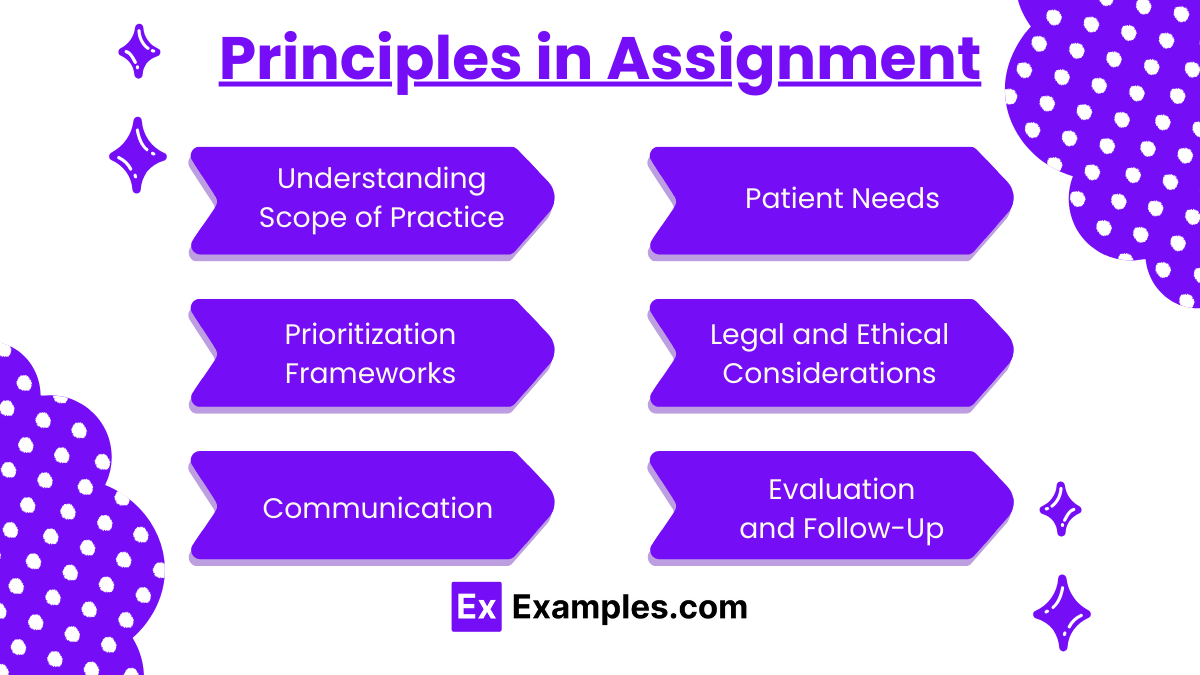
1. Understanding Scope of Practice
- Assign tasks based on the legal and professional scope of the team members.
- Ensure tasks align with the Nurse Practice Act and job descriptions.
- Recognize that RNs manage patients with complex needs, while LPNs/LVNs handle routine care, and UAPs assist with non-clinical tasks.
2. Patient Needs
- Match the complexity of patient care with the skill and competence of the assigned staff.
- Critical or unstable patients should remain under the care of an RN.
- Stable patients with predictable outcomes can be assigned to LPNs or UAPs.
3. Prioritization Frameworks
- Use Maslow’s Hierarchy of Needs, ABCs (Airway, Breathing, Circulation), and Safety to assign tasks that ensure immediate life-threatening conditions are addressed first.
- Ensure all assignments reflect patient safety and continuity of care.
4. Legal and Ethical Considerations
- Assignments must comply with institutional policies and state regulations.
- Avoid overloading staff, as this can compromise patient safety and quality of care.
- Ensure that assignments are equitable and promote teamwork.
5. Communication
- Provide clear, concise, and detailed instructions regarding the expectations of the assigned tasks.
- Include necessary patient-specific information, such as care plans, goals, and timelines.
6. Evaluation and Follow-Up
- Continuously monitor and evaluate the outcomes of the assigned tasks.
- Provide constructive feedback to the team and address any issues that arise.
- Ensure tasks are completed as per standards, and make adjustments to assignments if necessary to maintain patient safety and care quality.
Principles in Delegation

1. The Five Rights of Delegation
- Right Task: Ensure the task is appropriate for delegation based on patient condition and staff competence.
- Right Circumstance: Only delegate when the patient’s condition is stable and the task does not require clinical judgment.
- Right Person: Delegate to individuals who have the necessary training, knowledge, and skills.
- Right Direction/Communication: Provide clear, specific instructions and expectations, ensuring the delegatee fully understands.
- Right Supervision/Evaluation: Monitor the delegatee’s progress, provide feedback, and assess outcomes.
2. Accountability and Responsibility
- The RN retains accountability for the overall care plan and the outcomes of the delegated task.
- Delegate tasks only to individuals who are competent and confident in performing them.
- Ensure continuous supervision and support, intervening as necessary.
3. Building Trust and Teamwork
- Delegation requires a relationship of mutual trust between the RN and team members.
- Promote an environment where staff feel comfortable seeking clarification or reporting challenges.
- Use delegation as an opportunity to develop team members’ skills and confidence.
4. Recognizing Limitations
- Avoid delegating tasks requiring critical thinking, clinical judgment, or nursing assessments.
- Do not delegate activities that require specialized knowledge, such as patient education or managing a deteriorating patient.
5. Effective Supervision
- Regularly check on progress and provide guidance as needed.
- Evaluate outcomes and use them as a basis for improving future delegation practices.
- Offer feedback and acknowledgment to foster staff motivation and growth.
Examples
Example 1: Prioritizing Care in a Multi-Patient Assignment
An RN is managing a medical-surgical unit with a mix of stable and unstable patients. The RN assigns the care of two stable postoperative patients to the LPN. These patients require routine medication administration and basic wound care. The RN retains responsibility for a critically ill patient who requires frequent monitoring, titration of IV medications, and assessments. This prioritization ensures that complex tasks requiring clinical judgment are handled by the RN, while routine care is safely assigned to the LPN.
Example 2: Delegating Non-Clinical Tasks to UAPs
During a busy shift, the RN delegates non-clinical tasks such as assisting patients with bathing, feeding, and ambulation to the UAP. The RN provides clear instructions, such as reporting any changes in the patient’s condition (e.g., difficulty breathing during ambulation). This delegation allows the RN to focus on higher-priority clinical tasks, such as administering medications and assessing unstable patients.
Example 3: Managing a Patient Discharge
The RN is preparing a patient for discharge. The RN retains responsibility for providing discharge teaching, including medication instructions and follow-up care, as this task requires clinical judgment and patient education. The RN delegates the task of gathering the patient’s belongings and escorting them to their transportation to the UAP. This ensures efficient workflow while maintaining high-quality patient care.
Example 4: Handling a Code Situation
During a cardiac arrest in the unit, the RN takes charge of the situation, directing the resuscitation efforts and administering critical medications. The RN delegates tasks such as compressions to a trained UAP and asks an LPN to monitor and document the patient’s vital signs and response during the event. Effective communication and supervision ensure that each team member performs their role appropriately, contributing to the patient’s survival.
Example 5: Delegating Routine Procedures
The RN assigns the task of inserting a urinary catheter for a stable patient to the LPN, as this task falls within the LPN’s scope of practice. The RN ensures the LPN understands the procedure and the expected outcomes. After the task is completed, the RN evaluates the patient’s response to the intervention, maintaining accountability for the overall care.
Practice Questions
Question 1
A registered nurse (RN) is delegating tasks to a licensed practical nurse (LPN) and unlicensed assistive personnel (UAP). Which task should the RN delegate to the UAP?
A. Administering oral medications to a stable patient
B. Performing a sterile dressing change on a post-operative patient
C. Assisting a patient with ambulation to the bathroom
D. Conducting a focused assessment on a patient with chest pain
Answer: C. Assisting a patient with ambulation to the bathroom
Explanation:
- UAP Scope of Practice: UAPs are trained to perform non-clinical, routine tasks that do not require clinical judgment, such as ambulating, bathing, and feeding patients.
- LPN Responsibilities: Administering oral medications (A) and performing sterile dressing changes (B) fall within the scope of LPN practice.
- RN Responsibilities: Conducting focused assessments (D) involves clinical judgment, which is the responsibility of the RN.
- Delegating ambulation to the UAP allows the RN to focus on tasks requiring higher-level decision-making.
Question 2
The RN on a medical-surgical unit is assigning patients to the care team. Which patient should the RN assign to the LPN?
A. A patient admitted with unstable angina who is scheduled for a stress test
B. A patient receiving IV chemotherapy with a history of allergic reactions
C. A patient requiring frequent blood glucose monitoring and insulin administration
D. A patient newly diagnosed with a pulmonary embolism receiving IV heparin
Answer: C. A patient requiring frequent blood glucose monitoring and insulin administration
Explanation:
- Stable Patient: LPNs can care for stable patients with predictable outcomes, such as monitoring blood glucose and administering subcutaneous insulin.
- Critical and Complex Care: Patients with unstable angina (A), potential chemotherapy reactions (B), or a new pulmonary embolism on IV heparin (D) require ongoing assessment and critical thinking, which are within the RN’s scope.
- Assigning stable patients to the LPN ensures safe delegation and prioritizes the RN’s role in handling higher-acuity cases.
Question 3
Which of the following statements indicates the RN understands the “Right Supervision/Evaluation” principle of delegation?
A. “I will provide detailed instructions to the LPN and let them complete the task independently.”
B. “I will verify that the task was completed correctly and provide feedback as necessary.”
C. “I will assume the LPN knows how to handle the task because they are experienced.”
D. “I will only follow up with the LPN if the patient complains about the task.”
Answer: B. “I will verify that the task was completed correctly and provide feedback as necessary.”
Explanation:
- Right Supervision/Evaluation: Delegation requires the RN to monitor the task’s completion, ensure it was performed correctly, and provide guidance or feedback as needed.
- Option A: While detailed instructions are important, supervision and follow-up are still necessary.
- Option C: Assumptions about the delegatee’s experience without verification can compromise patient safety.
- Option D: Waiting for a patient complaint to evaluate task performance neglects the RN’s responsibility for oversight.


