Convert milliseconds to hours and vice versa at Examples.com. Input your values for immediate and reliable conversions.
ms to min
Formula: Time in minutes(min) = Time in milliseconds(ms) ∕ 60000
Milliseconds :
Minutes :
| milliseconds | minutes |
|---|---|
| 1 | 0.000016666666666666667 |
min to ms
Formula: Time in milliseconds(ms) = Time in minutes(min)x 60000
Minutes :
Milliseconds :
| minutes | milliseconds |
|---|---|
| 1 | 60000 |
Time Converters to Millisecond (mm)
Time Converters to Hour (hr)
| Nanosecond to Hour | Microsecond to Hour | Millisecond to Hour |
| Second to Hour | Minute to Hour | Day to Hour |
| Week to Hour | Month to Hour | Calendar Year to Hour |
| Decade to Hour | Century to Hour |
Conversion Factors:
- Milliseconds to Hours: 1 hour = 3,600,000 milliseconds
- Hours to Milliseconds: 1 millisecond = 1/3,600,000 hours
How to Convert Milliseconds to Hours:
To convert milliseconds to hours, divide the number of milliseconds by 3,600,000.
Hours=Milliseconds/3,600,000
Example:
Convert 7,200,000 milliseconds to hours.
Hours=7,200,000 ms/3,600,000=2 hr
How to Convert Hours to Milliseconds:
To convert hours to milliseconds, multiply the number of hours by 3,600,000.
Milliseconds=Hours×3,600,000
Example:
Convert 3 hours to milliseconds.
Milliseconds=3 hr×3,600,000=10,800,000 ms
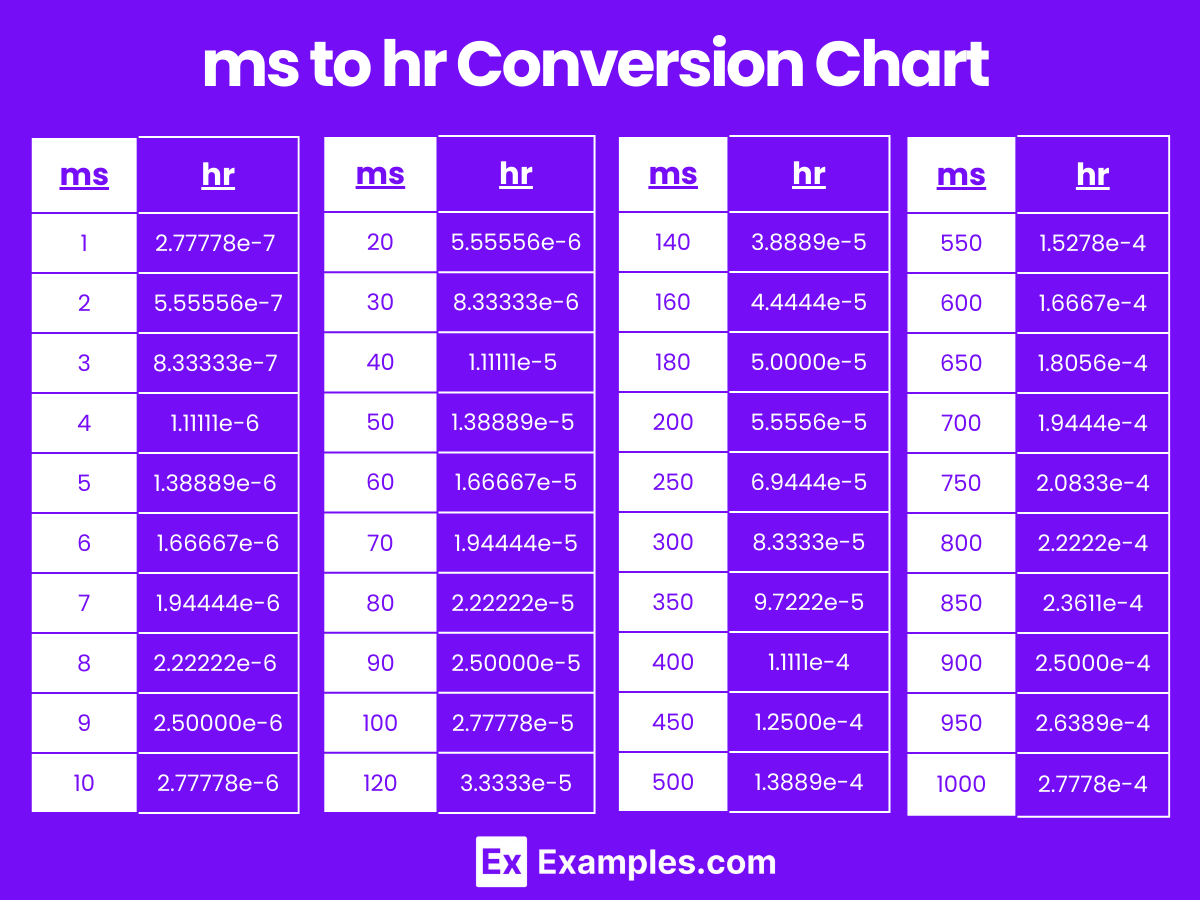
Milliseconds to Hours Conversion Table
| Milliseconds (ms) | Hours (hr) |
|---|---|
| 1 ms | 2.77778e-7 hr |
| 2 ms | 5.55556e-7 hr |
| 3 ms | 8.33333e-7 hr |
| 4 ms | 1.11111e-6 hr |
| 5 ms | 1.38889e-6 hr |
| 6 ms | 1.66667e-6 hr |
| 7 ms | 1.94444e-6 hr |
| 8 ms | 2.22222e-6 hr |
| 9 ms | 2.50000e-6 hr |
| 10 ms | 2.77778e-6 hr |
| 20 ms | 5.55556e-6 hr |
| 30 ms | 8.33333e-6 hr |
| 40 ms | 1.11111e-5 hr |
| 50 ms | 1.38889e-5 hr |
| 60 ms | 1.66667e-5 hr |
| 70 ms | 1.94444e-5 hr |
| 80 ms | 2.22222e-5 hr |
| 90 ms | 2.50000e-5 hr |
| 100 ms | 2.77778e-5 hr |
ms to hr Conversion Chart
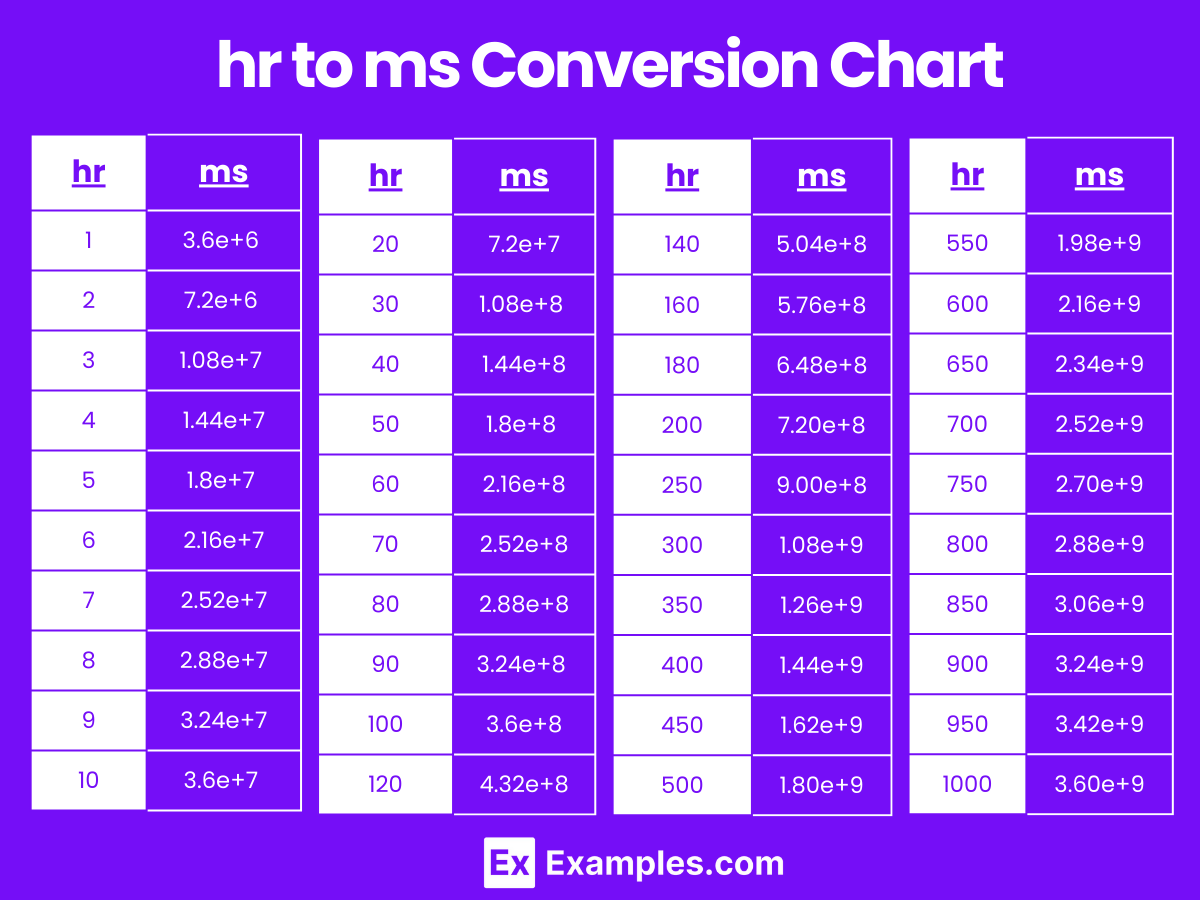
Hours to Milliseconds Conversion Table
| Hours (hr) | Milliseconds (ms) |
|---|---|
| 1 hr | 3.6e+6 ms |
| 2 hr | 7.2e+6 ms |
| 3 hr | 1.08e+7 ms |
| 4 hr | 1.44e+7 ms |
| 5 hr | 1.8e+7 ms |
| 6 hr | 2.16e+7 ms |
| 7 hr | 2.52e+7 ms |
| 8 hr | 2.88e+7 ms |
| 9 hr | 3.24e+7 ms |
| 10 hr | 3.6e+7 ms |
| 20 hr | 7.2e+7 ms |
| 30 hr | 1.08e+8 ms |
| 40 hr | 1.44e+8 ms |
| 50 hr | 1.8e+8 ms |
| 60 hr | 2.16e+8 ms |
| 70 hr | 2.52e+8 ms |
| 80 hr | 2.88e+8 ms |
| 90 hr | 3.24e+8 ms |
| 100 hr | 3.6e+8 ms |
hr to ms Conversion Chart
Difference Between Milliseconds to Hours
| Aspect | Milliseconds (ms) | Hours (hr) |
|---|---|---|
| Definition | A millisecond is one thousandth of a second. | An hour is equal to 60 minutes or 3600 seconds. |
| Symbol | ms | hr |
| Conversion Factor | 1 ms = 2.77778e-7 hr | 1 hr = 3,600,000 ms |
| Usage | Used for precise time measurements in short intervals. | Used for measuring longer time intervals. |
| Precision | Suitable for high-precision applications like computing and scientific research. | Suitable for general time measurements in daily life and scheduling. |
| Examples | 5000 ms = 0.00139 hr | 2 hr = 7,200,000 ms |
| Applications | Timing in sports, network latency, performance metrics, and scientific experiments. | Time management, work shifts, event scheduling, and travel durations. |
| Common Devices | Stopwatches, timers in software, system clocks in computers, and high-speed cameras. | Clocks, watches, timers, and scheduling devices. |
1. Solved Examples on Converting Milliseconds to Hours
Example 1:
Convert 7,200,000 milliseconds to hours.
Hours=7,200,000 ms/3,600,000=2 hr
Example 2:
Convert 1,800,000 milliseconds to hours.
Hours=1,800,000 ms/3,600,000=0.5 hr
Example 3:
Convert 360,000 milliseconds to hours.
Hours=360,000 ms/3,600,000=0.1 hr
Example 4:
Convert 10,800,000 milliseconds to hours.
Hours=10,800,000 ms/3,600,000=3 hr
Example 5:
Convert 54,000 milliseconds to hours.
Hours=54,000 ms/3,600,000=0.015 hr
2. Solved Examples on Converting Hours to Milliseconds
Example 1:
Convert 2 hours to milliseconds.
Milliseconds=2 hr×3,600,000=7,200,000 ms
Example 2:
Convert 0.5 hours to milliseconds.
Milliseconds=0.5 hr×3,600,000=1,800,000 ms
Example 3:
Convert 1 hour to milliseconds.
Milliseconds=1 hr×3,600,000=3,600,000 ms
Example 4:
Convert 3 hours to milliseconds.
Milliseconds=3 hr×3,600,000=10,800,000 ms
Example 5:
Convert 0.1 hours to milliseconds.
Milliseconds=0.1 hr×3,600,000=360,000 ms
Is converting milliseconds to hours commonly used in real-life applications?
Yes, converting milliseconds to hours is commonly used in various real-life applications such as tracking the duration of events, measuring time in scientific experiments, and managing long-duration processes.
Why is it important to convert milliseconds to hours?
Converting milliseconds to hours is important for understanding and managing longer time intervals in a more comprehensible format, especially in applications that deal with durations spanning several hours.
Why might engineers need to convert milliseconds to hours?
Engineers might need to convert milliseconds to hours to evaluate the operational duration of machinery and systems over extended periods, ensuring accurate maintenance schedules and performance assessments.
How does converting milliseconds to hours assist in server uptime monitoring?
Converting milliseconds to hours provides a clearer understanding of server uptime, making it easier to monitor and report on the reliability and performance of server systems.
How is converting milliseconds to hours beneficial in project management?
Converting milliseconds to hours helps project managers to allocate and track time for various tasks and milestones more effectively, ensuring better time management.
How does converting milliseconds to hours impact event scheduling?
Converting milliseconds to hours helps in scheduling events by providing a more understandable time format, which is crucial for planning and coordinating activities over longer periods.

