The cardiovascular system is a critical focus for the NCLEX-RN® exam, encompassing the heart, blood vessels, and blood flow essential for oxygenation and nutrient delivery. Key topics include cardiac anatomy, physiology, conduction pathways, hemodynamics, and regulation of blood pressure. Nurses must understand common cardiovascular conditions such as heart failure, hypertension, myocardial infarction, and arrhythmias. Additionally, the exam tests knowledge of nursing interventions, pharmacology, and patient education to promote cardiovascular health and manage complications effectively, ensuring comprehensive care for diverse patient populations.
Learning Objectives
In studying “Cardiovascular” for the NCLEX-RN® exam, you should learn to assess and manage cardiovascular conditions, including hypertension, heart failure, myocardial infarction, and arrhythmias. Understand diagnostic tools such as ECG, echocardiography, and laboratory tests like troponin and BNP. Analyze nursing interventions like medication administration, fluid balance monitoring, and promoting circulation. Evaluate the principles of patient education on lifestyle modifications and medication compliance. Additionally, explore the integration of prioritization frameworks (e.g., ABCs) in cardiovascular emergencies and the prevention of complications. Apply your knowledge to interpreting NCLEX-style scenarios and developing effective care plans to ensure safe, evidence-based patient care.
I. Anatomy and Physiology of the Cardiovascular System
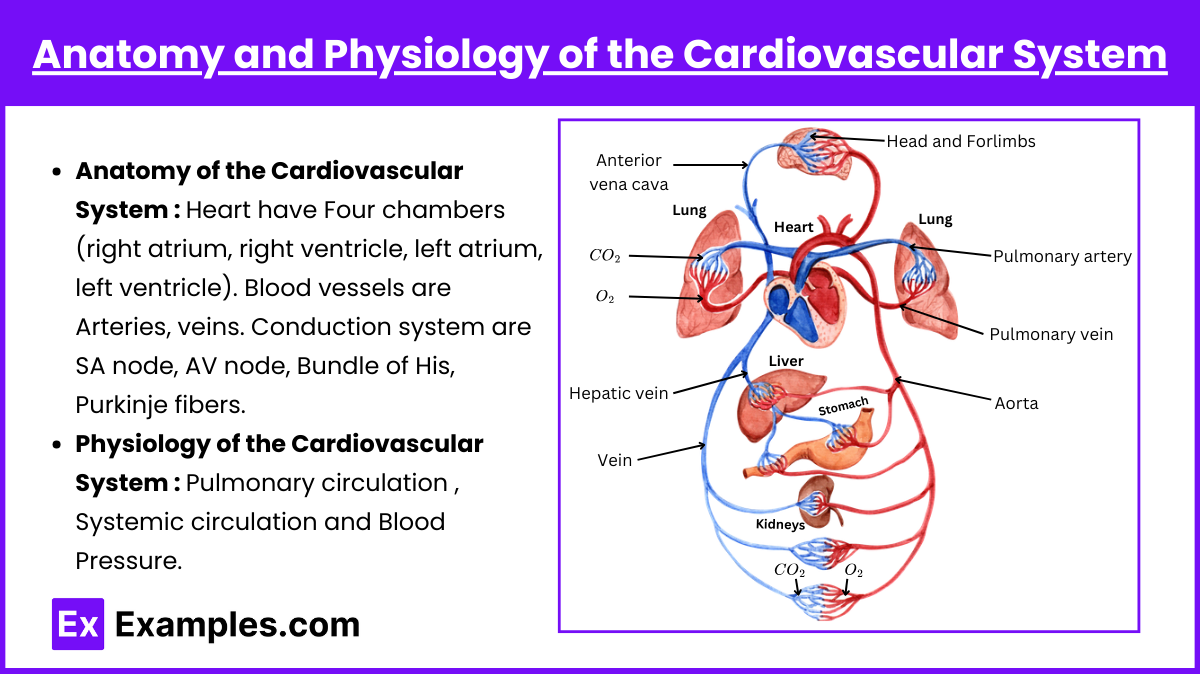
The cardiovascular system, also known as the circulatory system, consists of the heart, blood vessels, and blood, working together to deliver oxygen, nutrients, hormones, and other vital substances to tissues while removing waste products like carbon dioxide.
- Anatomy of the Cardiovascular System:
- Heart: Four chambers (right atrium, right ventricle, left atrium, left ventricle). The heart is a muscular organ located in the thoracic cavity, slightly left of the midline. It is the central pump of the cardiovascular system.
- Blood vessels: Arteries, veins, and capillaries.Blood vessels form a closed system that carries blood to and from the heart and tissues.
- Conduction system: SA node, AV node, Bundle of His, Purkinje fibers.
- SA Node: The heart’s natural pacemaker, initiating electrical impulses.
- AV Node: Delays impulses to allow ventricular filling.
- Bundle of His and Purkinje Fibers: Distribute impulses to ventricular muscle fibers.
- Physiology of the Cardiovascular System:
- Pulmonary circulation: Oxygenates blood.
- Systemic circulation: Distributes oxygenated blood.
- The cardiac cycle describes the sequence of events in a heartbeat
- Blood Pressure (BP) Force exerted by circulating blood on vessel walls.Measured in systolic (during contraction) and diastolic (during relaxation) pressures.
II. Cardiovascular Assessment
A thorough cardiovascular assessment is essential for identifying abnormalities and planning effective nursing interventions. This involves gathering subjective data, conducting a comprehensive physical examination, and analyzing diagnostic findings.
1. Subjective Data Collection : Understanding the patient’s experience, history, and risk factors is essential in cardiovascular assessment.
Key Components:
- Chief Complaints: Chest pain, shortness of breath, fatigue, dizziness, or swelling.
- Medical and Family History: Conditions like hypertension, diabetes, coronary artery disease, or congenital defects.
- Lifestyle Factors: Smoking, alcohol use, diet, exercise, and stress levels.
- Symptom Analysis: Details on onset, duration, frequency, intensity, and associated factors.
2. Physical Examination : A systematic evaluation of the cardiovascular system through inspection, palpation, and auscultation. which involves inspection, palpation, and auscultation to identify any abnormalities. Nurses assess the general appearance for cyanosis, pallor, or edema and inspect the chest wall for visible pulsations or heaving.
Key Steps:
- Inspection: Observing for cyanosis, pallor, edema, or visible pulsations in the chest and neck.
- Palpation: Assessing peripheral pulses (rate, rhythm, amplitude), apical impulse, thrills, or heaves.
- Auscultation: Listening to heart sounds (S1, S2), murmurs, rubs, or gallops with a stethoscope.
- Blood Pressure: Measuring in both arms and noting orthostatic changes.
3. Diagnostic Tools : Diagnostic tools play a critical role in confirming findings from the physical exam. An ECG identifies arrhythmias, ischemia, or myocardial infarction, while echocardiography assesses cardiac structure and function, including ejection fraction.
Common Tools:
- Electrocardiogram (ECG): Detects arrhythmias or ischemia.
- Echocardiography: Evaluates cardiac structure and function.
- Chest X-rays: Assesses heart size and pulmonary congestion.
- Blood Tests: Includes cardiac biomarkers (troponin, BNP) and lipid profiles.
- Stress Testing: Examines cardiovascular response to exercise.
- Doppler Ultrasound: Evaluates blood flow in peripheral arteries and veins.
4. Functional Assessments : Assessing cardiovascular performance under specific conditions provides valuable functional insights. functional assessments evaluate cardiovascular performance under specific conditions. Stress tests assess the heart’s response to exercise and help detect ischemia or arrhythmias, while Holter monitoring captures continuous ECG data to identify intermittent abnormalities.
Techniques:
- Stress Testing: Identifies ischemia or arrhythmias during exertion.
- Holter Monitoring: Records continuous ECG data to capture intermittent abnormalities.
- Capillary Refill: Checks peripheral circulation efficiency.
- Peripheral Vascular Examination: Evaluates signs of PAD or venous insufficiency.
III. Common Cardiovascular Disorders
- Hypertension:
- Definition: BP ≥ 140/90 mmHg (or as per guidelines).
- Nursing Interventions: Low-sodium diet, medication compliance, weight management.
- Coronary Artery Disease (CAD):
- Risk Factors: Smoking, obesity, diabetes.
- Nursing Priorities: Assess for angina, encourage lifestyle modifications.
- Heart Failure:
- Types: Left-sided (pulmonary symptoms), right-sided (systemic symptoms).
- Interventions: Diuretics, monitor for fluid overload, low-sodium diet.
- Arrhythmias:
- Symptoms: Chest pain, diaphoresis, nausea.
- Emergency Care: MONA (Morphine, Oxygen, Nitrates, Aspirin).
- Peripheral Artery Disease (PAD):
- Symptoms: Intermittent claudication, cold extremities.
- Nursing Actions: Promote circulation, avoid smoking.
IV. Nursing Interventions and Care Plans
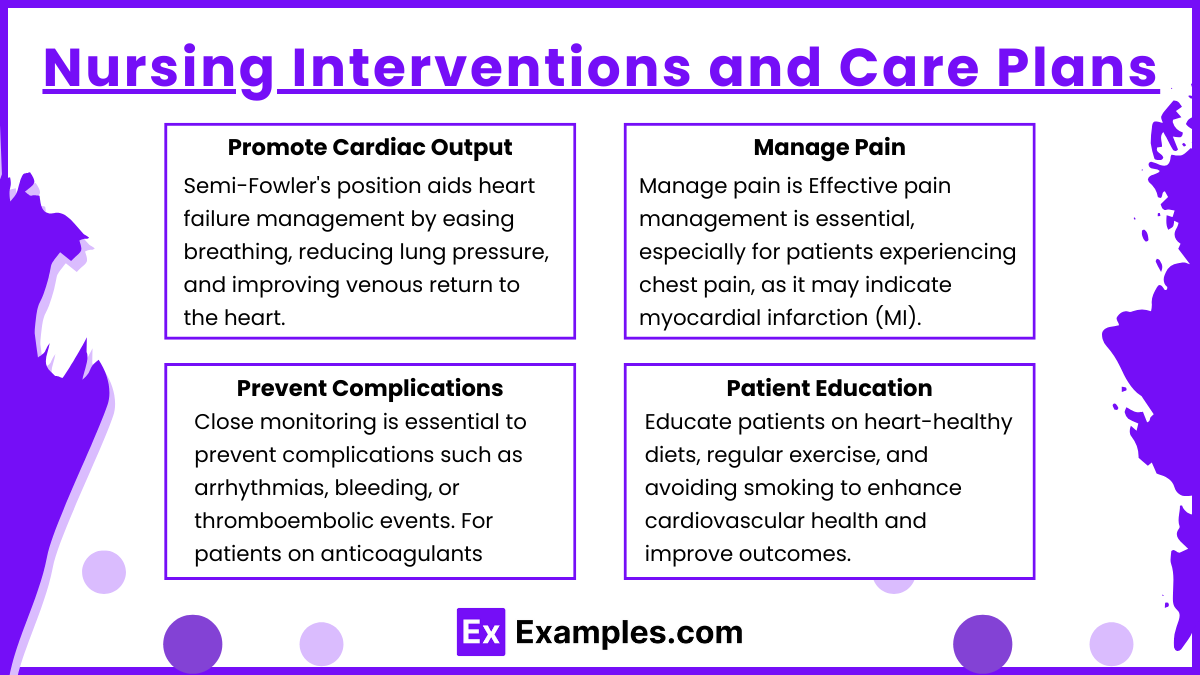
- Promote Cardiac Output : Positioning the patient in a semi-Fowler’s position is crucial for heart failure management, as it facilitates easier breathing by reducing the pressure on the lungs and improving venous return to the heart. Additionally, elevate the head of the bed as necessary to enhance oxygenation and comfort. Regularly monitor the patient’s fluid balance by tracking intake and output, as fluid overload can exacerbate heart failure symptoms. Assess vital signs, such as blood pressure, heart rate, and oxygen saturation, to evaluate the effectiveness of interventions and detect early signs of decompensation.
- Manage Pain : Effective pain management is essential, especially for patients experiencing chest pain, as it may indicate myocardial infarction (MI). Administer prescribed medications such as nitroglycerin to alleviate angina or morphine for severe MI-related pain. Alongside medication, assess and document the patient’s pain characteristics, including location, intensity, and duration, to guide treatment and monitor for changes that could signal complications. Encourage the patient to remain calm and reduce physical exertion to lower oxygen demand on the heart, minimizing further ischemia.
- Prevent Complications : Close monitoring is essential to prevent complications such as arrhythmias, bleeding, or thromboembolic events. For patients on anticoagulants, regularly assess for signs of bleeding, including bruising, hematuria, or gastrointestinal bleeding. Monitor cardiac rhythms for arrhythmias, which may require immediate intervention, such as administration of antiarrhythmic drugs or cardioversion. For immobilized patients, implement measures to prevent deep vein thrombosis (DVT), such as using compression stockings, encouraging leg exercises, and ensuring proper hydration.
- Patient Education : Empowering patients with knowledge is key to effective cardiovascular care. Educate them on the importance of lifestyle modifications, such as adopting a heart-healthy diet low in sodium and saturated fats, engaging in regular physical activity tailored to their condition, and completely abstaining from smoking to improve cardiac outcomes. Explain the purpose, dosage, and potential side effects of prescribed medications, emphasizing the importance of adherence to prevent disease progression. Provide resources and support for stress management, as chronic stress can adversely affect cardiovascular health. Ensure patients understand the signs and symptoms that warrant immediate medical attention, such as severe chest pain, shortness of breath, or sudden swelling.
Examples
Example 1: Hypertension Management
A patient presents with newly diagnosed hypertension. The NCLEX-RN® may ask about appropriate nursing interventions, such as educating the patient on a low-sodium diet, promoting regular exercise, and ensuring medication adherence (e.g., ACE inhibitors, beta-blockers). Priority questions may involve assessing the patient for complications like hypertensive crisis or organ damage, requiring immediate interventions like administering IV antihypertensives.
Example 2: Heart Failure Care
A question might focus on a patient admitted with left-sided heart failure, exhibiting symptoms like pulmonary edema, dyspnea, and fatigue. Nurses are expected to prioritize interventions such as elevating the head of the bed, administering diuretics, and monitoring oxygen saturation. NCLEX scenarios may also include evaluating a patient’s fluid status and educating them about fluid restrictions and daily weight monitoring.
Example 3: Myocardial Infarction (MI) Emergency
The exam may include a case study of a patient experiencing chest pain radiating to the left arm, nausea, and diaphoresis. Nurses must recognize these signs of an MI and prioritize interventions like initiating MONA protocol (Morphine, Oxygen, Nitrates, Aspirin) and preparing the patient for cardiac catheterization. NCLEX may also test the nurse’s ability to identify and manage post-MI complications, such as arrhythmias or cardiogenic shock.
Example 4: Deep Vein Thrombosis (DVT) Management
A question could involve a patient with unilateral leg swelling, redness, and warmth, suspected of having a DVT. The nurse’s priority actions include elevating the affected limb, avoiding massage, and initiating anticoagulant therapy (e.g., heparin). NCLEX questions may test knowledge on preventing complications like pulmonary embolism and educating patients on lifestyle modifications and medication adherence.
Example 5: Arrhythmia Recognition and Intervention
A patient may present with atrial fibrillation or ventricular tachycardia. NCLEX questions often require the nurse to interpret ECG findings, assess for hemodynamic stability, and implement interventions like administering antiarrhythmic medications or preparing for synchronized cardioversion. Patient education on long-term anticoagulation therapy to prevent stroke in atrial fibrillation cases may also be emphasized.
Practice Questions
Question 1
A patient is admitted with acute coronary syndrome (ACS). Which intervention should the nurse perform first?
A. Administer aspirin 325 mg orally.
B. Attach the patient to a cardiac monitor.
C. Administer sublingual nitroglycerin.
D. Obtain a 12-lead electrocardiogram (ECG).
Answer: D. Obtain a 12-lead electrocardiogram (ECG).
Explanation: Obtaining a 12-lead ECG is the top priority as it identifies myocardial ischemia or infarction. This directs immediate treatment decisions, such as thrombolysis or PCI. Aspirin, cardiac monitoring, and nitroglycerin are important but must follow an ECG to ensure appropriate and safe interventions.
Why the Other Options Are Incorrect:
- A: Aspirin is essential for platelet inhibition but is given after an ECG confirms ACS.
- B: Cardiac monitoring is important but does not provide diagnostic information as quickly as an ECG.
- C: Nitroglycerin relieves chest pain but may be contraindicated in conditions like hypotension or right ventricular infarction, which the ECG identifies.
Question 2
A patient with a history of heart failure reports a 3-pound weight gain in 2 days, fatigue, and mild dyspnea. What is the nurse’s priority intervention?
A. Encourage the patient to rest and monitor symptoms.
B. Increase the dose of the patient’s diuretic medication.
C. Assess lung sounds and check oxygen saturation.
D. Contact the healthcare provider to report the findings.
Answer: C. Assess lung sounds and check oxygen saturation.
Explanation: Rapid weight gain, fatigue, and dyspnea indicate possible fluid overload or worsening heart failure. The nurse must assess lung sounds and oxygen levels to detect signs of pulmonary congestion or hypoxia, which guide further interventions.
Why the Other Options Are Incorrect:
- A: Resting and monitoring symptoms delays assessment and may worsen the patient’s condition.
- B: Adjusting medication dosage requires provider approval and should be based on a full assessment.
- D: Contacting the provider is necessary, but assessment data must be gathered first to report meaningful findings.
Question 3
A nurse is caring for a patient receiving IV heparin therapy for a deep vein thrombosis (DVT). Which laboratory value requires immediate intervention?
A. Hemoglobin: 14 g/dL.
B. Platelet count: 80,000/mm³.
C. Prothrombin time (PT): 13 seconds.
D. Activated partial thromboplastin time (aPTT): 50 seconds.
Answer: B. Platelet count: 80,000/mm³.
Explanation: A platelet count of 80,000/mm³ suggests potential heparin-induced thrombocytopenia (HIT), a life-threatening condition. The nurse must stop heparin and notify the provider immediately.
Why the Other Options Are Incorrect:
- A: Hemoglobin of 14 g/dL is within normal range and does not indicate bleeding or other immediate concerns.
- C: PT monitors warfarin therapy, not heparin. It is irrelevant in this context.
- D: An aPTT of 50 seconds is below the therapeutic range for heparin (60-80 seconds) but is not as critical as the platelet count in this scenario.