Cardiovascular focuses on the management of life-threatening heart conditions and hemodynamic instability in critically ill patients. It encompasses acute coronary syndromes, arrhythmias, heart failure, cardiogenic shock, and postoperative cardiac care. Nurses play a pivotal role in monitoring, interpreting diagnostic findings, and implementing lifesaving interventions. Mastery of pharmacology, advanced monitoring techniques, and rapid decision-making is essential to optimize outcomes. Effective care requires a comprehensive understanding of cardiovascular physiology, early recognition of complications, and the ability to respond promptly to evolving clinical situations.
Learning Objectives
In studying “Critical Care: Cardiovascular” for the NCLEX-RN®, you should learn to understand the management of critical cardiovascular conditions such as myocardial infarction, arrhythmias, heart failure, and shock. Analyze the application of advanced monitoring techniques, including ECG interpretation and hemodynamic assessments, to identify cardiac dysfunction. Evaluate the principles of interventions like defibrillation, medication titration, and mechanical circulatory support (e.g., IABP). Additionally, explore the integration of pharmacologic therapies and nursing care strategies to stabilize patients, prevent complications, and improve outcomes. Apply this knowledge to interpreting case scenarios and making evidence-based decisions in NCLEX-style questions.
1.Cardiovascular Anatomy and Physiology
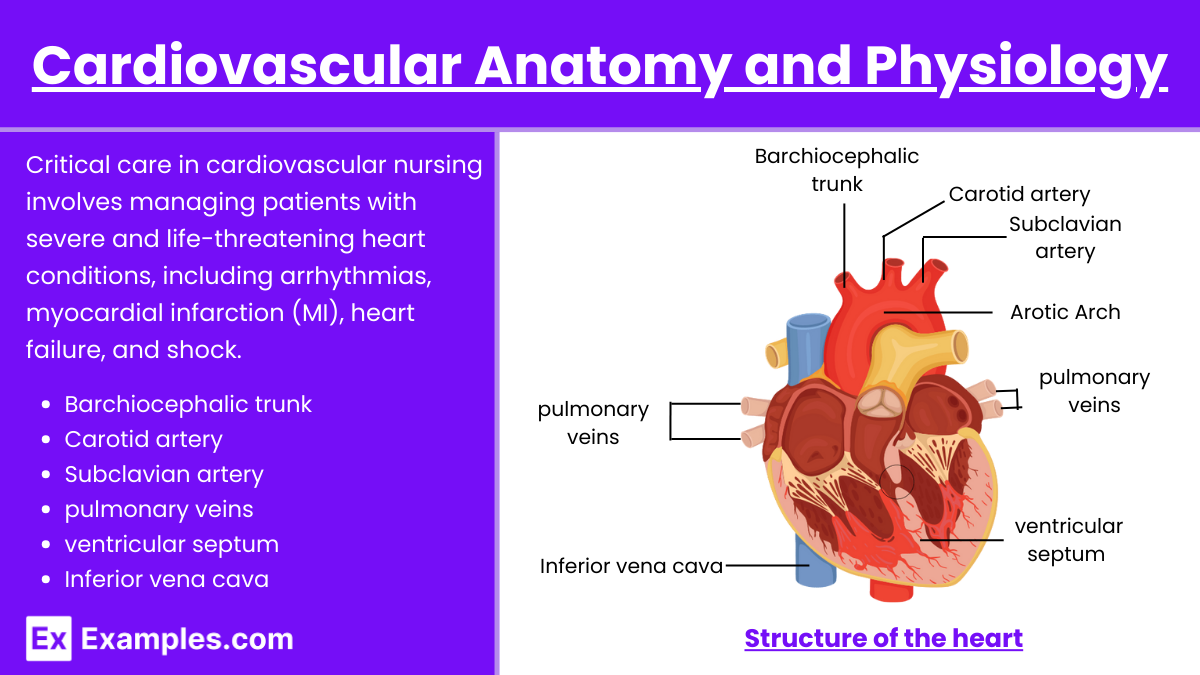
Critical care in cardiovascular nursing involves managing patients with severe and life-threatening heart conditions, including arrhythmias, myocardial infarction (MI), heart failure, and shock. Nurses play a pivotal role in monitoring, diagnosing, and implementing lifesaving interventions in a high-stakes environment.
- Understanding the structure and function of the heart and blood vessels.
- Cardiac cycle: Systole and diastole.
- Electrical conduction system: SA node, AV node, Bundle of His, Purkinje fibers.
- Hemodynamic principles: Preload, afterload, cardiac output (CO), and ejection fraction.
2. Assessment and Monitoring
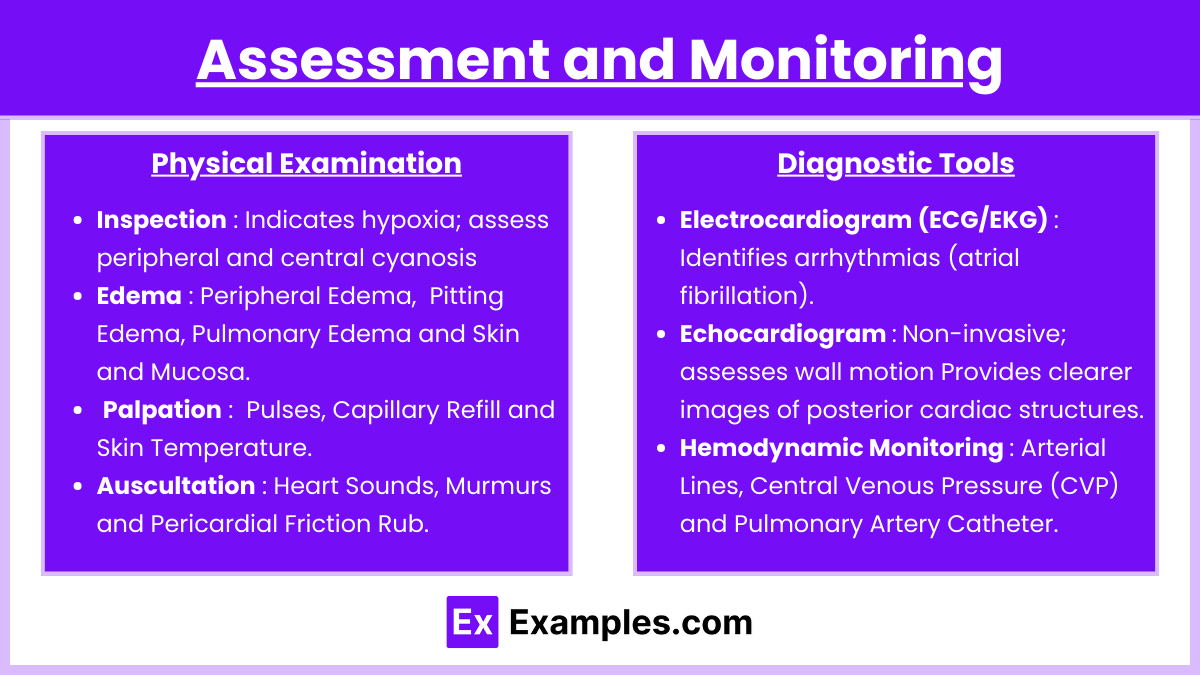
Thorough assessment and continuous monitoring are foundational in managing critically ill cardiovascular patients. Here’s an expanded view on key components:
Physical Examination :
- Inspection
- Cyanosis: Indicates hypoxia; assess peripheral and central cyanosis (lips, nail beds, extremities).
- Jugular Vein Distension (JVD): Suggests elevated central venous pressure (CVP) and right-sided heart failure.
- Edema:
- Peripheral Edema: Seen in lower extremities due to venous congestion.
- Pitting Edema: Associated with fluid overload or chronic heart failure.
- Pulmonary Edema: Evident as pink frothy sputum or crackles on auscultation.
- Skin and Mucosa: Check for pallor, diaphoresis, or mottling, which may indicate poor perfusion or shock.
- Palpation
- Pulses:
- Assess for rate, rhythm, and strength (bounding, weak, or thready).
- Compare bilaterally for equality and symmetry.
- Peripheral pulses (dorsalis pedis, posterior tibial) provide information about perfusion.
- Capillary Refill: Delayed refill (>2 seconds) suggests poor peripheral perfusion.
- Skin Temperature:
- Cool, clammy skin indicates vasoconstriction and poor perfusion.
- Warm, flushed skin may indicate sepsis or systemic vasodilation.
- Pulses:
- Auscultation
- Heart Sounds:
- S1 and S2: Assess regularity and presence of splitting.
- S3 (ventricular gallop): Common in heart failure, indicative of fluid overload.
- S4 (atrial gallop): Suggests non-compliant ventricles, often in hypertensive heart disease.
- Murmurs:
- Determine timing (systolic, diastolic, continuous) and intensity.
- Commonly caused by valvular disease (e.g., aortic stenosis, mitral regurgitation).
- Pericardial Friction Rub: Indicative of pericarditis.
- Heart Sounds:
Diagnostic Tools :
- Electrocardiogram (ECG/EKG)
- Identifies arrhythmias (atrial fibrillation, ventricular tachycardia).
- Detects ischemia or infarction (ST-segment elevation or depression, T-wave inversions).
- Evaluates QT interval prolongation, which can predispose to torsades de pointes.
- Echocardiogram
- Transthoracic (TTE): Non-invasive; assesses wall motion, ejection fraction, and valve function.
- Transesophageal (TEE): Provides clearer images of posterior cardiac structures, used in endocarditis or clots.
- Hemodynamic Monitoring
- Arterial Lines:
- Direct blood pressure measurement in real-time.
- Allows arterial blood sampling for ABG analysis.
- Central Venous Pressure (CVP):
- Measures right atrial pressure.
- Guides fluid resuscitation or diuresis.
- Pulmonary Artery Catheter (Swan-Ganz):
- Measures pulmonary artery pressure, cardiac output, and pulmonary capillary wedge pressure (PCWP).
- Useful in differentiating types of shock (cardiogenic vs. septic).
- Arterial Lines:
3. Common Cardiovascular Emergencies
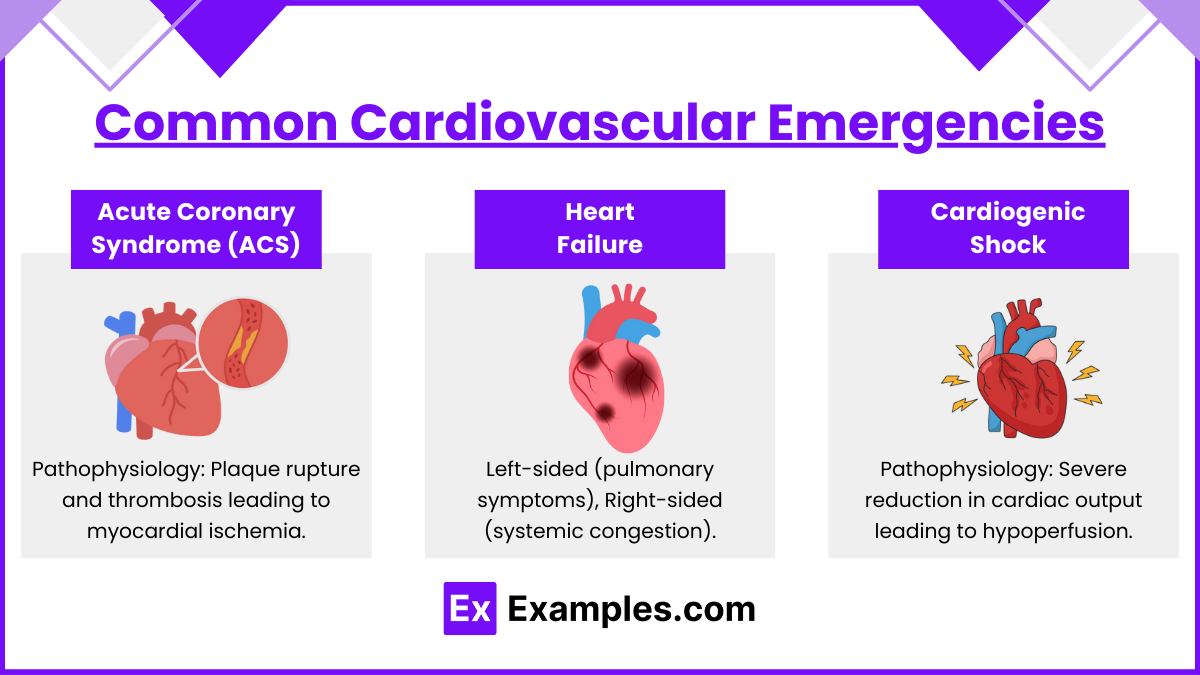
- Acute Coronary Syndrome (ACS):
- Pathophysiology: Plaque rupture and thrombosis leading to myocardial ischemia.
- Types: Unstable angina, NSTEMI, STEMI.
- Management:
- MONA: Morphine, Oxygen, Nitroglycerin, Aspirin.
- Thrombolytics or Percutaneous Coronary Intervention (PCI).
- Beta-blockers, ACE inhibitors, anticoagulants (e.g., heparin).
- Heart Failure:
- Types: Left-sided (pulmonary symptoms), Right-sided (systemic congestion).
- Management:
- Diuretics, ACE inhibitors, beta-blockers, digoxin.
- Monitor for fluid overload and electrolyte imbalances.
- Cardiogenic Shock:
- Pathophysiology: Severe reduction in cardiac output leading to hypoperfusion.
- Management:
- Inotropes (e.g., dobutamine), vasopressors (e.g., norepinephrine).
- Mechanical support: Intra-aortic balloon pump (IABP), ventricular assist devices (VADs).
4. Arrhythmias
- Life-Threatening Arrhythmias:
- Ventricular Tachycardia (VT): Can lead to ventricular fibrillation (VF).
- Ventricular Fibrillation (VF): Requires immediate defibrillation.
- Asystole/PEA (Pulseless Electrical Activity): High-quality CPR and epinephrine.
- Bradyarrhythmias:
- Symptomatic bradycardia: Managed with atropine, transcutaneous pacing.
- Tachyarrhythmias:
- Supraventricular Tachycardia (SVT): Vagal maneuvers, adenosine, synchronized cardioversion.
Examples
Example 1. Acute Myocardial Infarction (MI) Management
Patients presenting with an MI require immediate interventions to restore blood flow to the heart muscle and prevent further damage. The nurse’s role includes administering oxygen, nitroglycerin, morphine, and aspirin (MONA protocol), preparing the patient for reperfusion therapy (thrombolytics or percutaneous coronary intervention), and monitoring for complications like arrhythmias or cardiogenic shock. Nurses must interpret ECG changes, assess for chest pain, and continuously monitor vital signs to prevent adverse outcomes.
Example 2. Ventricular Fibrillation and Defibrillation
Ventricular fibrillation (VF) is a life-threatening arrhythmia requiring immediate action. The nurse must perform high-quality CPR while preparing the defibrillator for shock delivery. Administering medications like epinephrine or amiodarone and ensuring accurate rhythm interpretation are critical. Nurses must also provide post-resuscitation care, which includes maintaining hemodynamic stability, monitoring for recurrence of VF, and assessing for potential hypoxic or neurological complications.
Example 3. Cardiogenic Shock Management
In cardiogenic shock, the heart fails to pump sufficient blood to meet the body’s needs, leading to tissue hypoperfusion. Nurses manage this condition by initiating inotropes like dobutamine, administering vasopressors such as norepinephrine, and providing mechanical support like an intra-aortic balloon pump (IABP). Continuous hemodynamic monitoring, maintaining fluid balance, and preventing further organ dysfunction are essential responsibilities in managing this critical cardiovascular condition.
Example 4. Postoperative Care for Cardiac Surgery
Patients recovering from procedures such as coronary artery bypass grafting (CABG) or valve replacement require close monitoring for complications like bleeding, infection, arrhythmias, or fluid imbalance. Nurses manage chest tubes, titrate vasoactive medications, and assess for signs of cardiac tamponade or reduced cardiac output. Pain control and patient education about activity restrictions and wound care are also integral parts of postoperative care in cardiovascular critical care.
Example 5. Acute Heart Failure in Critical Care
Acute heart failure often manifests as pulmonary edema or systemic congestion, requiring prompt intervention. Nurses administer diuretics to reduce fluid overload, nitroglycerin to decrease preload, and oxygen therapy to alleviate respiratory distress. Monitoring oxygen saturation, blood pressure, and response to medications is crucial. Education about sodium restriction and medication adherence is essential for long-term management, even in a critical care setting.
Practice Questions
Question 1
A patient in the intensive care unit (ICU) is admitted with acute heart failure. The nurse notes crackles in the lungs, jugular vein distension (JVD), and pitting edema. Which intervention should the nurse anticipate first?
A. Administer a loop diuretic like furosemide.
B. Insert a central venous catheter for fluid administration.
C. Prepare the patient for hemodialysis.
D. Administer an intravenous bolus of normal saline.
Answer: A. Administer a loop diuretic like furosemide.
Explanation: The patient is exhibiting signs of fluid overload, a hallmark of acute heart failure. Loop diuretics such as furosemide are first-line medications to remove excess fluid, reduce pulmonary congestion, and improve symptoms like crackles and edema. Administering normal saline (Option D) would exacerbate the fluid overload. While inserting a central venous catheter (Option B) may be necessary later for monitoring or medication administration, it is not the immediate priority. Hemodialysis (Option C) is reserved for severe cases of fluid overload unresponsive to diuretics or for patients with renal failure.
Question 2
A patient with a history of myocardial infarction (MI) is admitted for chest pain. Their ECG shows ST-segment elevation. What is the priority nursing action?
A. Prepare the patient for immediate percutaneous coronary intervention (PCI).
B. Administer sublingual nitroglycerin and reassess pain.
C. Administer morphine for pain relief.
D. Obtain a detailed history of the chest pain.
Answer: A. Prepare the patient for immediate percutaneous coronary intervention (PCI).
Explanation: ST-segment elevation indicates an acute myocardial infarction (STEMI), requiring immediate reperfusion to restore blood flow to the myocardium. Percutaneous coronary intervention (PCI) is the gold standard treatment for STEMI and must be initiated promptly to minimize myocardial damage. Nitroglycerin (Option B) and morphine (Option C) are part of symptom management but do not address the underlying ischemia. Obtaining a detailed history (Option D) can be done after initiating life-saving measures.
Question 3
The nurse is monitoring a patient on a pulmonary artery catheter. The pulmonary capillary wedge pressure (PCWP) is elevated, and the patient exhibits shortness of breath and orthopnea. What is the nurse’s priority intervention?
A. Administer a bolus of intravenous fluids.
B. Administer a diuretic to reduce fluid volume.
C. Increase the infusion rate of the inotropic medication.
D. Notify the healthcare provider and prepare for intubation.
Answer: B. Administer a diuretic to reduce fluid volume.
Explanation : An elevated pulmonary capillary wedge pressure (PCWP) indicates left ventricular failure and fluid overload, contributing to pulmonary congestion and shortness of breath. Diuretics (Option B) are the priority intervention to reduce fluid volume and alleviate symptoms. Administering additional fluids (Option A) would worsen the situation. Increasing inotropes (Option C) may be appropriate for low cardiac output but is not indicated as the first step for fluid overload. Intubation (Option D) may be required if the patient decompensates, but addressing fluid overload early can prevent the need for this intervention.