The endocrine system is vital in maintaining homeostasis by producing hormones that regulate metabolism, growth, reproduction, and stress responses. Key glands include the pituitary, thyroid, adrenal glands, pancreas, and parathyroids. For the NCLEX-RN® exam, a solid understanding of common endocrine disorders such as diabetes mellitus, thyroid imbalances, adrenal dysfunctions, and their associated complications is crucial. Nurses must prioritize assessment, early intervention, and patient education to ensure optimal outcomes. Mastering these concepts aids in providing comprehensive care and excelling on the NCLEX-RN®.
Learning Objectives
In studying "Adult Health: Endocrine" for the NCLEX-RN®, you should learn to understand the pathophysiology, assessment, and management of common endocrine disorders such as diabetes mellitus, thyroid dysfunctions, adrenal insufficiency, and pituitary abnormalities. Analyze how hormonal imbalances affect homeostasis and systemic functions. Evaluate nursing interventions, including medication administration, patient education, and monitoring for complications like diabetic ketoacidosis or thyroid storm. Additionally, explore the role of laboratory tests in diagnosing endocrine disorders and develop the ability to prioritize care for patients in acute and chronic states. Apply this understanding to interpreting clinical scenarios and answering NCLEX practice questions effectively.
Overview of the Endocrine System
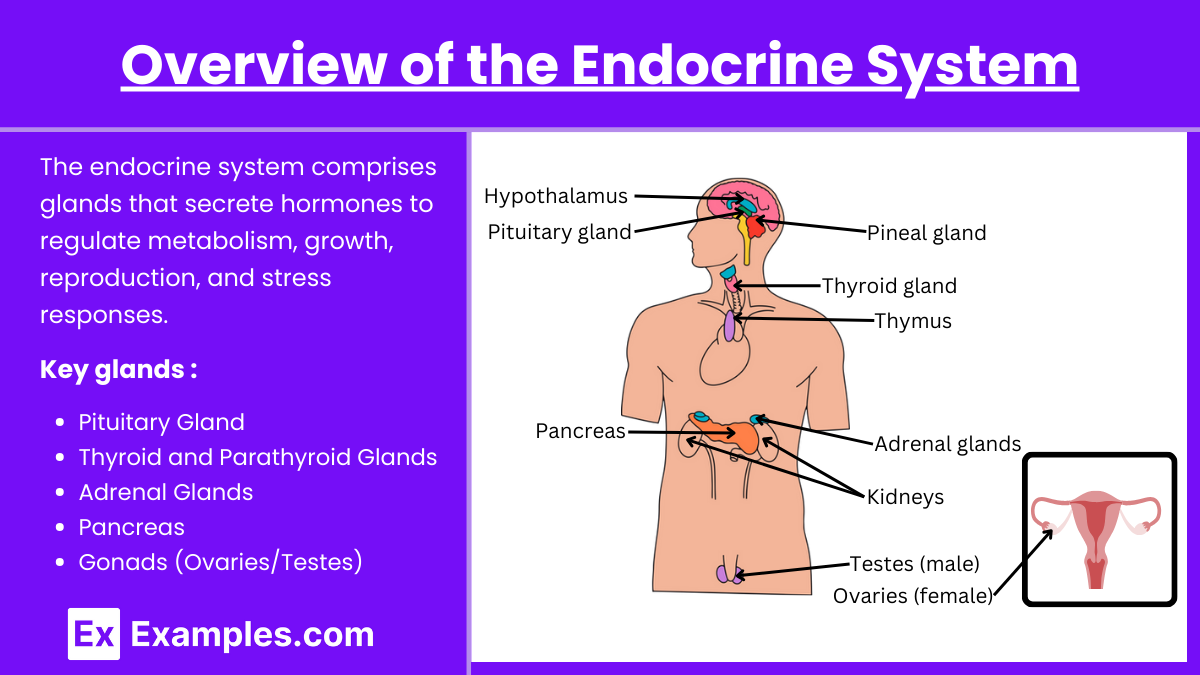
The endocrine system is critical in maintaining homeostasis through hormonal regulation. Understanding endocrine disorders is essential for success on the NCLEX-RN®, as this topic frequently appears in exam questions. The endocrine system comprises glands that secrete hormones to regulate metabolism, growth, reproduction, and stress responses.
Key glands:
Pituitary Gland: Master gland controlling other endocrine glands.
Thyroid and Parathyroid Glands: Regulate metabolism and calcium levels.
Adrenal Glands: Control stress response and electrolyte balance.
Pancreas: Regulates blood glucose via insulin and glucagon.
Gonads (Ovaries/Testes): Responsible for sexual development and reproduction.
Common Endocrine Disorders
1. Diabetes Mellitus
Type 1: Autoimmune destruction of beta cells in the pancreas; requires insulin.
Type 2: Insulin resistance; often managed with oral hypoglycemics and lifestyle changes.
Complications:
Hypoglycemia: Confusion, diaphoresis, tremors.
Hyperglycemia: Polyuria, polydipsia, polyphagia.
Diabetic Ketoacidosis (DKA): Fruity breath, Kussmaul respirations.
Hyperosmolar Hyperglycemic State (HHS): Severe hyperglycemia without ketosis.
NCLEX Tip: Focus on blood glucose monitoring, signs of hypo-/hyperglycemia, and medication administration.
2. Thyroid Disorders
Hyperthyroidism (e.g., Graves' disease):
Symptoms: Tachycardia, weight loss, heat intolerance.
Management: Antithyroid medications (methimazole), beta-blockers, radioactive iodine therapy.
Hypothyroidism (e.g., Hashimoto's thyroiditis):
Symptoms: Fatigue, weight gain, cold intolerance, bradycardia.
Management: Levothyroxine therapy (monitor for signs of overdose: tachycardia, insomnia).
NCLEX Tip: Prioritize airway in thyroid storm and educate on lifelong medication for hypothyroidism.
3. Adrenal Disorders
Cushing's Syndrome: Excess cortisol.
Symptoms: Moon face, truncal obesity, striae, hypertension.
Management: Treat the underlying cause (e.g., tumor removal).
Addison’s Disease: Insufficient cortisol.
Symptoms: Fatigue, weight loss, hyperpigmentation, hypotension.
Management: Corticosteroid replacement, stress dose during illness.
NCLEX Tip: Addisonian crisis is a medical emergency; treat with IV steroids and fluids.
4. Parathyroid Disorders
Hyperparathyroidism: High calcium levels.
Symptoms: Bone pain, kidney stones, muscle weakness.
Management: Surgery, hydration.
Hypoparathyroidism: Low calcium levels.
Symptoms: Tetany, Chvostek's and Trousseau's signs.
Management: Calcium and vitamin D supplementation.
NCLEX Tip: Recognize symptoms of calcium imbalances.
5. Pituitary Disorders
Acromegaly/Gigantism: Excess growth hormone; manage with surgical removal of tumor.
Diabetes Insipidus (DI): Lack of ADH.
Symptoms: Polyuria, polydipsia, dilute urine.
Management: Desmopressin, hydration.
SIADH: Excess ADH.
Symptoms: Fluid retention, hyponatremia.
Management: Fluid restriction, hypertonic saline.
Nursing Interventions and Priorities
Nursing interventions and priorities refer to the planned actions and critical focuses a nurse undertakes to address a patient's health needs, manage their condition, and ensure optimal outcomes. These interventions are grounded in evidence-based practices and align with the nursing process, encompassing assessment, patient education, safety measures, and emergency management. Priorities guide nurses in identifying and addressing the most critical issues first, such as life-threatening conditions or acute complications.
Components of Nursing Interventions and Priorities
Assessment:
Monitor vital signs and laboratory values (e.g., glucose, calcium, TSH, cortisol).
Observe for signs of hormone imbalances (e.g., tachycardia in hyperthyroidism, lethargy in hypothyroidism).
Patient Education:
Importance of medication adherence (e.g., insulin, levothyroxine).
Diet and lifestyle changes for diabetes management.
Signs and symptoms of complications to report (e.g., DKA, Addisonian crisis).
Safety:
Ensure airway patency during thyroid storm or severe hypocalcemia.
Prevent falls in patients with bone demineralization or muscle weakness.
Emergency Management:
DKA: IV insulin, fluid replacement, electrolyte monitoring.
Addisonian Crisis: IV steroids, aggressive fluid replacement.
Thyroid Storm: Antithyroid medications, cooling measures.
Examples
Example 1: Management of Diabetic Ketoacidosis (DKA)
A 45-year-old client with Type 1 diabetes mellitus is admitted to the emergency department with severe abdominal pain, nausea, and vomiting. The nurse notes fruity breath, Kussmaul respirations, and a blood glucose level of 450 mg/dL. Management focuses on initiating IV insulin, administering fluids to correct dehydration, and monitoring electrolytes. NCLEX questions may test your knowledge of prioritizing interventions, recognizing complications such as hypokalemia, and understanding the pathophysiology of DKA.
Example 2: Thyroid Storm in Hyperthyroidism
A 30-year-old female with untreated Graves’ disease presents with fever, tachycardia, and agitation. The client is diagnosed with thyroid storm, a life-threatening emergency. Nursing care includes administering antithyroid medications (e.g., propylthiouracil), beta-blockers to control heart rate, and implementing cooling measures. On the NCLEX, this scenario could involve identifying clinical signs of thyroid storm, prioritizing care, and patient education regarding medication adherence.
Example 3: Cushing’s Syndrome Complications
A 50-year-old client with a history of corticosteroid use for autoimmune disease presents with moon face, truncal obesity, purple striae, and hypertension. The NCLEX might ask about the nurse's role in managing hyperglycemia, preventing infections, and providing education on gradual tapering of corticosteroids. Questions may also test your ability to identify complications such as osteoporosis and impaired wound healing.
Example 4: Addisonian Crisis
A 60-year-old male with Addison’s disease arrives in the hospital with severe fatigue, hypotension, and hyperpigmentation of the skin. During the crisis, immediate interventions include administering IV hydrocortisone and saline to correct hypotension and electrolyte imbalances. NCLEX questions may focus on recognizing early signs of adrenal insufficiency, understanding the importance of stress-dose steroids, and client education about carrying emergency steroid injections.
Example 5: Management of Hypoparathyroidism
A 35-year-old client undergoing thyroidectomy develops tingling in the fingers and a positive Chvostek's sign, indicating hypocalcemia due to accidental removal of the parathyroid glands. Management includes calcium gluconate IV, oral calcium supplements, and vitamin D. NCLEX questions may evaluate your knowledge of electrolyte imbalances, nursing interventions for hypocalcemia, and educating the client about long-term calcium and vitamin D therapy.
Practice Questions
Question 1
A client with diabetes mellitus is admitted with confusion, diaphoresis, and tremors. The nurse checks the client’s blood glucose level, which is 50 mg/dL. What is the priority nursing action?
A. Administer 50% dextrose intravenously.
B. Provide a glass of orange juice with sugar.
C. Prepare to administer glucagon intramuscularly.
D. Call the healthcare provider.
Answer: B
Explanation:
The client’s symptoms indicate hypoglycemia, confirmed by a blood glucose level of 50 mg/dL.
Oral glucose (e.g., orange juice) is the priority for a conscious client who can safely swallow, as it is the fastest way to increase blood glucose.
50% dextrose (IV) or glucagon (IM) are used for clients who are unconscious or unable to swallow.
Calling the healthcare provider is not the priority in this acute situation.
Question 2
A client with hyperthyroidism is experiencing palpitations, a temperature of 104°F (40°C), and confusion. The nurse suspects thyroid storm. Which intervention should the nurse perform first?
A. Administer acetaminophen.
B. Administer beta-blockers.
C. Ensure a patent airway.
D. Start intravenous fluids.
Answer: C
Explanation:
Thyroid storm is a life-threatening emergency requiring immediate interventions.
Airway management is the first priority in any critical condition to maintain oxygenation.
Beta-blockers (e.g., propranolol) help manage tachycardia, but only after airway is ensured.
Acetaminophen can reduce fever, but it is not the priority.
IV fluids support circulation but are secondary to airway and breathing.
Question 3
The nurse is caring for a client with Addison's disease who suddenly develops severe hypotension, confusion, and abdominal pain. What should the nurse do first?
A. Administer hydrocortisone IV.
B. Infuse 0.9% normal saline rapidly.
C. Check blood glucose levels.
D. Draw blood for serum cortisol levels.
Answer: A
Explanation:
The client is likely experiencing Addisonian crisis, a life-threatening condition caused by acute adrenal insufficiency.
The priority is IV hydrocortisone to replace deficient corticosteroids and stabilize the client.
Rapid IV fluids (e.g., 0.9% normal saline) can help manage hypotension but are secondary to corticosteroid replacement.
Checking blood glucose levels is important but not the first priority.
Drawing blood for cortisol levels can confirm the diagnosis but is not urgent in an acute crisis.