Ethical and legal principles are integral to nursing practice, ensuring patient safety, rights, and quality care. Nurses must navigate ethical dilemmas while adhering to legal frameworks that guide their professional responsibilities. Key ethical principles, such as autonomy, beneficence, and justice, combine with legal mandates like informed consent, HIPAA, and malpractice laws to shape safe and ethical care delivery. Mastery of these concepts is essential for success on the NCLEX RN® and for upholding nursing professionalism and integrity.
Learning Objectives
In studying "Fundamentals: Ethical/Legal" for the NCLEX RN® Exam, you should learn to understand the core ethical principles such as autonomy, beneficence, nonmaleficence, justice, and fidelity, and their application in nursing practice. Analyze key legal concepts, including informed consent, confidentiality (HIPAA), advance directives, and standards of care. Evaluate scenarios involving legal safeguards like mandated reporting, malpractice, and appropriate delegation. Explore how ethical and legal principles guide decision-making, patient advocacy, and professional accountability. Apply this understanding to interpreting patient care scenarios and ethical dilemmas presented in NCLEX-style questions to ensure safe and competent nursing practice.
Key Concepts in Ethical/Legal Nursing
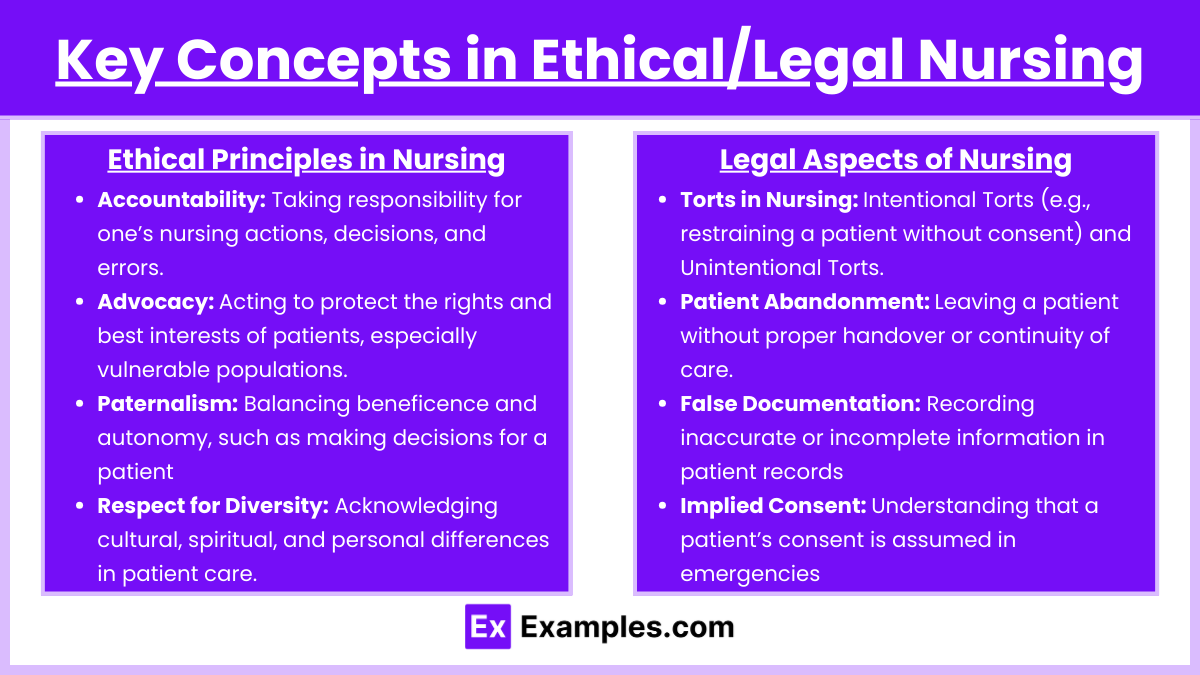
1. Ethical Principles in Nursing
Accountability: Taking responsibility for one’s nursing actions, decisions, and errors.
Advocacy: Acting to protect the rights and best interests of patients, especially vulnerable populations.
Paternalism: Balancing beneficence and autonomy, such as making decisions for a patient when they cannot.
Respect for Diversity: Acknowledging cultural, spiritual, and personal differences in patient care.
Examples of Ethical Principles in Practice:
Respecting a patient's decision to refuse life-saving surgery due to religious beliefs (Autonomy).
Providing pain management to alleviate suffering for a terminally ill patient (Beneficence).
Refusing to administer a medication with known harmful side effects unless benefits outweigh the risks (Nonmaleficence).
2. Legal Aspects of Nursing
Torts in Nursing:
Intentional Torts: Actions like assault, battery, and false imprisonment (e.g., restraining a patient without consent).
Unintentional Torts: Acts of negligence or malpractice leading to harm.
Patient Abandonment: Leaving a patient without proper handover or continuity of care.
False Documentation: Recording inaccurate or incomplete information in patient records, which can lead to legal consequences.
Implied Consent: Understanding that a patient’s consent is assumed in emergencies when they cannot communicate.
Examples of Legal Aspects in Practice:
Ensuring that patient care meets standards outlined by state nursing boards (Standards of Care).
Maintaining patient confidentiality by not discussing patient details in public spaces (Confidentiality).
Ethical Theories Relevant to Nursing
Deontology: Duty-based ethics; focuses on the nurse's obligations.
Utilitarianism: Outcome-focused ethics; aims for the greatest good for the greatest number.
Virtue Ethics: Emphasizes the character of the nurse, such as compassion and honesty.
Ethics of Care: Emphasizes interpersonal relationships and the importance of empathy, compassion, and communication in nursing practice.
Justice-Based Ethics: Focuses on equity, particularly when allocating limited resources.
Principlism: Combines multiple ethical principles to resolve complex dilemmas.
Legal Safeguards for Nurses
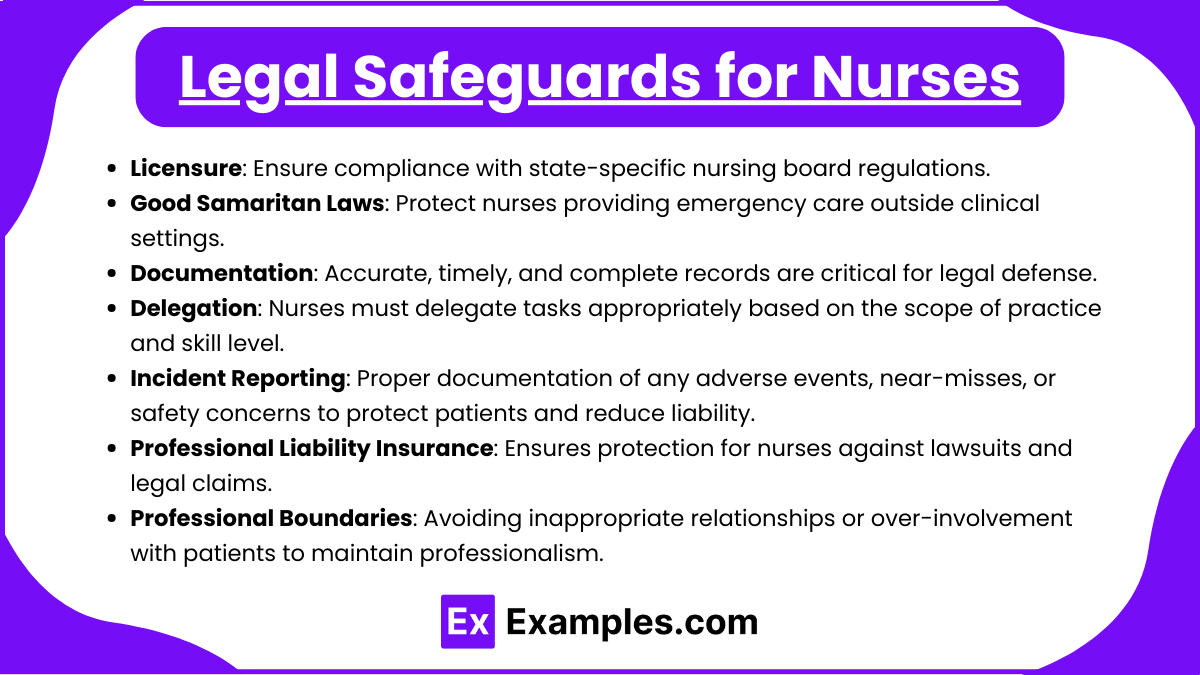
Licensure: Ensure compliance with state-specific nursing board regulations.
Good Samaritan Laws: Protect nurses providing emergency care outside clinical settings.
Documentation: Accurate, timely, and complete records are critical for legal defense.
Delegation: Nurses must delegate tasks appropriately based on the scope of practice and skill level.
Incident Reporting: Proper documentation of any adverse events, near-misses, or safety concerns to protect patients and reduce liability.
Professional Liability Insurance: Ensures protection for nurses against lawsuits and legal claims.
Professional Boundaries: Avoiding inappropriate relationships or over-involvement with patients to maintain professionalism.
Common Ethical Dilemmas in Nursing

Cultural Competency:
Providing culturally appropriate care when cultural practices conflict with medical advice.
Example: A patient refusing blood transfusions due to religious beliefs.
Technology in Care:
Balancing privacy concerns with the increasing use of electronic health records and telehealth.
Example: Protecting patient data from cybersecurity threats while ensuring accessibility to authorized healthcare providers.
Allocation of Scarce Resources:
Ethical considerations in prioritizing patients during crises (e.g., organ transplantation or pandemic triage).
Example: Deciding which critically ill patient receives the last available ICU bed.
Nurse-Physician Conflicts:
Resolving disagreements about patient care plans.
Example: A nurse advocating for additional diagnostic tests that the physician initially declines.
Examples
Example 1. Informed Consent
A nurse witnesses a patient signing an informed consent form for surgery. The nurse ensures the patient understands the procedure, risks, benefits, and alternatives explained by the physician. If the patient expresses confusion or hesitancy, the nurse advocates for further clarification from the physician before proceeding. This demonstrates ethical responsibility (autonomy) and legal obligation in securing informed consent.
Example 2. Confidentiality and HIPAA Compliance
A nurse overhears a coworker discussing a patient’s diagnosis in a public area. The nurse reminds the coworker about the importance of maintaining patient confidentiality under HIPAA regulations. If necessary, the nurse reports the violation to the appropriate supervisor. This example reflects adherence to legal safeguards for patient privacy and the ethical principle of fidelity.
Example 3. Delegation and Accountability
An RN delegates a task, such as measuring vital signs, to an unlicensed assistive personnel (UAP). The RN ensures the UAP is qualified to perform the task and provides clear instructions. The RN also monitors the task’s completion and intervenes if necessary. This illustrates ethical accountability and compliance with legal standards of care in delegation.
Example 4. End-of-Life Care Decisions
A terminally ill patient has a living will that specifies "Do Not Resuscitate" (DNR) orders. The nurse supports the patient’s autonomy by respecting their advance directive, even if family members request interventions. The nurse also ensures documentation is updated to reflect the patient’s wishes. This scenario showcases ethical principles (autonomy and beneficence) and legal obligations related to end-of-life care.
Example 5. Reporting Abuse
During an assessment, a nurse observes signs of physical abuse in a child, including unexplained bruises and fear of a caregiver. The nurse follows mandatory reporting laws by notifying child protective services and documenting the findings objectively. This reflects the nurse’s ethical duty to protect vulnerable populations and comply with legal requirements for mandated reporting.
Practice Questions
Question 1
A patient with terminal cancer refuses additional chemotherapy and states, "I just want to live the rest of my life comfortably." Which ethical principle is the nurse upholding by respecting this decision?
A. Beneficence
B. Nonmaleficence
C. Justice
D. Autonomy
Answer: D. Autonomy
Explanation:
Autonomy refers to respecting the patient’s right to make decisions about their own healthcare, even if the nurse or healthcare provider does not agree with those decisions. In this scenario, the nurse respects the patient’s wish to decline further chemotherapy, upholding their autonomy.
Beneficence involves actions that promote the patient’s well-being, such as offering palliative care to relieve suffering.
Nonmaleficence focuses on avoiding harm; while important, it is not the primary principle here.
Justice relates to fairness and equitable resource allocation, which does not apply in this scenario.
Question 2
Which action by a nurse could result in a charge of negligence?
A. Administering a prescribed medication that causes an allergic reaction.
B. Forgetting to raise the side rails on a patient’s bed, leading to a fall.
C. Not informing a patient about the risks of a surgical procedure.
D. Disclosing confidential patient information to an unauthorized family member.
Answer: B. Forgetting to raise the side rails on a patient’s bed, leading to a fall.
Explanation:
Negligence occurs when a nurse fails to perform a duty or takes an action below the standard of care, resulting in harm to the patient. Forgetting to raise side rails is a clear breach of standard care that can lead to injury.
Administering a prescribed medication that causes an allergic reaction does not constitute negligence if the nurse followed proper procedures and verified the patient’s allergies beforehand.
Not informing a patient about surgical risks is typically the physician's responsibility, not the nurse's, unless delegated.
Disclosing confidential information violates HIPAA but falls under legal breaches, not negligence specifically.
Question 3
A patient arrives in the emergency department unconscious. No family members are present, and urgent surgery is required. What type of consent applies in this situation?
A. Implied consent
B. Informed consent
C. Written consent
D. Verbal consent
Answer: A. Implied consent
Explanation:
Implied consent is assumed when a patient is unable to give consent, and immediate medical intervention is necessary to preserve life or prevent harm. In this case, the unconscious state and urgency of the surgery warrant implied consent.
Informed consent requires the patient to be fully informed of risks, benefits, and alternatives and to give consent voluntarily; this is not possible when the patient is unconscious.
Written consent is a formal agreement typically used for elective or planned procedures, which is not applicable in emergencies.
Verbal consent requires a conscious patient who can provide spoken agreement, which is not possible here.