Leadership and management in nursing require a thorough understanding of ethical and legal principles to ensure safe, patient-centered care. Ethical principles, such as autonomy, beneficence, and justice, guide nurses in decision-making, while legal principles, including informed consent, confidentiality, and accountability, ensure compliance with laws protecting patients and healthcare providers. On the NCLEX-RN®, nurses must demonstrate their ability to navigate complex ethical dilemmas and adhere to legal standards, ensuring professionalism, patient safety, and adherence to the Nurse Practice Act and institutional policies.
Learning Objectives
In studying "Leadership & Management: Ethical/Legal" for the NCLEX-RN® exam, you should learn to understand the ethical principles of autonomy, beneficence, non-maleficence, justice, fidelity, and veracity, as well as legal concepts like informed consent, confidentiality, negligence, and malpractice. Analyze how these principles guide decision-making, patient advocacy, and accountability in nursing practice. Evaluate scenarios involving end-of-life care, informed consent, and delegation to ensure compliance with ethical standards and legal requirements. Additionally, explore how these principles impact patient rights, safety, and communication, and apply your understanding to prioritizing and resolving ethical/legal dilemmas in NCLEX-style practice questions.
Key Concepts of Ethical/Legal Principles in Nursing
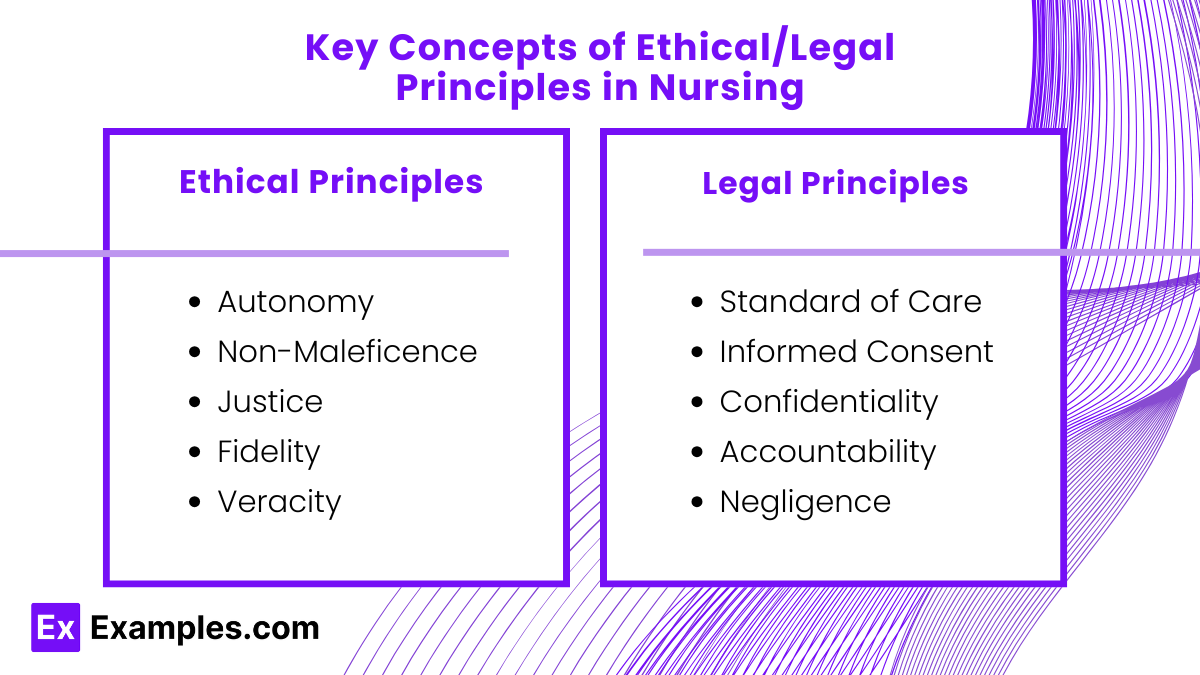
1. Ethical Principles
Nursing ethics focus on providing care that respects patient autonomy, promotes beneficence, and upholds justice.
Autonomy: Respecting the patient’s right to make decisions about their care.
Beneficence: Acting in the best interest of the patient by promoting their well-being.
Non-Maleficence: Avoiding harm to the patient.
Justice: Providing fair and equal treatment to all patients.
Fidelity: Being faithful to commitments, promises, and responsibilities.
Veracity: Being honest and truthful in communication with patients.
2. Legal Principles
Legal concepts in nursing ensure compliance with laws that protect patients, healthcare providers, and institutions.
Standard of Care: The minimum acceptable level of care based on evidence and guidelines.
Informed Consent: Ensuring patients understand and agree to procedures after being informed of risks, benefits, and alternatives.
Confidentiality: Protecting patient information as mandated by the Health Insurance Portability and Accountability Act (HIPAA).
Accountability: Taking responsibility for nursing actions and decisions.
Negligence: Avoiding actions that deviate from the standard of care and cause harm to patients.
Application of Ethical and Legal Principles in Leadership
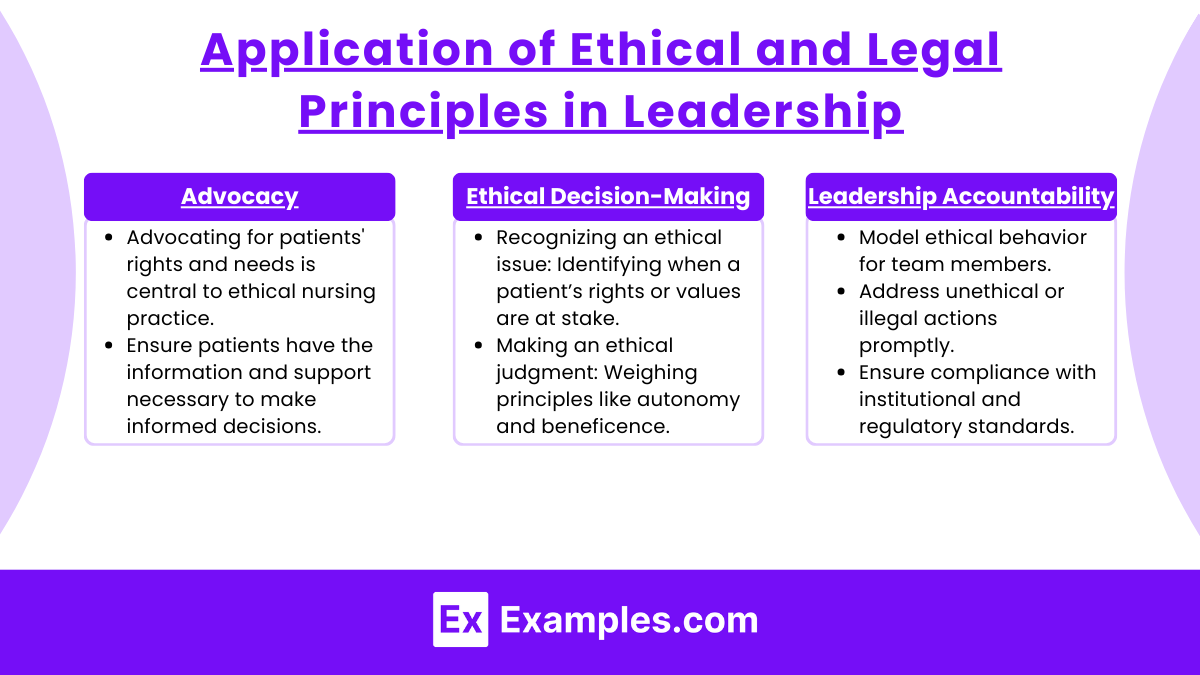
1. Advocacy
Advocating for patients' rights and needs is central to ethical nursing practice.
Ensure patients have the information and support necessary to make informed decisions.
2. Ethical Decision-Making
Use ethical frameworks, such as the Four-Component Model:
Recognizing an ethical issue: Identifying when a patient’s rights or values are at stake.
Making an ethical judgment: Weighing principles like autonomy and beneficence.
Prioritizing ethical intentions: Acting in the patient’s best interest.
Taking action: Implementing decisions based on ethical reasoning.
3. Leadership Accountability
As leaders, nurses must:
Model ethical behavior for team members.
Address unethical or illegal actions promptly.
Ensure compliance with institutional and regulatory standards.
Common Ethical/Legal Scenarios

1. End-of-Life Care
Respect patient decisions regarding advance directives and Do-Not-Resuscitate (DNR) orders.
Address family disagreements with empathy and clarity.
2. Informed Consent
Ensure patients understand the procedure, its risks, and benefits.
Verify that the consent is voluntary and provided by a competent individual.
3. Confidentiality Breaches
Report incidents where patient information is improperly shared.
Safeguard medical records to comply with HIPAA standards.
4. Delegation and Accountability
Delegate tasks appropriately while retaining accountability for patient outcomes.
Avoid delegating responsibilities outside a team member's scope of practice.
5. Handling Medication Errors
Acknowledge errors immediately and take corrective actions.
Document incidents truthfully and implement measures to prevent recurrence.
Examples
Example 1. Patient Autonomy vs. Family Wishes
A patient with advanced cancer decides to discontinue chemotherapy, choosing comfort care instead. The family strongly disagrees and demands continued treatment. The nurse must respect the patient’s autonomy while communicating empathetically with the family. The correct action includes ensuring the patient is fully informed about their decision and advocating for their rights while managing the family’s emotional response.
Example 2. Handling Informed Consent
A patient scheduled for surgery expresses confusion about the procedure during pre-operative preparations. The nurse realizes that the surgeon has not explained the risks and benefits in detail. Legally and ethically, the nurse must halt the process and request the surgeon to provide additional information. This ensures the patient gives informed consent, a fundamental patient right and legal requirement.
Example 3. Confidentiality and HIPAA Compliance
A nurse overhears a colleague discussing a patient’s condition in a hospital elevator. This action violates HIPAA regulations and patient confidentiality. The nurse’s ethical and legal responsibility is to address the colleague directly and report the breach to the appropriate supervisor. Ensuring confidentiality not only complies with the law but also maintains trust in the healthcare system.
Example 4. Delegation and Accountability
An RN delegates vital sign monitoring for a stable patient to a UAP. Later, the nurse discovers that the UAP failed to report a significant change in the patient’s condition. While the task was appropriately delegated, the RN remains legally and ethically accountable for supervising and following up on delegated tasks. The nurse must document the incident, evaluate the delegation process, and provide guidance to the UAP.
Example 5. Addressing End-of-Life Decisions
A terminally ill patient has a valid Do-Not-Resuscitate (DNR) order, but during a cardiac arrest, a family member insists on resuscitation. The nurse’s ethical duty is to follow the DNR order, ensuring the patient’s wishes are honored. The legal responsibility includes documenting the event accurately and notifying the healthcare provider. The nurse should also provide emotional support to the family and explain the importance of respecting the patient’s autonomy.
Practice Questions
Question 1
A patient diagnosed with terminal cancer refuses further treatment. The family insists on continuing all possible interventions. As the nurse, what is your best course of action?
A. Respect the family's wishes and encourage treatment continuation.
B. Notify the healthcare provider to convince the patient to accept treatment.
C. Respect the patient’s decision and advocate for their autonomy.
D. Ask the hospital ethics committee to intervene immediately.
Answer: C. Respect the patient’s decision and advocate for their autonomy.
Explanation: The principle of autonomy states that patients have the right to make decisions about their own care, even if their choices conflict with the opinions of their family or healthcare team. Nurses have an ethical duty to respect and advocate for patients' decisions.
A is incorrect because it disregards the patient’s autonomy.
B is incorrect because the nurse's role is not to pressure patients into accepting care but to ensure informed decision-making.
D is incorrect because involving the ethics committee is unnecessary unless there is a legal or ethical conflict that cannot be resolved through communication.
Question 2
A nurse accidentally administers the wrong medication to a patient but notes no immediate adverse effects. What is the first action the nurse should take?
A. Document the error in the patient’s chart and report it to the supervisor.
B. Inform the patient that a medication error occurred and provide reassurance.
C. Notify the prescribing healthcare provider and monitor the patient for side effects.
D. Complete an incident report and keep it in the patient’s medical record.
Answer: C. Notify the prescribing healthcare provider and monitor the patient for side effects.
Explanation: The nurse must first ensure patient safety by notifying the healthcare provider and monitoring for adverse effects. This allows prompt intervention if necessary.
A is incorrect because documenting the error in the patient’s chart before taking action does not prioritize patient safety.
B is incorrect because while informing the patient is part of transparency, it is not the priority.
D is incorrect because incident reports are not placed in the patient’s medical record; they are part of quality improvement efforts and legal documentation.
Question 3
A nurse witnesses a colleague posting details about a patient’s condition on social media, but no identifiers are used. What is the most appropriate initial action?
A. Confront the colleague and demand the post be removed immediately.
B. Report the post to the nurse manager or supervisor.
C. Ignore the post since no identifying information was included.
D. Discuss social media policies with the colleague at a later time.
Answer: B. Report the post to the nurse manager or supervisor.
Explanation: Even if no identifiers are included, discussing a patient’s condition on social media violates HIPAA and professional nursing standards. Reporting the incident to the nurse manager ensures it is addressed appropriately and prevents further violations.
A is incorrect because while addressing the colleague is an option, it does not ensure the issue is resolved or reported.
C is incorrect because HIPAA violations are not dependent on the inclusion of identifying information; discussing patient details in any form is a breach.
D is incorrect because delaying the discussion allows for potential continued violations.