The gastrointestinal (GI) system plays a vital role in digestion, nutrient absorption, and waste elimination, supporting overall health. It includes organs like the stomach, intestines, liver, and pancreas, all working to ensure the body receives essential nutrients. Nutrition, closely tied to GI function, is critical for energy, growth, and tissue repair. Disorders such as GERD, Crohn’s disease, and malabsorption can disrupt this balance. Nursing care focuses on managing symptoms, promoting optimal nutrition, and preventing complications to improve patient outcomes.
Learning Objectives
In studying “Adult Health: Gastrointestinal/Nutrition” for the NCLEX-RN® Exam, you should learn to understand the anatomy, physiology, and common pathophysiological conditions of the gastrointestinal system. Analyze the role of nutrition in health and disease, including the principles of enteral and parenteral nutrition. Evaluate nursing interventions for conditions like GERD, PUD, IBD, and pancreatitis. Explore the use of pharmacological and non-pharmacological strategies to manage symptoms and complications. Apply your knowledge to prioritize nursing care, educate patients on dietary modifications, and interpret clinical findings. Additionally, practice applying these concepts to NCLEX-style questions to develop critical thinking and clinical reasoning skills.
Overview of the Gastrointestinal System
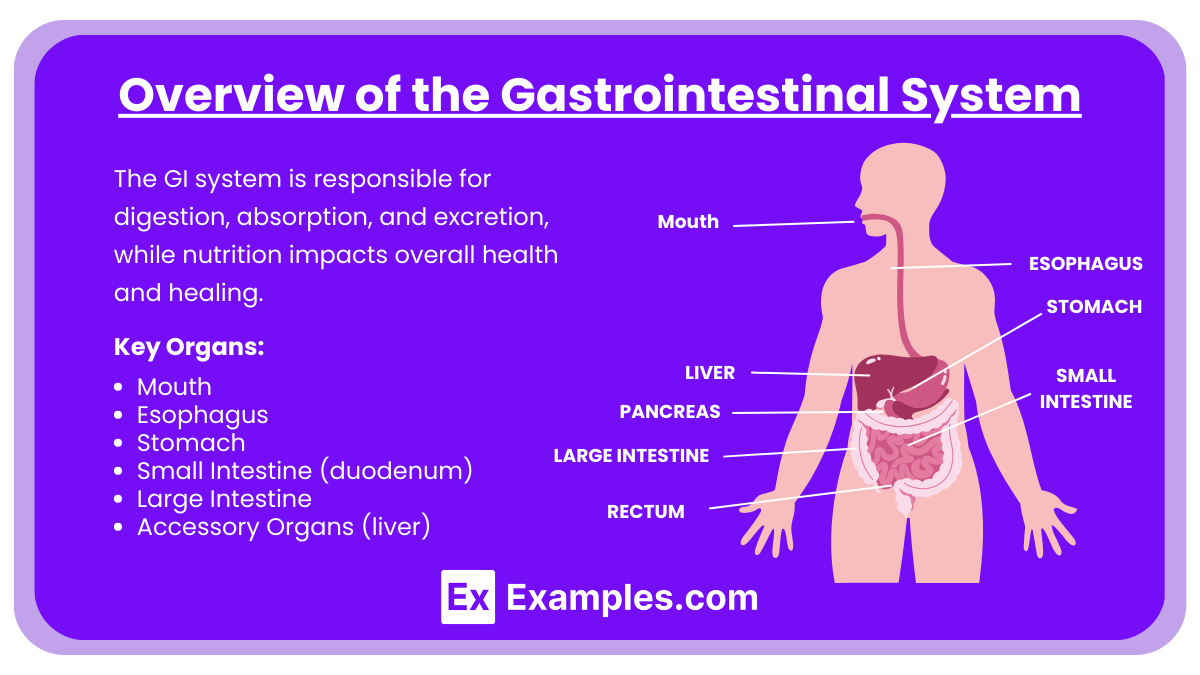
The GI system is responsible for digestion, absorption, and excretion, while nutrition impacts overall health and healing. As a nurse, understanding disease processes, clinical manifestations, diagnostic tests, and nursing interventions is crucial. The gastrointestinal (GI) system is responsible for:
- Digestion: Breaking down food into absorbable nutrients.
- Absorption: Transferring nutrients into the bloodstream.
- Excretion: Elimination of waste products.
Key Organs:
- Mouth
- Esophagus
- Stomach
- Small Intestine (duodenum, jejunum, ileum)
- Large Intestine
- Accessory Organs (liver, pancreas, gallbladder)
Disorders of the GI System
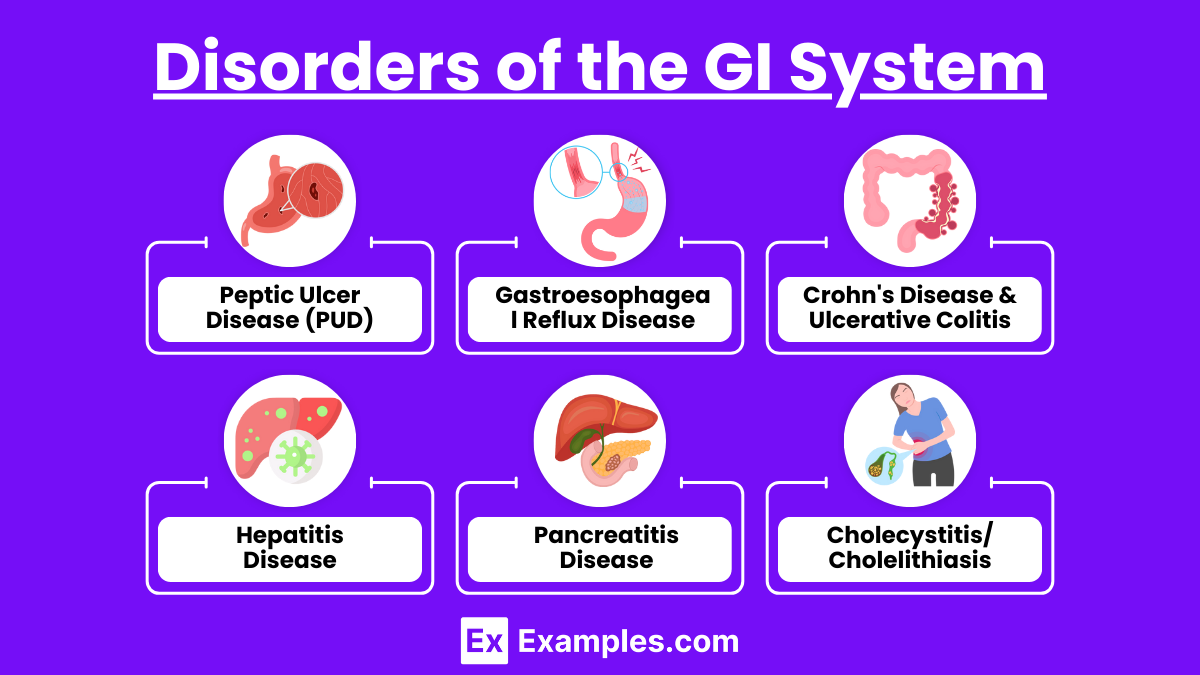
- Peptic Ulcer Disease (PUD)
- Causes: H. pylori infection, NSAIDs, stress.
- Symptoms: Epigastric pain, nausea, vomiting, melena.
- Interventions: Administer proton pump inhibitors (PPIs), antibiotics for H. pylori, and antacids. Educate on lifestyle changes, including avoiding spicy foods, caffeine, and alcohol.
- Gastroesophageal Reflux Disease (GERD)
- Causes: Weak LES (lower esophageal sphincter), obesity, smoking.
- Symptoms: Heartburn, regurgitation, dysphagia.
- Interventions: Advise small frequent meals, elevate head of bed, avoid triggers (caffeine, chocolate). Medications: Antacids, H2 blockers, PPIs.
- Crohn’s Disease & Ulcerative Colitis (Inflammatory Bowel Diseases)
- Crohn’s: Skip lesions, affects mouth to anus, transmural.
- Ulcerative Colitis: Continuous lesions, confined to the colon.
- Interventions: Encourage low-residue diets during flares, administer corticosteroids, immunosuppressants, and biologics.
- Hepatitis Disease
- Types: A, B, C, D, E.
- Symptoms: Jaundice, dark urine, fatigue, abdominal pain.
- Interventions: Supportive care, antiviral medications (for chronic hepatitis), educate on hygiene and vaccination.
- Pancreatitis Disease
- Acute: Gallstones, alcohol use.
- Chronic: Alcohol use, cystic fibrosis.
- Symptoms: Severe epigastric pain radiating to back, nausea, vomiting, elevated amylase/lipase.
- Interventions: NPO, pain management, IV fluids, low-fat diet post-recovery.
- Cholecystitis/Cholelithiasis
- Causes: Gallstones, bile stasis.
- Symptoms: RUQ pain, Murphy’s sign, nausea after fatty meals.
- Interventions: NPO, administer antibiotics, cholecystectomy.
Common Diagnostic Tests
- Endoscopy (EGD, colonoscopy): Endoscopy is a critical diagnostic tool for direct visualization of the gastrointestinal tract. Esophagogastroduodenoscopy (EGD) evaluates the esophagus, stomach, and duodenum, while colonoscopy examines the colon and rectum. These procedures are instrumental in identifying GERD, ulcers, Crohn’s disease, Barrett’s esophagus, colorectal cancer, and other conditions. They enable biopsies for histopathology and therapeutic interventions like polyp removal or stricture dilation. Patients undergo sedation during the procedure.
- Abdominal Ultrasound: Abdominal Ultrasound uses high-frequency sound waves to detect abnormalities like gallstones, fatty liver, liver cysts, and tumors. It is also effective in assessing ascites and other structural anomalies in organs like the liver, gallbladder, pancreas, and kidneys. The procedure involves moving a transducer over the abdomen with an applied gel to produce images. Fasting is often required to enhance visualization of certain organs. Ultrasound is advantageous due to its safety during pregnancy and lack of radiation exposure, though its effectiveness can be limited in obese individuals or those with significant bowel gas.
- CT Scan/MRI: CT Scan and MRI provide highly detailed imaging for diagnosing gastrointestinal disorders. CT scans are invaluable for identifying tumors, abscesses, blockages, perforations, and inflammation with cross-sectional images. MRI offers superior soft tissue contrast, making it ideal for liver lesions, pancreatic masses, and bile duct evaluations through Magnetic Resonance Cholangiopancreatography (MRCP). Both tests may require oral or IV contrast agents for enhanced visualization. Patients must remain still during the procedure, and MRI requires additional preparation, such as removing metal objects due to the magnetic field.
- Stool Studies: Stool Studies play a crucial role in diagnosing infections, parasites, blood, and inflammatory markers in the gastrointestinal tract. These tests include fecal occult blood testing (FOBT) for detecting hidden blood and stool cultures to identify pathogenic bacteria or parasites. They are non-invasive and provide essential information for conditions like gastrointestinal infections, inflammatory bowel disease, and colorectal cancer screening. Proper sample collection and transport are necessary to ensure accurate results.
- Serum Labs: Amylase, lipase, liver enzymes (ALT, AST, ALP), bilirubin. Serum Laboratory Tests are essential for evaluating enzyme levels and liver function. Amylase and lipase are critical markers for diagnosing pancreatitis. Liver enzymes, including ALT, AST, and ALP, assess hepatic function and detect liver injury or disease. Bilirubin levels help evaluate jaundice and biliary obstruction. These tests provide a biochemical snapshot of organ function and are often used alongside imaging for comprehensive evaluation.
Nutritional Concepts
- Enteral Nutrition : Enteral nutrition involves delivering nutrients directly into the gastrointestinal (GI) tract via a feeding tube. It is preferred over parenteral nutrition when the GI tract is functional.
- Indications: Swallowing issues, unconscious clients.
- Nursing Interventions: Verify tube placement (X-ray, pH test), maintain patency, assess residual volumes, prevent aspiration.
- Parenteral Nutrition (TPN) : Parenteral nutrition involves intravenous delivery of nutrients when the GI tract is nonfunctional.
- Indications: Non-functional GI tract, severe malnutrition.
- Nursing Interventions: Monitor blood glucose, prevent infection, assess for electrolyte imbalances.
- Special Diets : Special diets are tailored to meet the unique nutritional needs of individuals based on their health conditions
- Low-residue diet: A low-residue diet is designed to reduce bowel activity and is commonly recommended for individuals with inflammatory bowel disease (IBD) during flares, diverticulitis, or post-GI surgery. This diet includes easily digestible foods like white rice, refined cereals, tender meats, and dairy, while avoiding high-fiber foods like whole grains, nuts, and raw vegetables.
- High-protein, high-calorie:A high-protein, high-calorie diet supports tissue repair and energy needs, making it essential for patients recovering from wounds, surgery, or conditions like cancer, burns, and sepsis. Foods such as eggs, poultry, fish, nuts, and dairy are encouraged.
- Low-fat diet: Gallbladder disease, pancreatitis. A low-fat diet is often prescribed for individuals with gallbladder disease, pancreatitis, or hyperlipidemia. It includes lean meats, low-fat dairy, and skinless poultry while avoiding fried foods, fatty meats, and butter.
- Gluten-free diet: A gluten-free diet is crucial to prevent intestinal damage and includes gluten-free grains like rice, corn, and quinoa, while avoiding wheat, barley, rye, and oats unless certified gluten-free.
Examples
Example 1: Patient with Gastroesophageal Reflux Disease (GERD)
A 45-year-old patient presents with complaints of frequent heartburn, regurgitation, and a chronic cough, particularly after meals. The NCLEX question may ask about nursing interventions such as elevating the head of the bed during sleep, avoiding trigger foods (spicy, acidic, or fatty), and the appropriate use of proton pump inhibitors (PPIs) or H2 receptor blockers. The question might also test the nurse’s knowledge of educating the patient about avoiding eating within three hours of bedtime to prevent acid reflux.
Example 2: Postoperative Care for a Patient with a PEG Tube
A patient recovering from esophageal cancer surgery has a percutaneous endoscopic gastrostomy (PEG) tube placed for long-term enteral feeding. The NCLEX may ask about proper nursing care, including verifying tube placement, flushing the tube with sterile water before and after feedings, maintaining head-of-bed elevation to prevent aspiration, and monitoring for complications such as infection or tube dislodgment. Understanding how to assess residual volumes and implement feeding protocols safely is a key component.
Example 3: Management of a Patient with Acute Pancreatitis
A 60-year-old patient arrives in the emergency department with severe epigastric pain radiating to the back, nausea, and vomiting. Laboratory results show elevated amylase and lipase levels. NCLEX questions might focus on the nurse’s priority actions, such as keeping the patient NPO (nothing by mouth) to rest the pancreas, providing IV fluids for hydration, and administering prescribed pain medications like opioids. The exam may also assess knowledge of dietary modifications, such as a low-fat diet, once the patient can tolerate oral intake.
Example 4: Nutritional Support for a Patient with Inflammatory Bowel Disease (IBD)
A young adult with Crohn’s disease is experiencing an acute flare with diarrhea, abdominal pain, and weight loss. The NCLEX question may address the nurse’s role in ensuring the patient is on a low-residue diet to reduce bowel activity, monitoring for dehydration, and providing enteral nutrition if oral intake is insufficient. Additionally, questions may test the nurse’s knowledge of medication management, including corticosteroids and immunomodulators, and the importance of preventing complications such as strictures or fistulas.
Example 5: Care for a Patient with Celiac Disease
A 35-year-old patient is diagnosed with celiac disease and reports persistent bloating, diarrhea, and fatigue despite eating a “healthy diet.” The NCLEX may include questions on patient education, emphasizing the necessity of a gluten-free diet and avoiding foods containing wheat, barley, and rye. The nurse may also need to educate the patient about cross-contamination prevention, appropriate substitutes like rice and quinoa, and monitoring for secondary complications such as anemia or osteoporosis due to malabsorption.
Practice Questions
Question 1
A client with Crohn’s disease is admitted with severe abdominal pain and diarrhea. The nurse should expect which dietary recommendation during an exacerbation?
A. High-fiber diet
B. Low-residue diet
C. Gluten-free diet
D. Low-fat diet
Answer: B. Low-residue diet
Explanation:
- A low-residue diet minimizes fiber and reduces bowel activity, which helps decrease symptoms like diarrhea and abdominal pain during a Crohn’s disease exacerbation. Foods such as refined grains, lean proteins, and well-cooked vegetables are preferred.
- A high-fiber diet (Option A) would aggravate symptoms by increasing bowel motility.
- A gluten-free diet (Option C) is primarily indicated for clients with celiac disease, not Crohn’s disease.
- A low-fat diet (Option D) is used for conditions like gallbladder disease and pancreatitis but is not specifically recommended for Crohn’s disease flares.
Question 2
The nurse is caring for a client receiving total parenteral nutrition (TPN). Which of the following findings requires immediate intervention?
A. Blood glucose level of 140 mg/dL
B. Redness and warmth at the central line insertion site
C. Daily weight increase of 1.5 pounds
D. Serum potassium level of 4.0 mEq/L
Answer: B. Redness and warmth at the central line insertion site
Explanation:
- Redness and warmth at the central line site suggest a possible infection, such as catheter-related bloodstream infection (CRBSI). This is a priority because infections can lead to sepsis, which is life-threatening and requires immediate intervention.
- A blood glucose level of 140 mg/dL (Option A) is elevated but within an acceptable range for TPN clients. Regular monitoring and insulin adjustments can manage this.
- A daily weight increase of 1.5 pounds (Option C) could indicate fluid retention but is not as critical as a potential infection.
- A serum potassium level of 4.0 mEq/L (Option D) is normal (reference range: 3.5–5.0 mEq/L) and does not require intervention.
Question 3
A client with GERD is being discharged with dietary instructions. Which statement by the client indicates the need for further teaching?
A. “I will avoid spicy foods and chocolate.”
B. “I will eat three large meals each day.”
C. “I will wait at least 2 hours after eating before lying down.”
D. “I will elevate the head of my bed by 6–8 inches while sleeping.”
Answer: B. “I will eat three large meals each day.”
Explanation:
- GERD management includes small, frequent meals to prevent reflux by avoiding overfilling the stomach. Eating three large meals increases the risk of acid reflux and worsens symptoms, indicating the need for further teaching.
- Avoiding spicy foods and chocolate (Option A) is correct because these are common triggers for GERD.
- Waiting at least 2 hours after eating before lying down (Option C) helps reduce the risk of acid reflux, especially at night.
- Elevating the head of the bed (Option D) reduces nighttime reflux by using gravity to prevent stomach contents from moving into the esophagus.